This document discusses thyroid disease, including:
- Thyroid disorders affect over 4 crore people in India, with 90% undiagnosed.
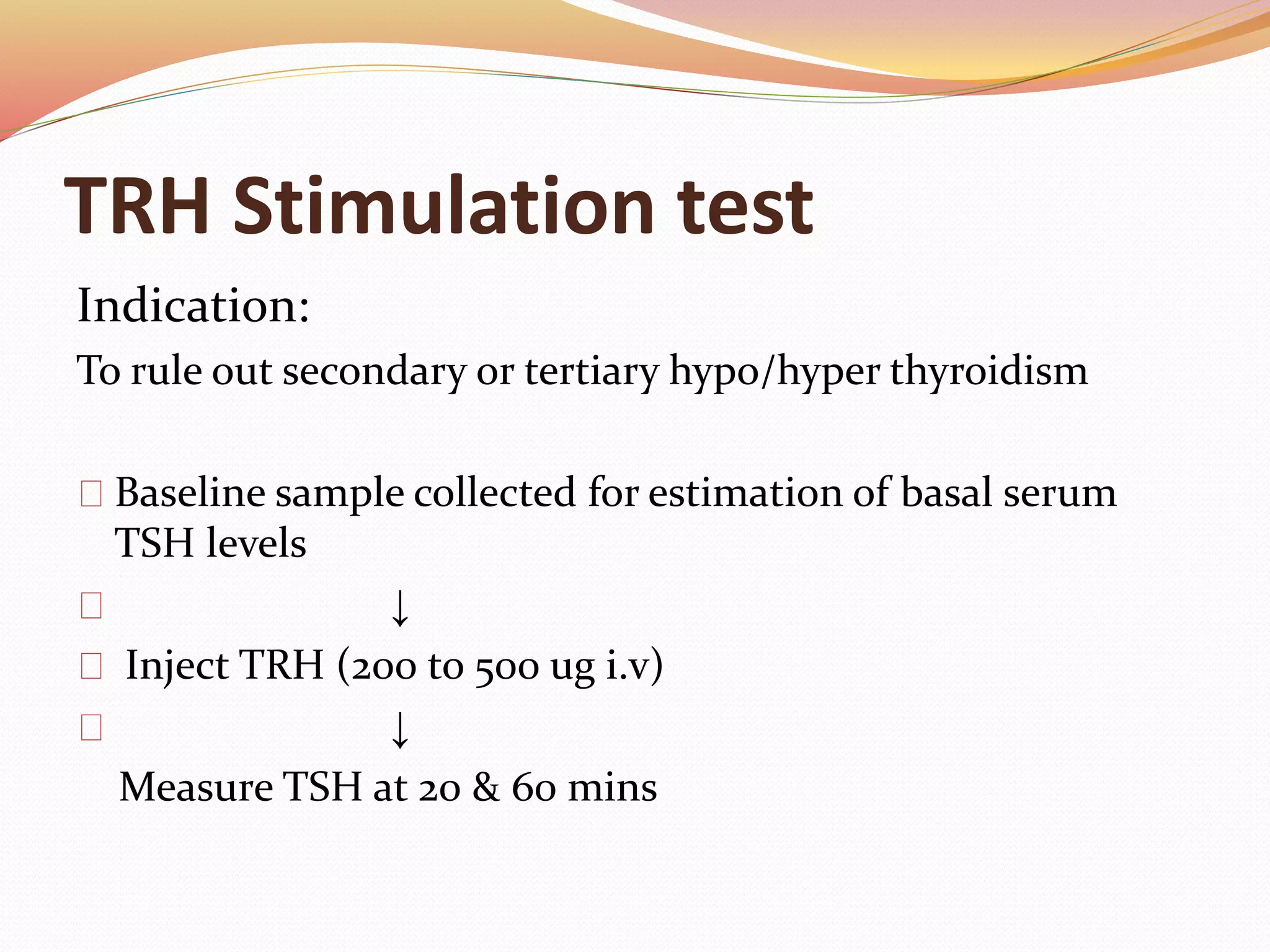
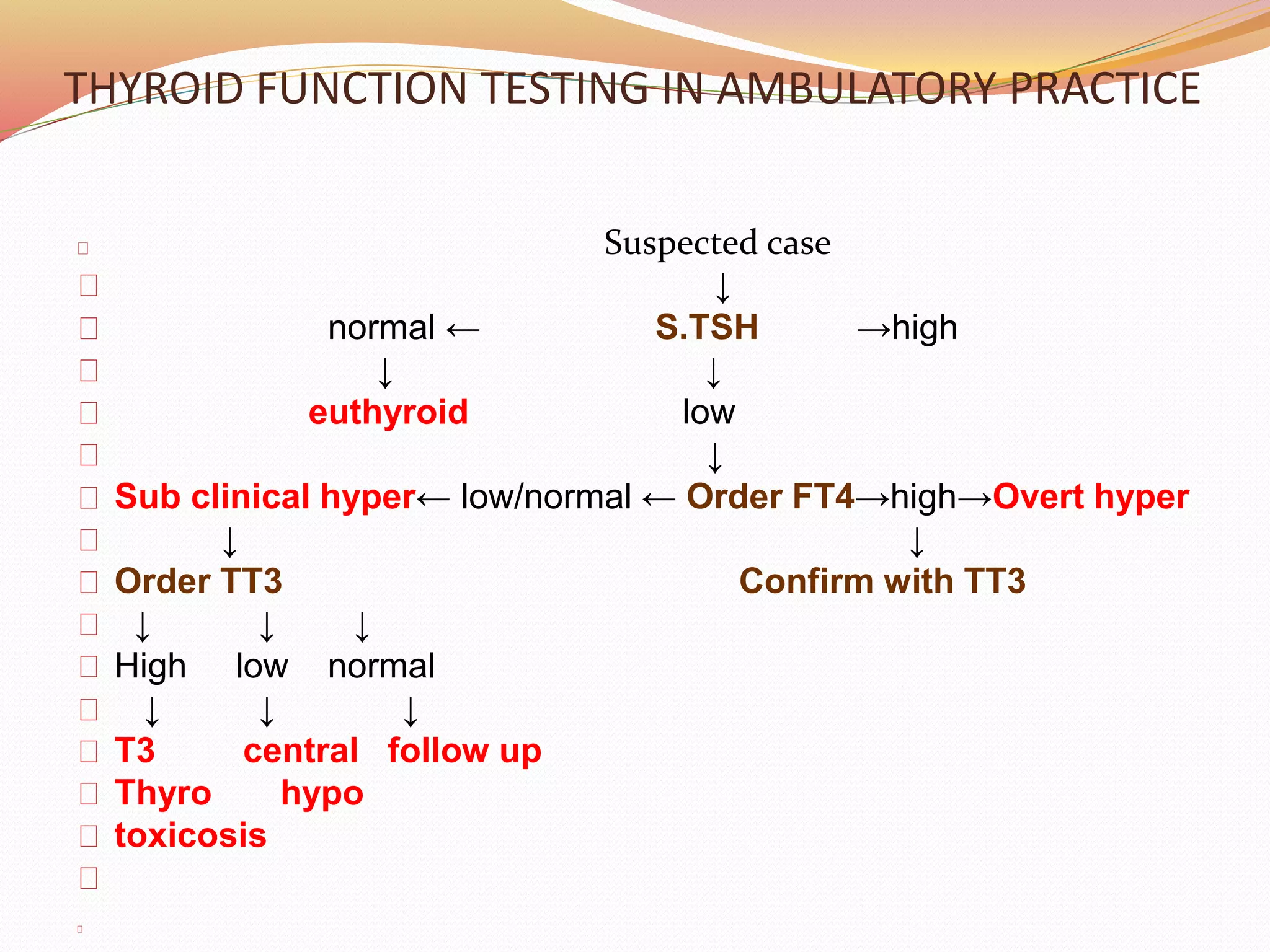
- Thyroid function tests include TSH, FT3, FT4, T3, T4, thyroid antibodies, and urinary iodine.
- Hypothyroidism is more common than hyperthyroidism. Causes include iodine deficiency, Hashimoto's, and surgery. Signs include dry skin, weight gain, and fatigue.
- Hyperthyroidism causes include Graves' disease. Signs include warm moist skin, weight loss, and tachycardia.
- Subclinical