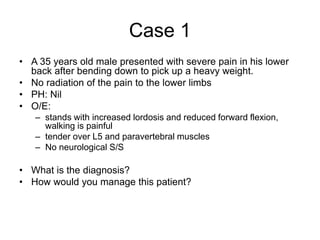
Case 1: A 35-year-old male presented with severe lower back pain after heavy lifting. Exam found tender lumbar spine, reduced flexion, and no neurological symptoms. Diagnosis is acute mechanical lower back pain. Management is pain medication, muscle relaxants, and advice on recovery expectations.
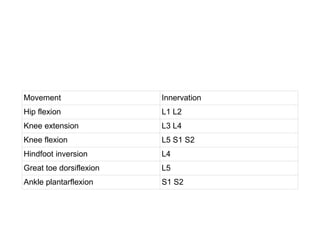
Case 2: A 37-year-old male also had lower back pain after heavy lifting, but now the pain radiates down his left leg. Exam found reduced back movement, weak left ankle plantar flexion and big toe flexion, and altered sensation in the left foot. Diagnosis is acute neurogenic lower back pain likely due to herniated disc. Management includes medications and advice, with consideration of imaging and specialist