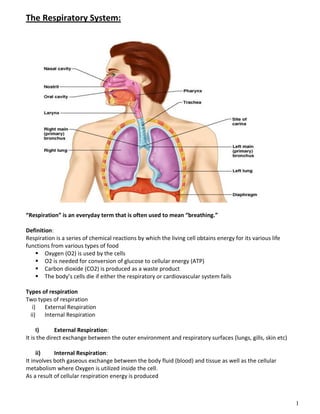
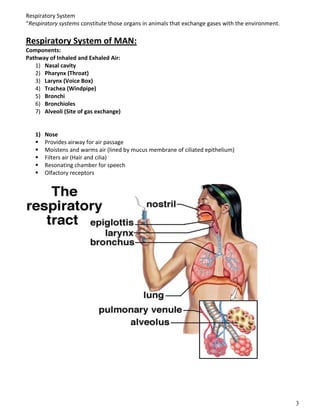
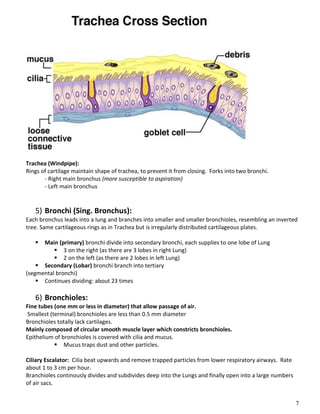
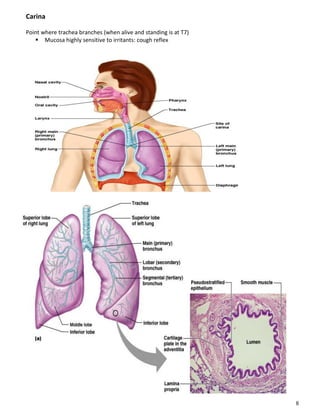
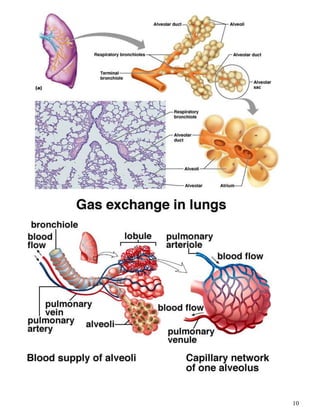
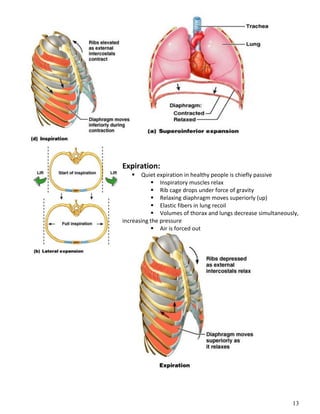
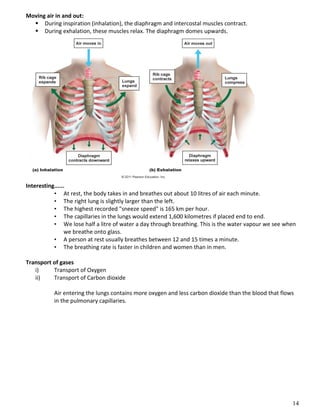
The respiratory system obtains oxygen from the air and transports it to cells via respiration. Oxygen diffuses into the lungs and blood, while carbon dioxide diffuses out of the blood and into the air. The blood then transports gases between the lungs and body tissues via internal respiration. Key components include the nasal cavity, pharynx, larynx, trachea, bronchi, bronchioles and alveoli where gas exchange occurs through thin epithelial walls. Hemoglobin transports oxygen in the blood and facilitates diffusion in tissues through factors like pH and temperature changes.