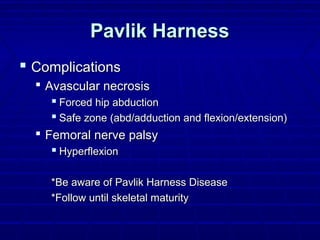
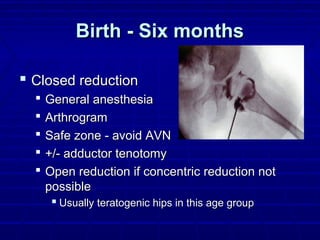
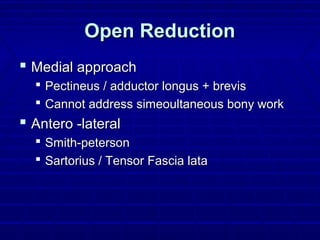
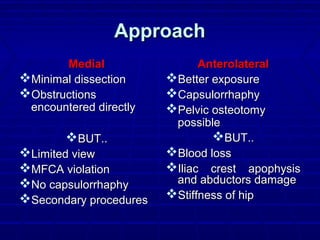
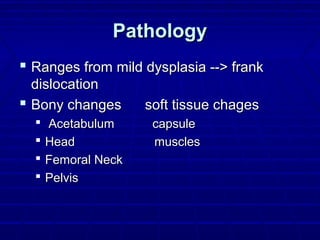
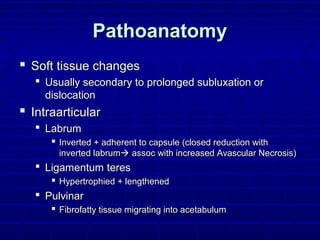
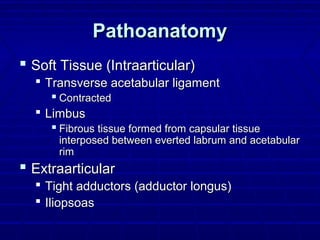
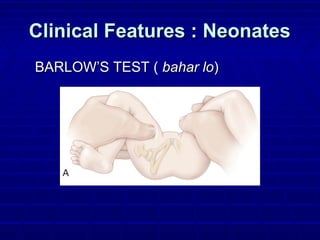
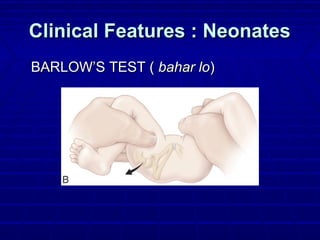
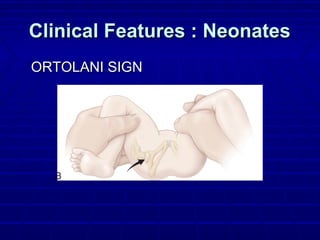
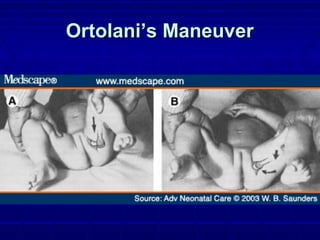
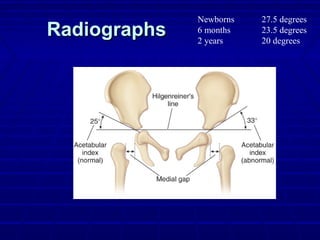
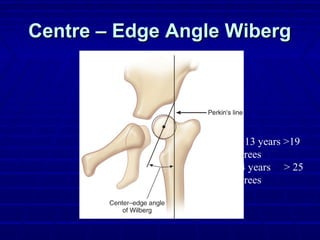
This document provides an overview of developmental dysplasia of the hip (DDH), including its normal development, etiology, epidemiology, diagnosis, treatment, and complications. Key points include: DDH can range from mild dysplasia to frank dislocation and is more common in females. Clinical diagnosis involves the Ortolani and Barlow maneuvers while imaging includes x-rays and ultrasound. Treatment depends on the grade of DDH and may involve closed or open reduction along with bracing or splinting. Complications can include avascular necrosis and osteoarthritis if left untreated.
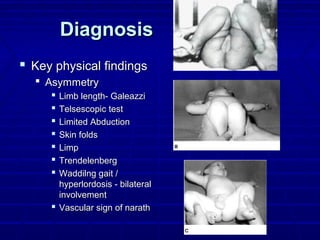
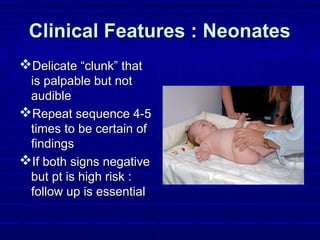
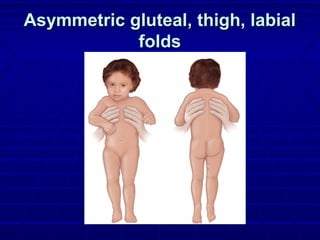
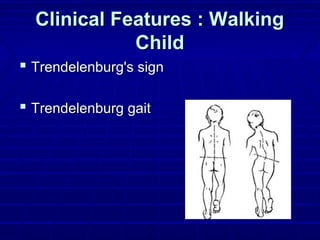
![Walking child:Walking child:
LLDLLD
↓↓AbductionAbduction
Tip-toe-walkingTip-toe-walking
Trendelenberg gaitTrendelenberg gait
Waddling [B/L]Waddling [B/L]
↑↑lumbar lordosislumbar lordosis](https://image.slidesharecdn.com/ddhhardik-130706213206-phpapp01/85/developemental-dysplasia-of-hip-23-320.jpg)



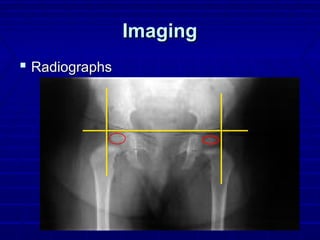
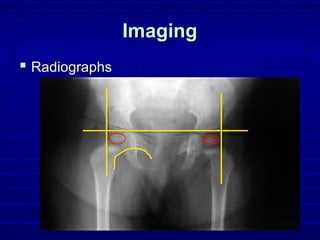


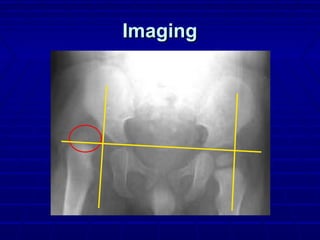
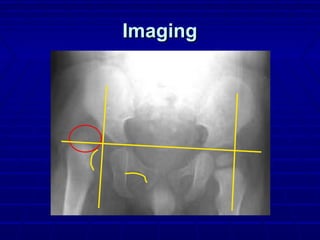
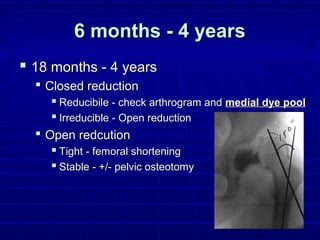
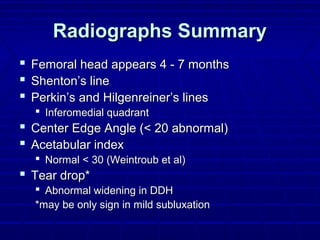
![Tear dropTear drop
AP X-rayAP X-ray
Lateral:wall ofLateral:wall of
acetabulumacetabulum
Medial:lesser pelvisMedial:lesser pelvis
Inferior :acetabularInferior :acetabular
notchnotch
Appears between 6-23Appears between 6-23
momo
[delayed in DDH][delayed in DDH]](https://image.slidesharecdn.com/ddhhardik-130706213206-phpapp01/85/developemental-dysplasia-of-hip-47-320.jpg)
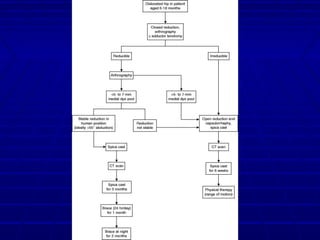
![ArthrogramArthrogram
Severin [1941]Severin [1941]
Normal appearance:Normal appearance:
LABRUM:LABRUM:
*Thorn over the*Thorn over the
femoral headfemoral head
*A recess of joint*A recess of joint
capsule overlies thecapsule overlies the
thornthorn](https://image.slidesharecdn.com/ddhhardik-130706213206-phpapp01/85/developemental-dysplasia-of-hip-58-320.jpg)