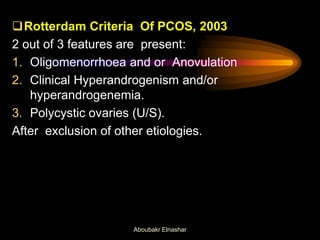
This document provides an overview of hirsutism. It begins with definitions of terms like hirsutism, virilization, and hypertrichosis. It then discusses the causes of hirsutism, which can include polycystic ovary syndrome (PCOS), ovarian tumors, adrenal tumors, and other conditions. The document reviews approaches to clinical evaluation and investigations for hirsutism, including the Ferriman-Gallwey scoring system. It provides guidelines on tests to measure androgens and rule out conditions like congenital adrenal hyperplasia. Overall, the document provides a comprehensive review of hirsutism, including its definition, causes, evaluation, and treatment guidelines.





























































![17 OHP:
an intermediate metabolite in steroidogensis in the adrenals.
In patients with a high likelihood of congenital
adrenal hyperplasia [positive family history, member of
a high-risk ethnic group such as Ashkenazi Jews
(prevalence 1 in 27), Hispanics
(1 in 40), and Slavics (1 in 50)], we recommend
measurement of an early morning follicular phase level
of 17-hydroxyprogesterone.
DHEAS:
Good marker of Adrenal A production
Not essential
Aboubakr Elnashar](https://image.slidesharecdn.com/hirsutism2013-140804224149-phpapp02/85/Hirsutism-65-320.jpg)