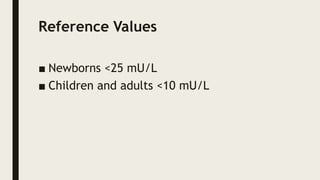
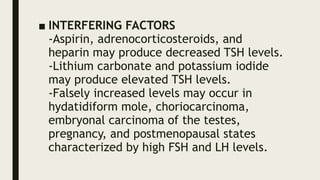
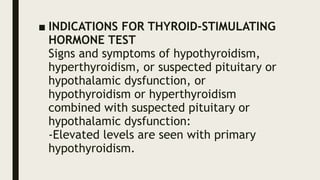
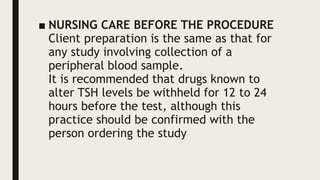
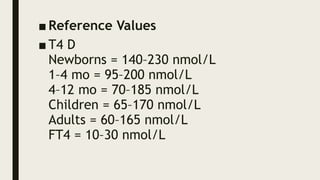
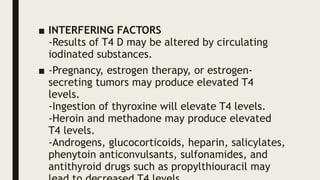
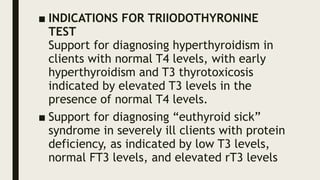
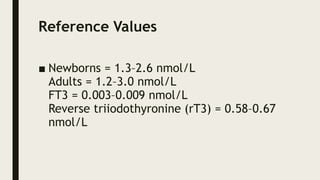
Thyroid-stimulating hormone (TSH) is produced in response to decreased thyroid hormone levels and regulates the thyroid gland's hormone production. TSH tests are crucial for diagnosing thyroid conditions such as hypothyroidism and hyperthyroidism, and results can be affected by various medications and physiological states. The document also discusses the measurement of thyroxine (T4) and triiodothyronine (T3), emphasizing their roles in metabolism and how to interpret their levels relative to thyroid function.