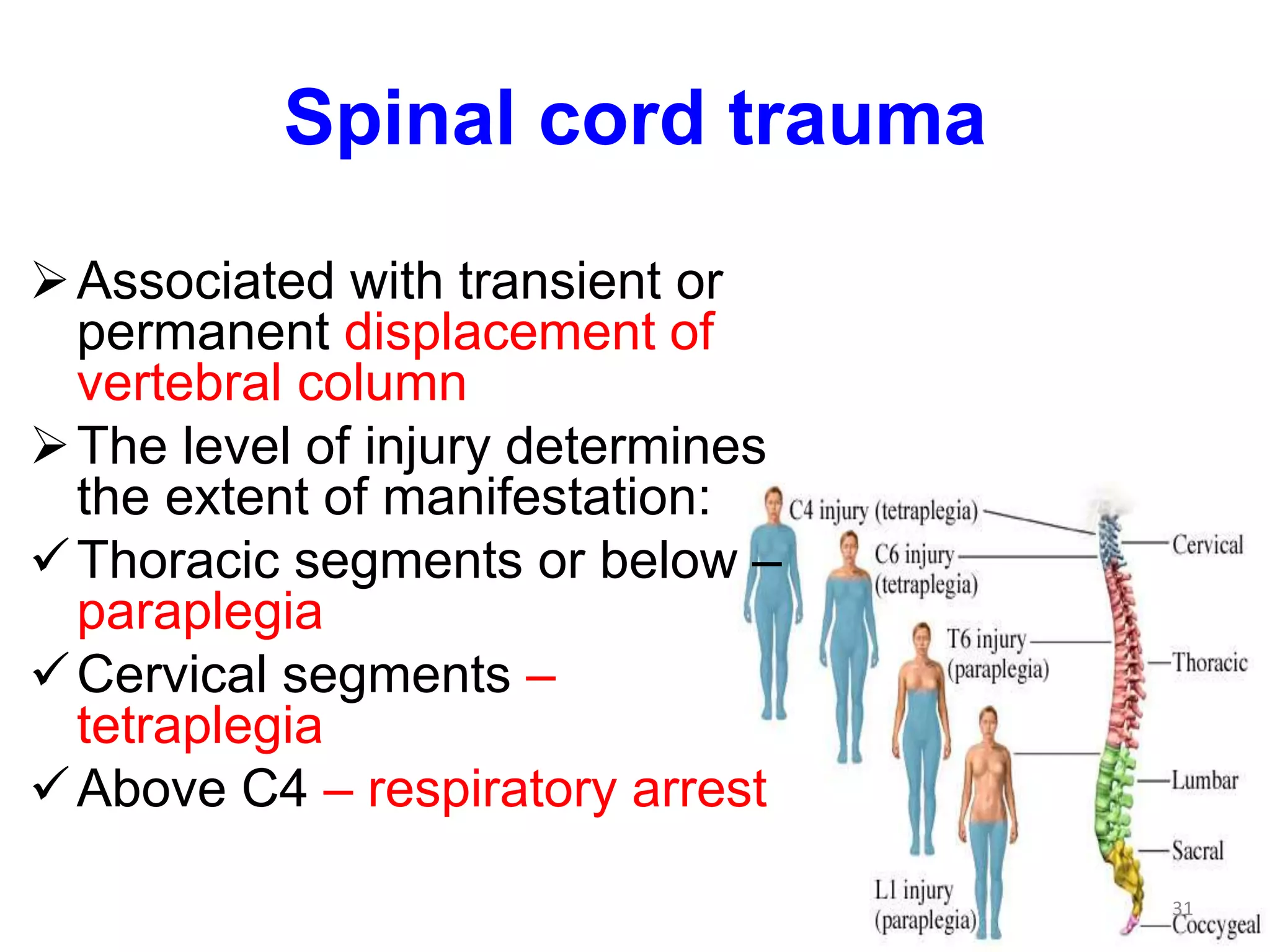
Head injuries from physical trauma can result in skull fractures, brain parenchymal injuries, and vascular injuries, which can all occur simultaneously. Trauma can cause closed or open head injuries that are either penetrating or blunt. The consequences of central nervous system trauma depend on the location of the lesion and the brain's limited ability to repair itself. Even injuries affecting just a few cubic centimeters of brain tissue can result in outcomes ranging from no symptoms to severe disability or death depending on the specific location.