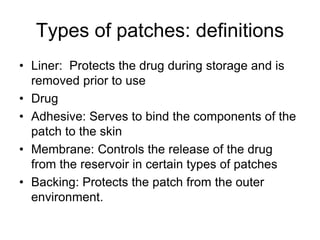
Transdermal drug delivery systems provide several advantages over oral administration, including maintaining consistent drug levels, avoiding first-pass metabolism, and not requiring active administration. There are two main types of patches - drug-in-adhesive patches where the drug is incorporated directly into the adhesive layer, and reservoir patches where the drug is contained separately from the adhesive. Limitations include the skin posing a barrier to larger drug molecules and low drug payloads, though these systems can still be commercially viable by maintaining drug levels over multiple days. Newer technologies like microneedles and iontophoresis aim to overcome limitations and expand the types of drugs that can be delivered transdermally.