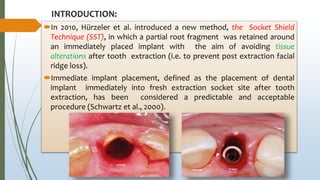
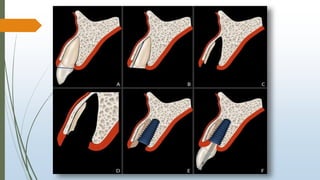
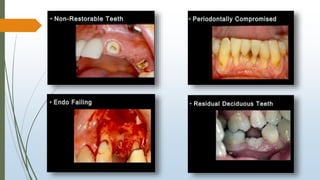
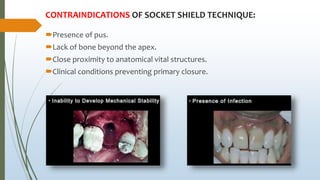
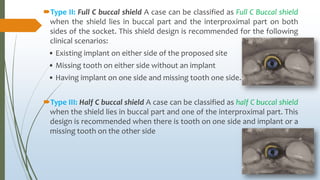
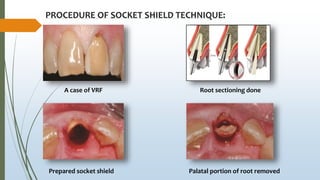
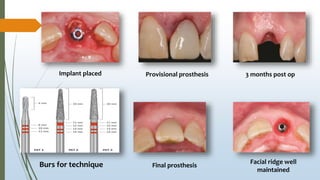
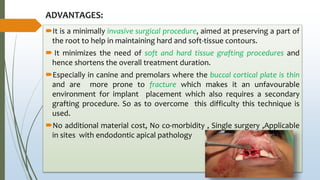
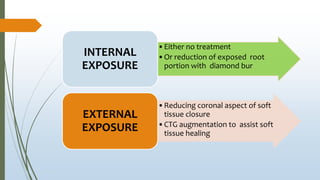
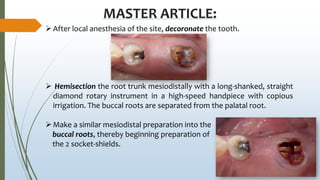
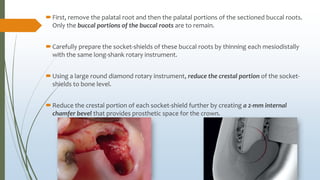
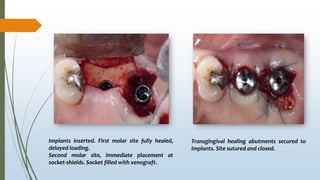
The document discusses the socket-shield technique, introduced in 2010 to help preserve buccal tissues during immediate implant placements by retaining a portion of the root post-extraction. It outlines indications, contraindications, procedural steps, advantages, limitations, and complications associated with the technique, emphasizing its potential benefits for maintaining ridge contour and minimizing surgery-associated tissue loss. The summary concludes with a mention of the technique's rising popularity and relevance in preserving hard and soft tissues post-tooth extraction.