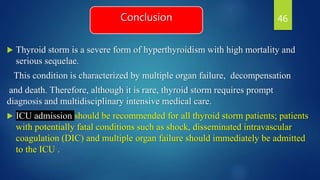
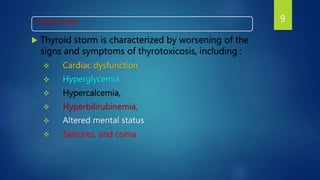
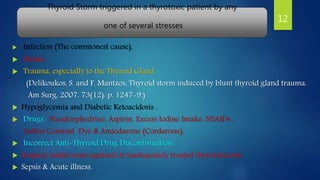
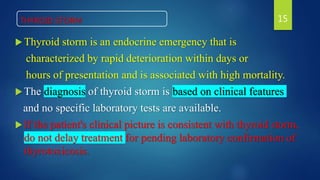
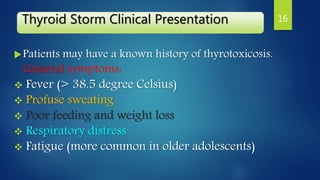
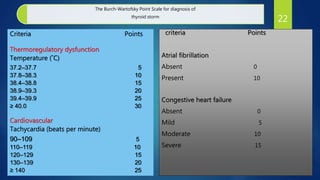
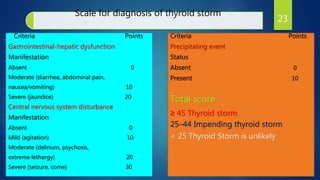
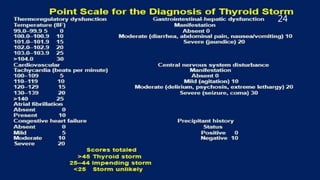
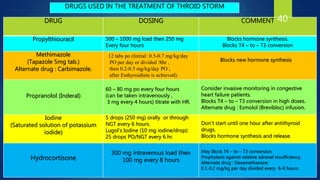
Thyroid storm is a life-threatening exacerbation of hyperthyroidism that can develop in patients with undiagnosed or untreated hyperthyroidism when stressed. It is characterized by worsening signs and symptoms of thyrotoxicosis including cardiac dysfunction, hyperglycemia, altered mental status, and seizures. Diagnosis is based on clinical features and scoring systems, with a Burch-Wartofsky score of over 45 suggestive of thyroid storm. Treatment involves supportive care, administration of beta blockers, antithyroid medications, iodine, and glucocorticoids to reduce thyroid hormone levels and symptoms.

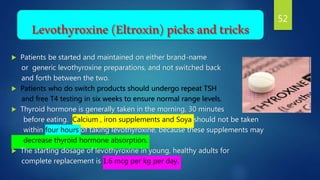
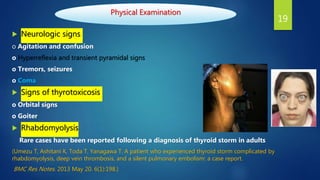
![Physical Examination
Fever
Temperature consistently exceeds 38.5°C.
Patients may progress to hyperpyrexia.
Temperature frequently exceeds 41°C.
Excessive sweating.
Cardiovascular signs
o Hypertension with wide pulse pressure.
o Hypotension in later stages with shock.
o Tachycardia disproportionate to fever.
o Signs of high-output heart failure.
o Cardiac arrhythmia (Supraventricular arrhythmias are more common,
[e.g., atrial flutter and fibrillation] , but ventricular tachycardia may also occur.)
18](https://image.slidesharecdn.com/thyroidstormfinala-210715051251/85/Thyroid-storm-final-a-18-320.jpg)



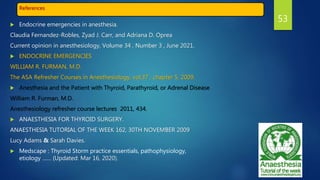
![Bile acid sequestarnts
Prevent reabsorption of free THs in the gut (released from conjugated TH
metabolites secreted into bile through the enterohepatic circulation).
A recommended dose is 4 g of cholestyramine every 6 hours
via a nasogastric tube. Another option is 20-30 g/day of Colestipol-HCl.
De Groot LJ, Bartalena L, De Groot LJ, Chrousos G, Dungan K, Feingold KR, et al. Thyroid Storm. In: De
Groot LJ, Beck-Peccoz P, Chrousos G, Dungan K, Grossman A, Hershman JM, Koch C, McLachlan R, New M,
Rebar R, Singer F, Vinik A, Weickert MO, editors. SourceEndotext [Internet]. South Dartmouth (MA):
MDText.com, Inc. 2000.
42](https://image.slidesharecdn.com/thyroidstormfinala-210715051251/85/Thyroid-storm-final-a-42-320.jpg)