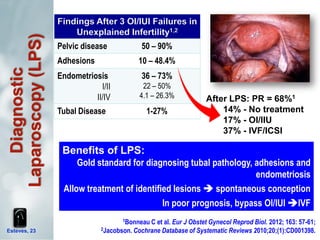
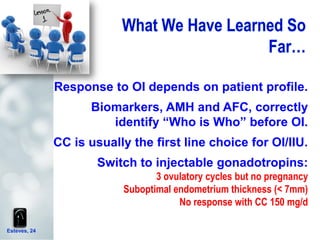
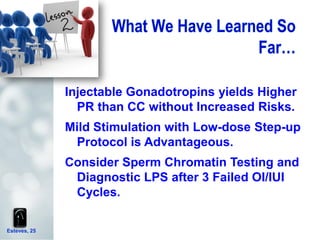
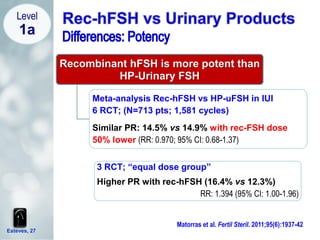
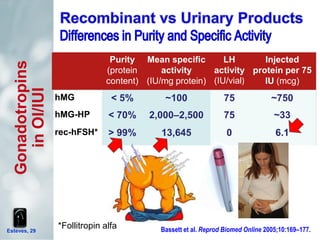
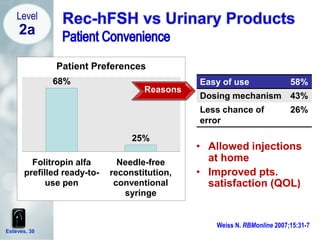
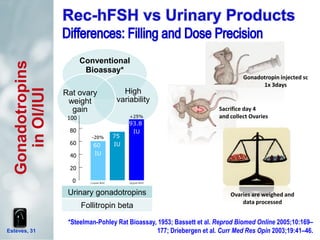
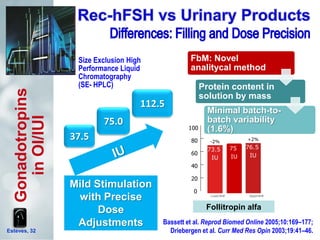
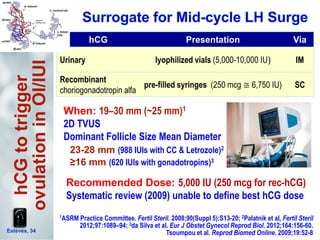
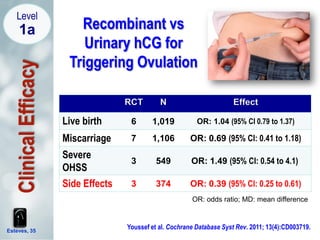
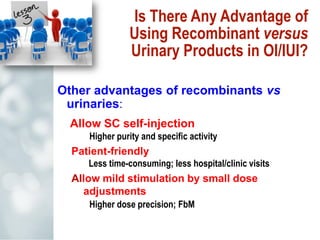
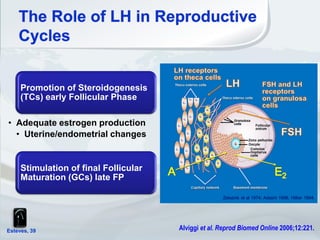
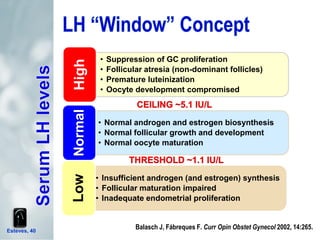
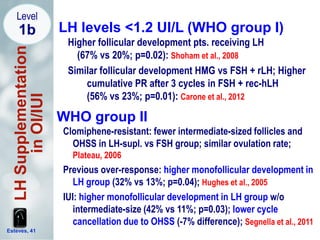
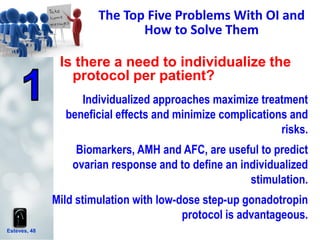
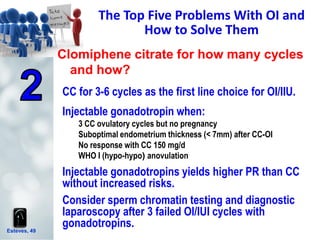
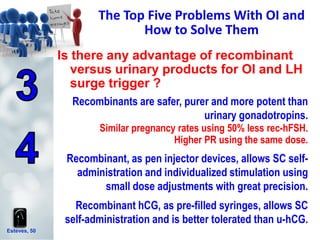
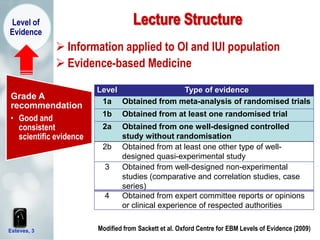
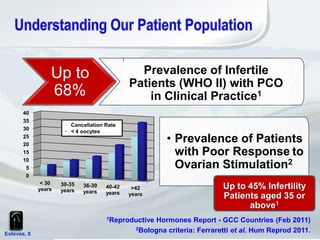
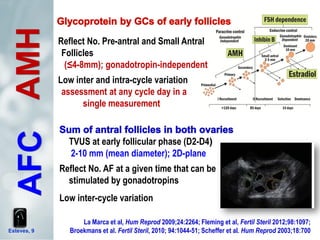
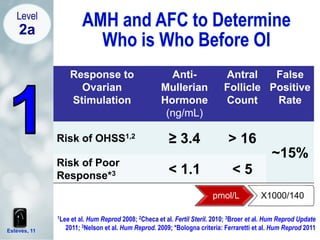
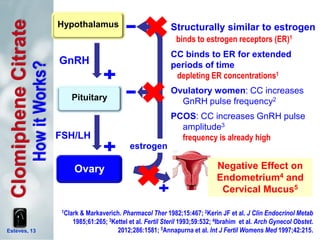
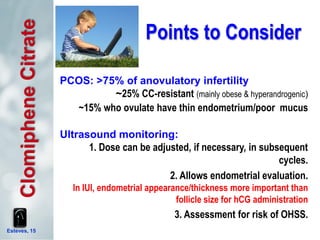
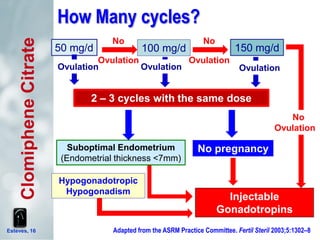
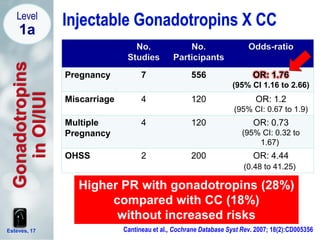
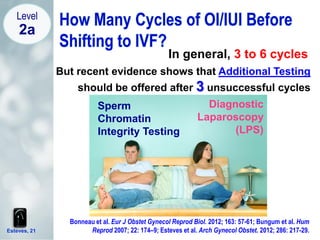
The document discusses the top five problems with ovulation induction and how to solve them. It addresses whether protocols need to be individualized, how long clomiphene citrate should be used, the advantages of recombinant versus urinary gonadotropins, the advantages of recombinant versus urinary hCG, and whether LH supplementation is needed. It provides evidence-based recommendations including that protocols should be tailored based on biomarkers and individual factors, clomiphene citrate is usually first-line for up to 3 cycles, and recombinant gonadotropins yield higher pregnancy rates than clomiphene without increased risks.


![Sperm Chromatin Dispersion Test:
Sperm with absent “halos” have
DNA strand breaks
Semen/Spermatozoa
Quantitative (Normal <20%)
Esteves et al. Arch Gynecol Obstet. 2012; 286: 217-29.
19%
1.5%
Normal Elevated
Live Birth Rates with
Intrauterine Insemination
OR = 0.07
[95% CI: 0.01-0.48]
Bungum et al. Hum
Reprod 2007; 22: 74–9](https://image.slidesharecdn.com/top5problemsyouhavewithoiandhowtosolvethemestevesslideshare-130607150320-phpapp01/85/Top-Five-Problems-You-Have-with-Ovulation-Induction-and-How-to-Solve-Them-22-320.jpg)