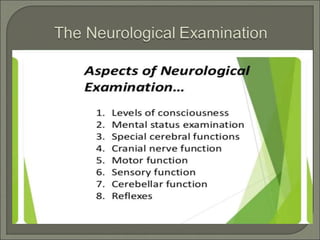
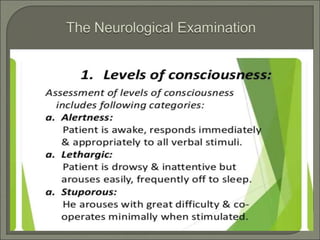
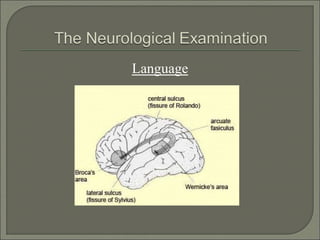
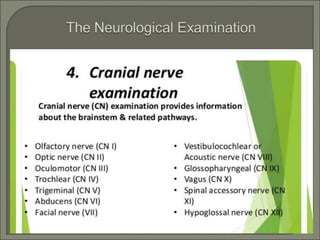
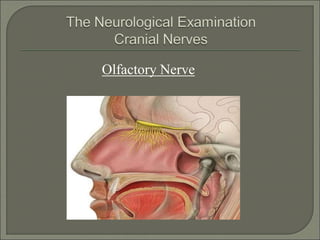
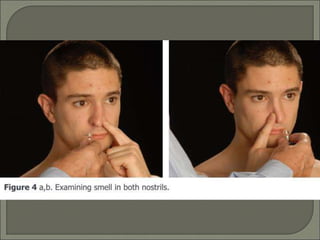
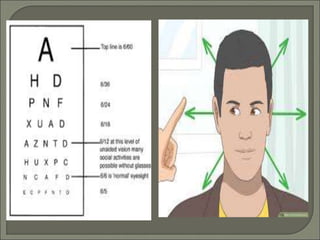
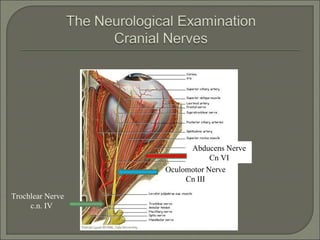
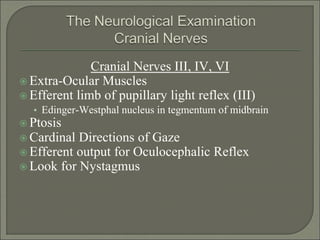
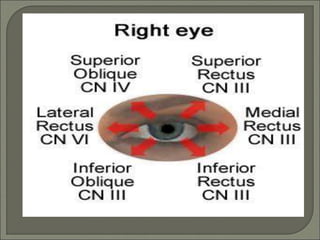
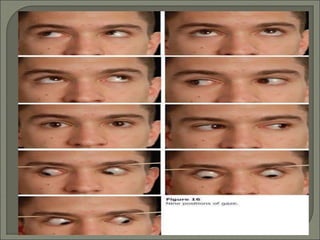
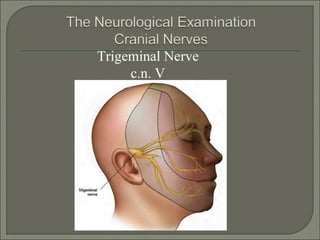
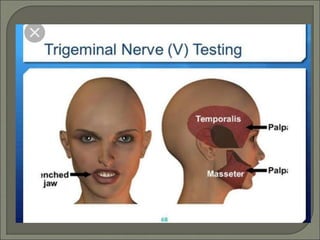
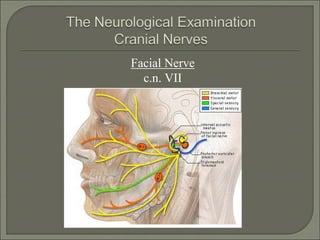
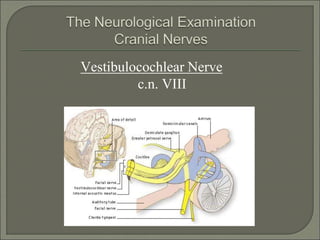
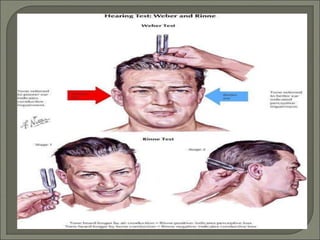
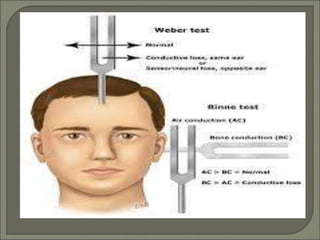
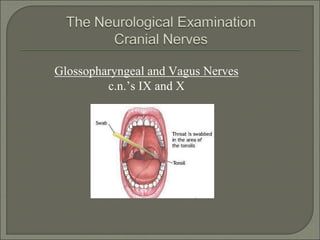
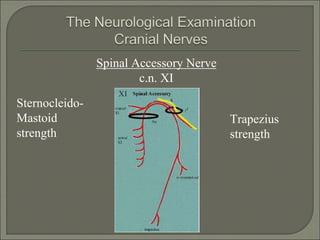
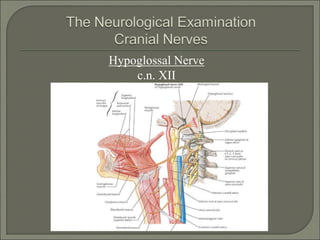
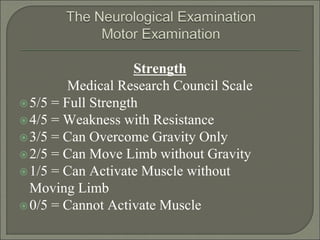
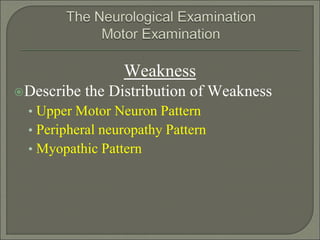
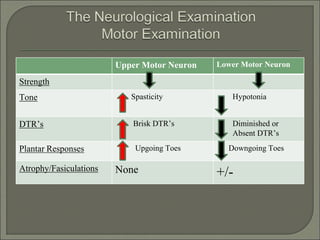
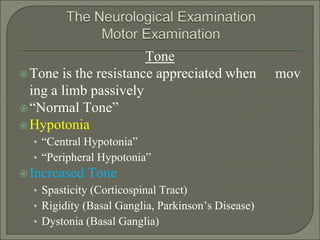
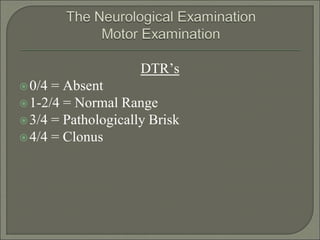
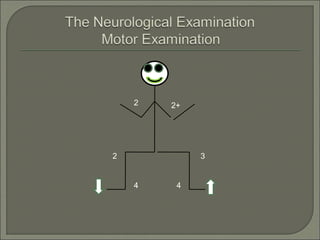
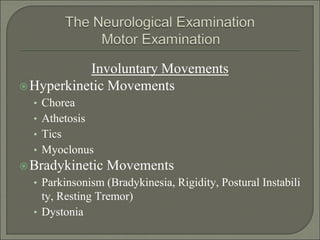
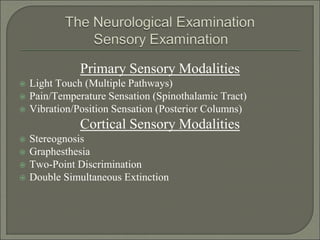
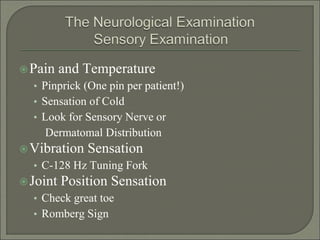
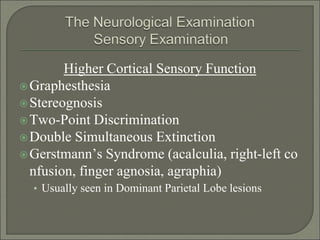
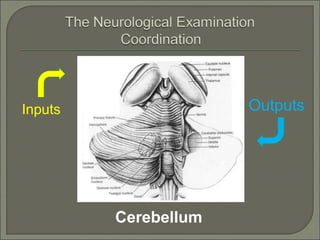
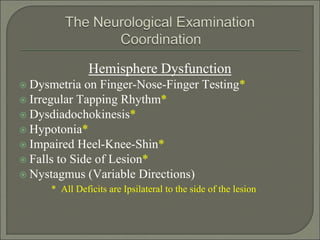
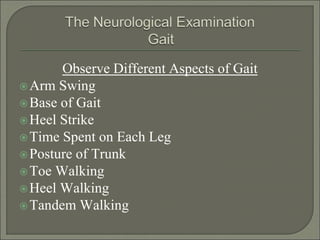
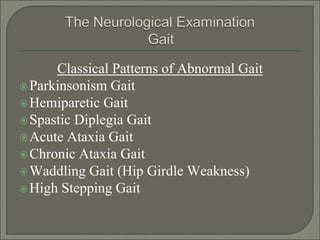
This document provides an overview of the neurological examination. It discusses examining various cranial nerves including visual acuity, eye movements, facial sensation, hearing, balance, and tongue and facial muscle function. It also covers assessing strength, tone, reflexes, sensory function, coordination, gait, and higher cognitive abilities. The exam evaluates multiple neurological domains to localize potential lesions in the brain or peripheral nervous system.