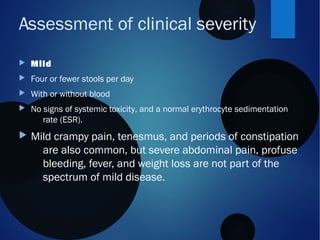
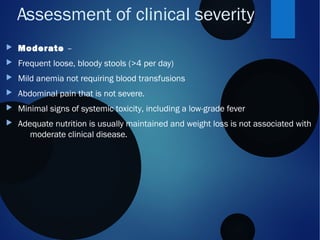
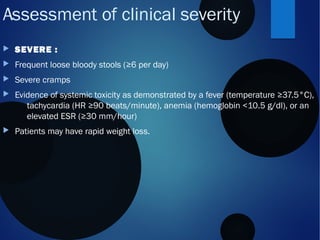
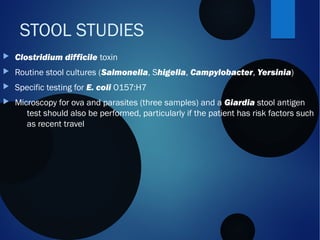
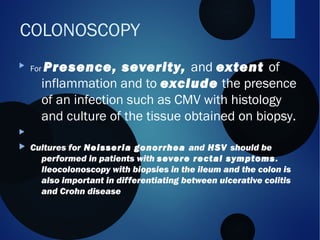
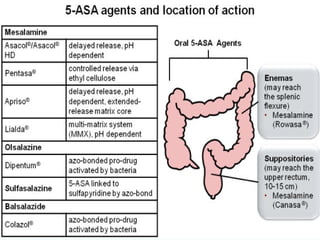
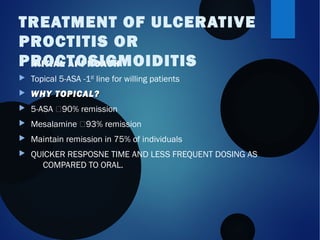
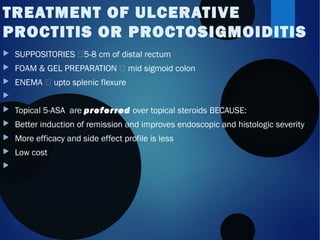
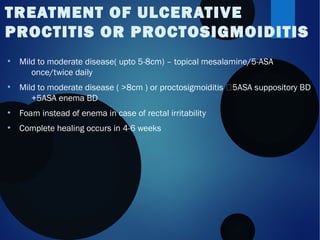
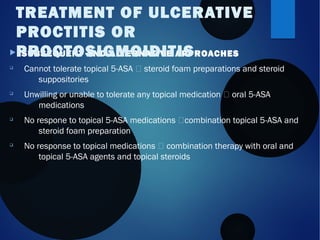
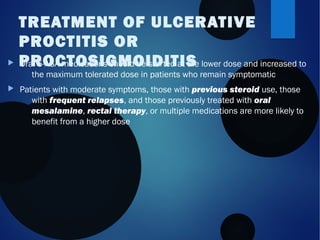
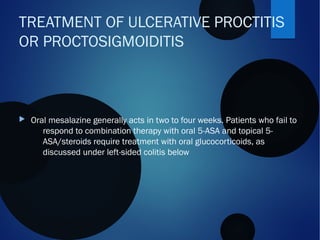
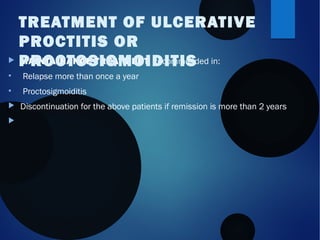
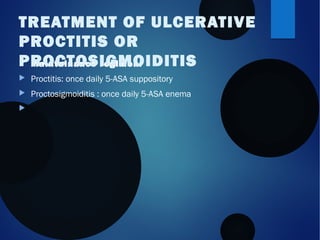
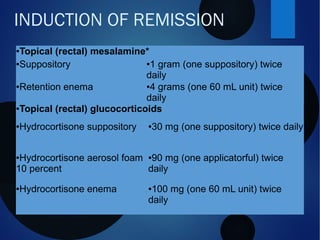
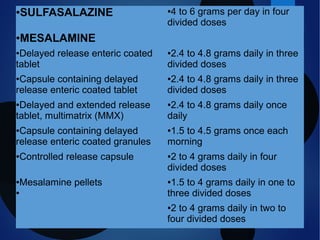
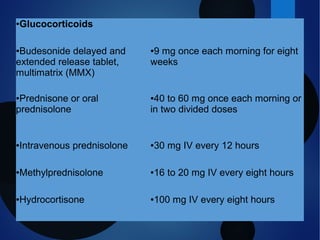
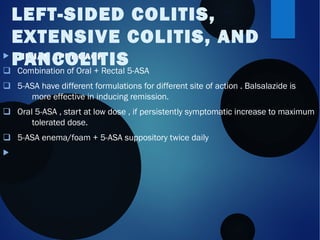
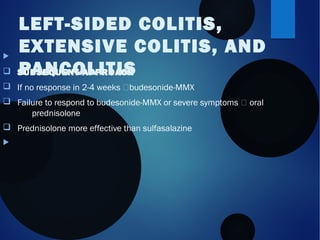
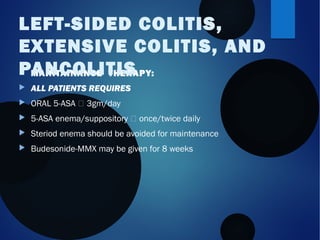
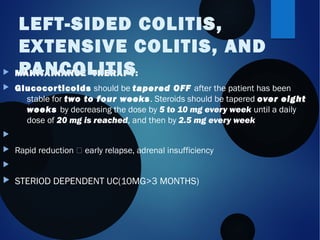
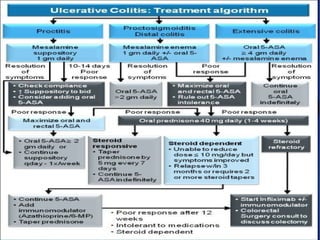
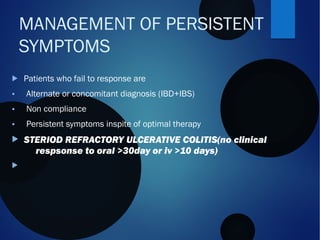
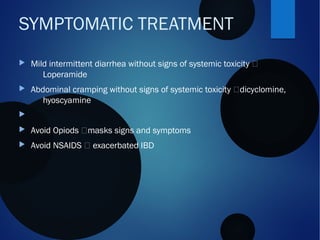
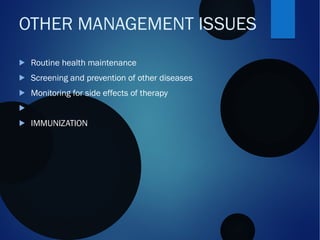
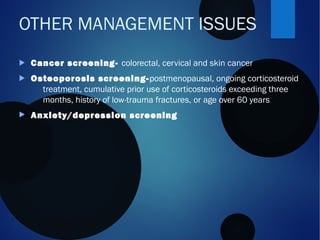
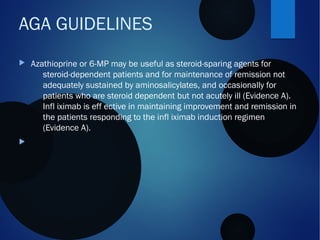
This presentation by Dr. Bhavin Mandowara covers the treatment strategies for mild to moderate ulcerative colitis, including evaluation, management, and symptomatic treatments. It emphasizes the use of topical 5-ASA as a first-line treatment and discusses various approaches for initial, subsequent, and maintenance therapy based on disease severity. Additionally, it outlines the importance of laboratory testing, alternative treatment options, and long-term management considerations.