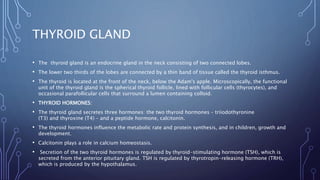
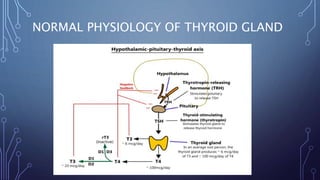
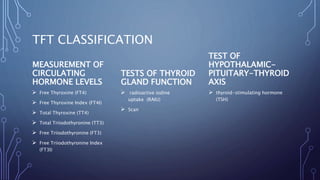
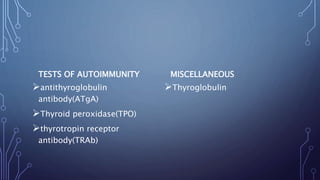
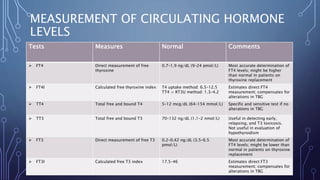
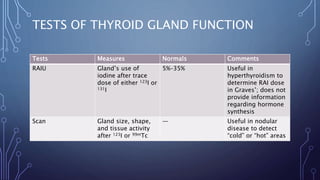
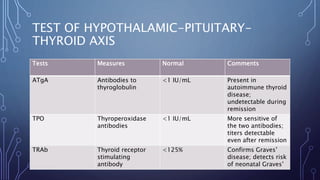
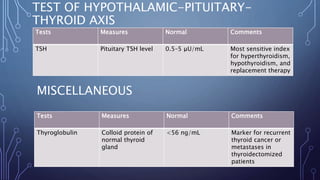
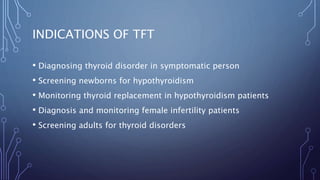
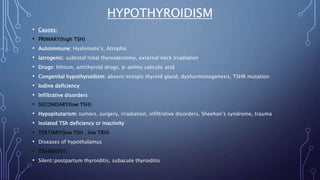
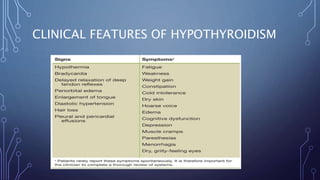
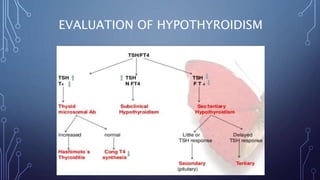
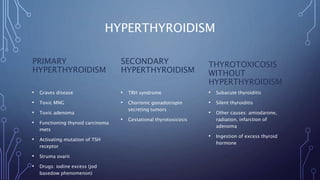
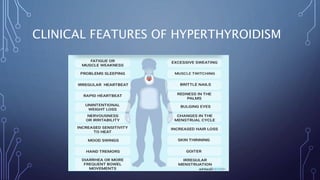
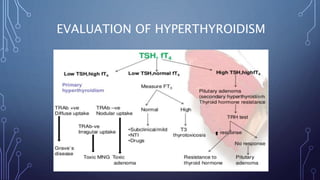
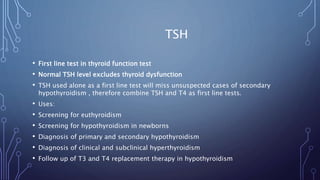
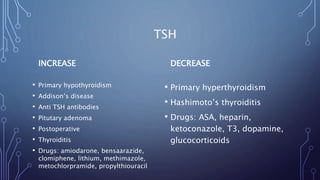
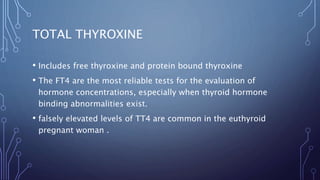
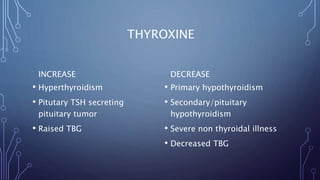
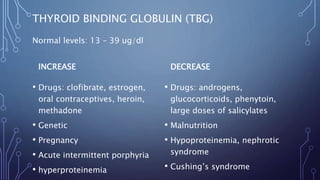
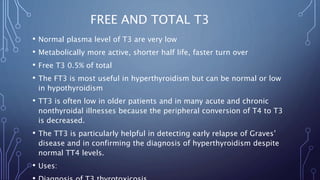
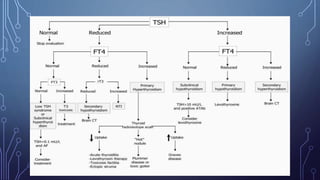
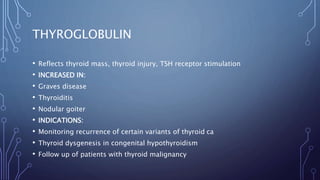
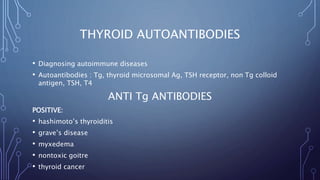
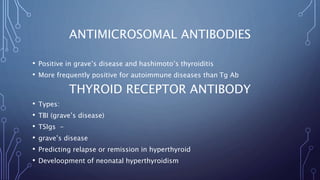
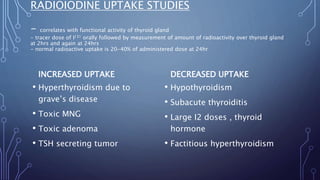
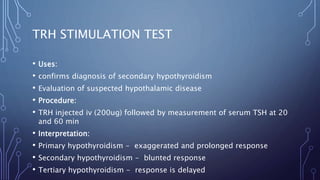
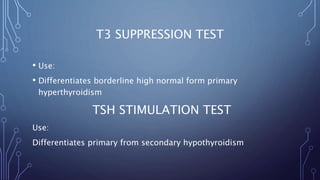
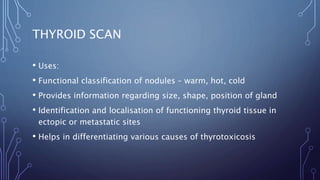
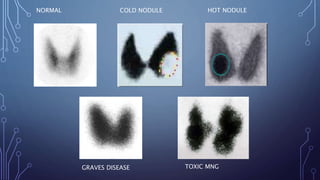
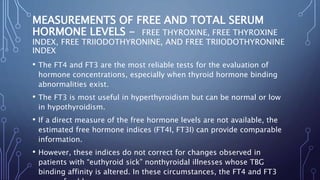
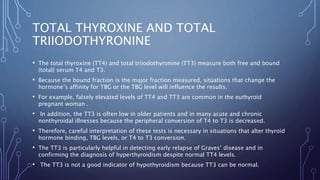
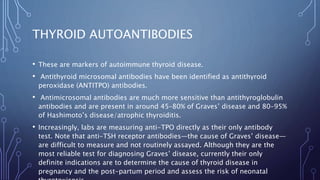
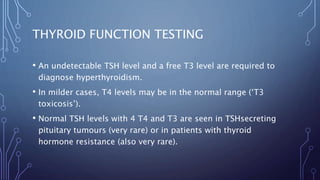
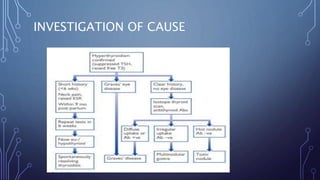
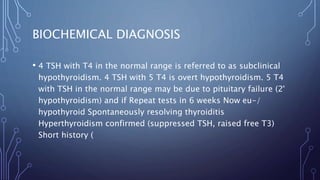
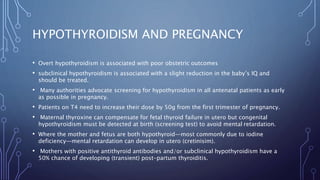
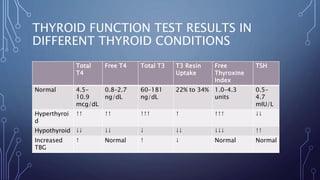
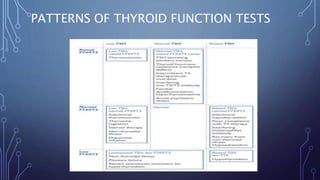
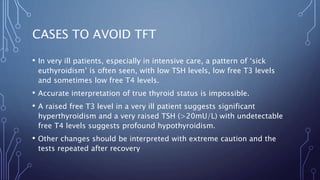
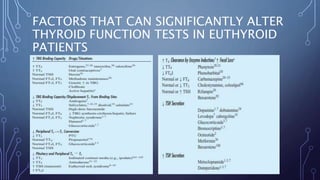
The document discusses thyroid function testing. It describes the thyroid gland and the hormones it secretes. It then covers the different types of thyroid function tests, including measurements of circulating hormone levels, tests of thyroid gland function and the hypothalamic-pituitary-thyroid axis, tests of autoimmunity, and miscellaneous tests. It discusses the indications, abnormalities, and clinical features associated with hypothyroidism and hyperthyroidism.