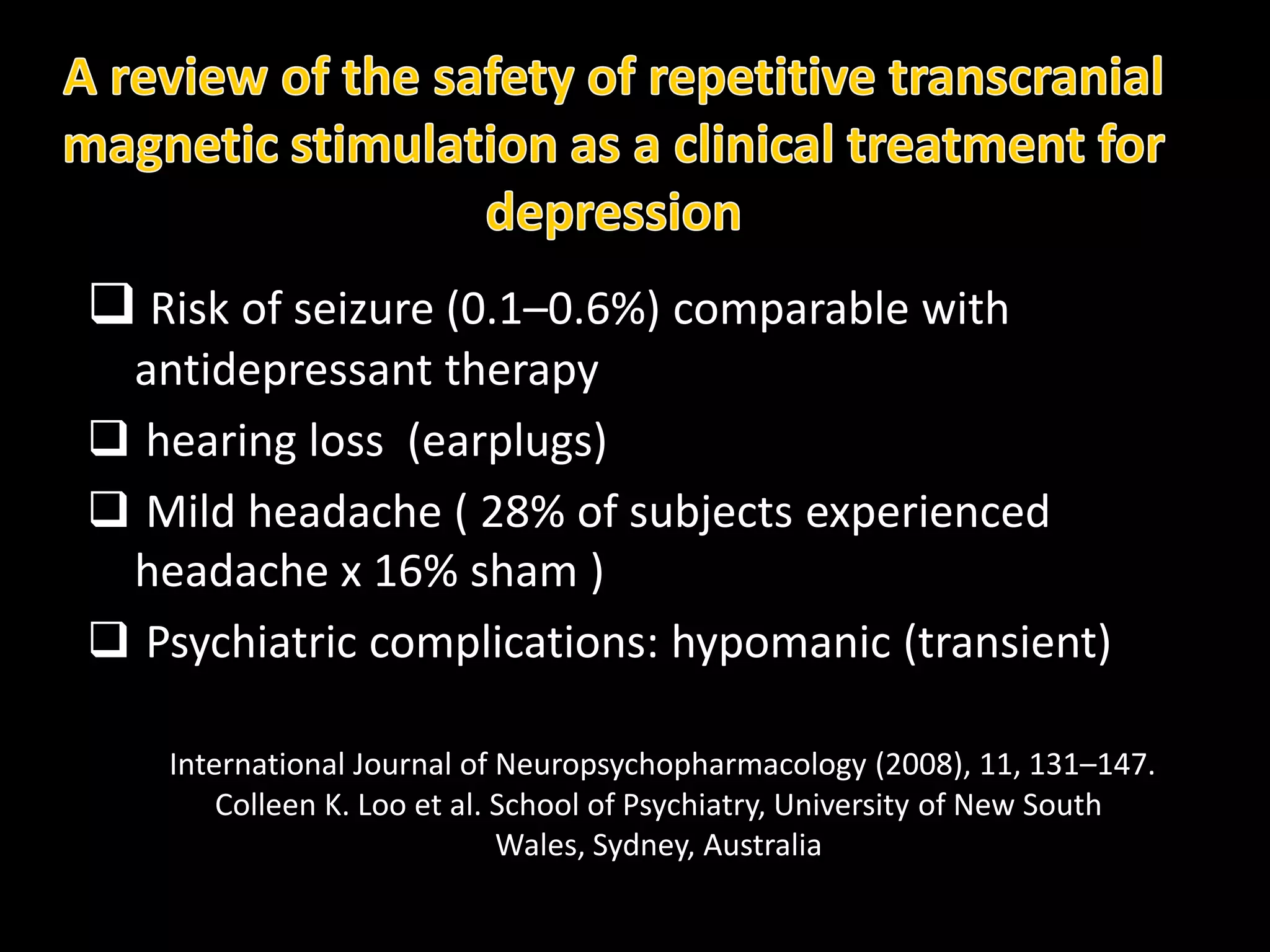
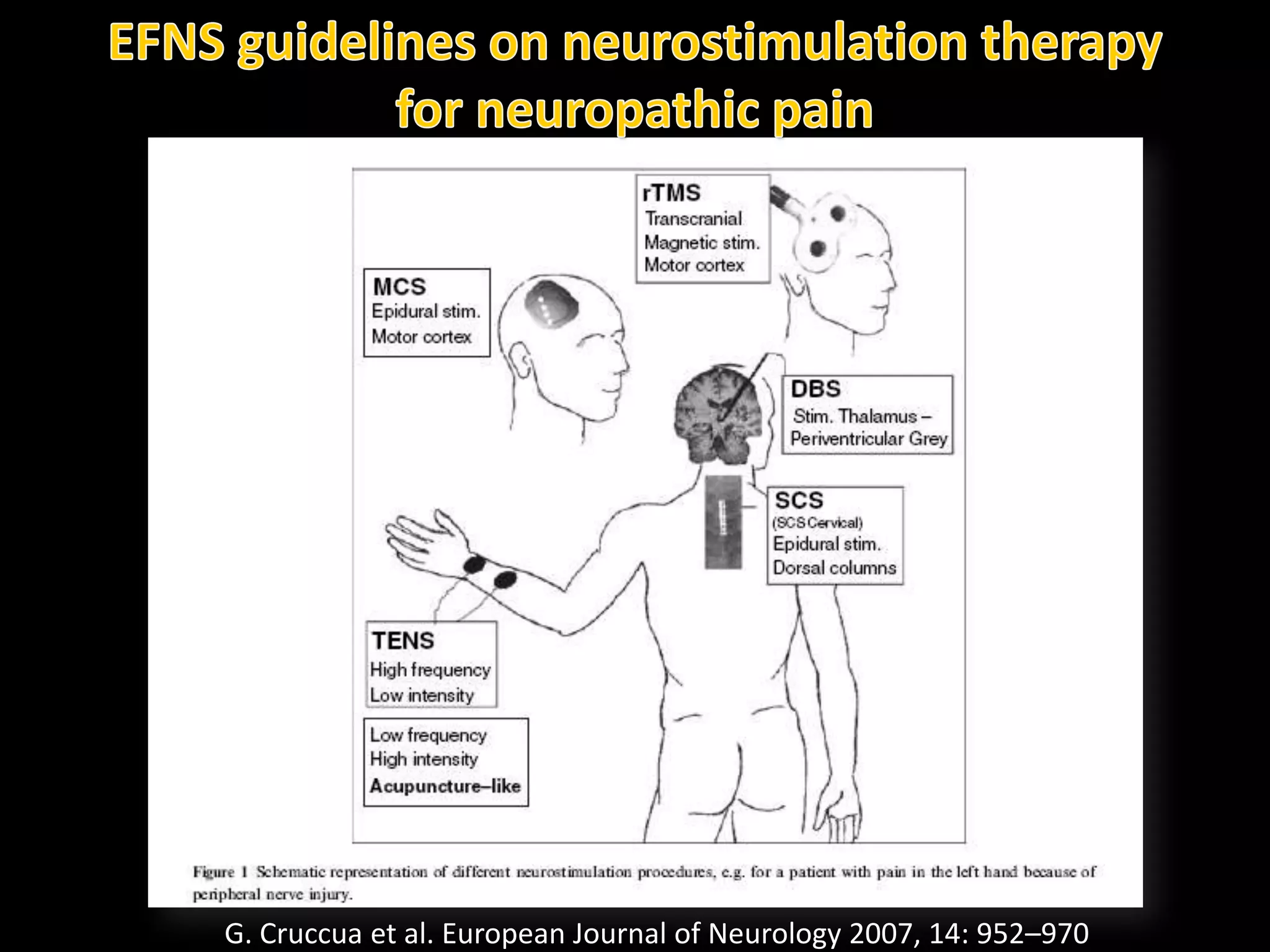
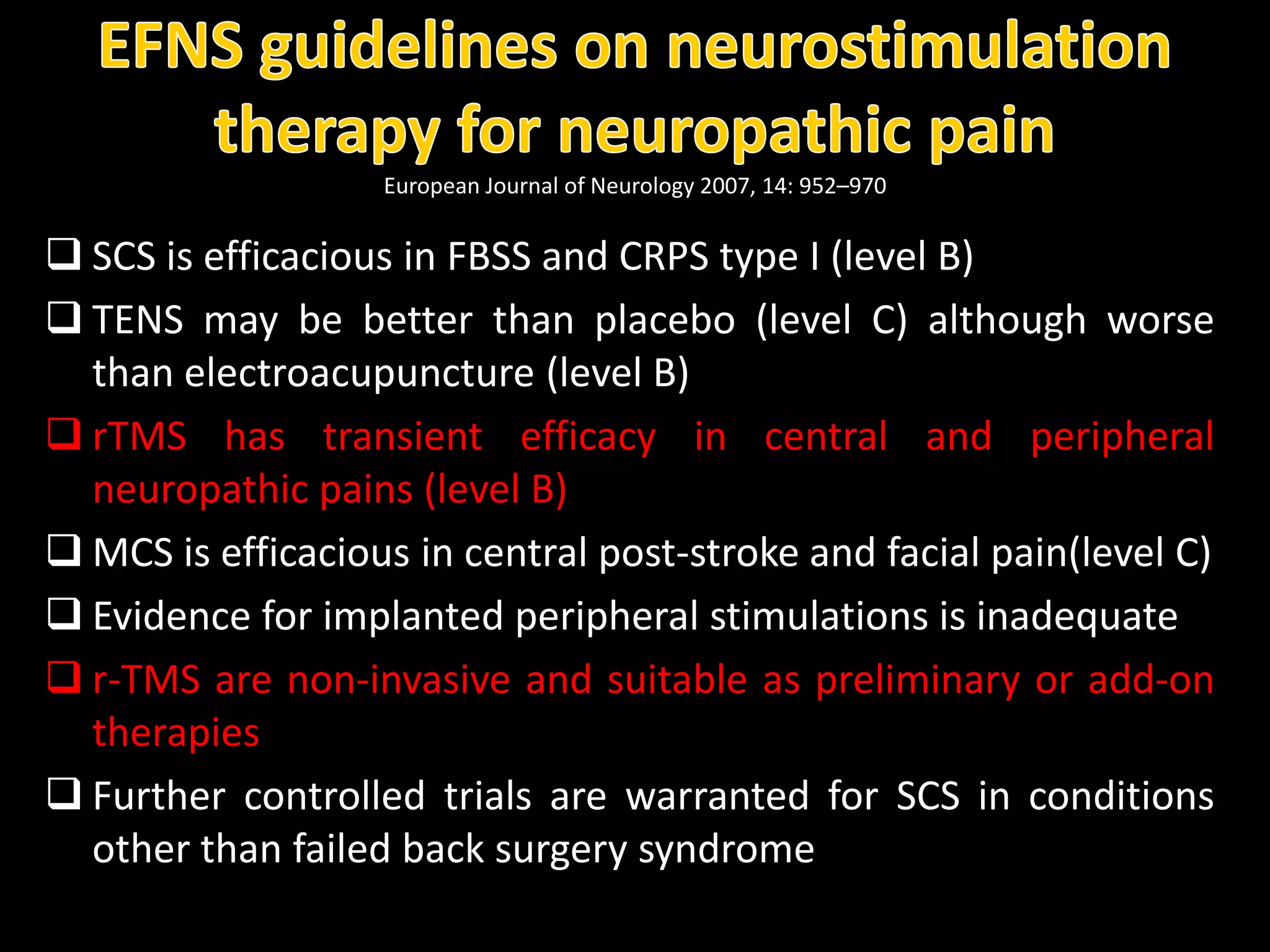
This document discusses the use of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS) for chronic pain management and its effects on various conditions such as stroke recovery and fibromyalgia. It reviews the efficacy, safety, and mechanism of action of rTMS, including results from several studies demonstrating its potential to reduce pain and decrease the need for opioids post-surgery. The findings suggest that rTMS could serve as a promising non-invasive treatment option for chronic pain patients, warranting further research and controlled trials.