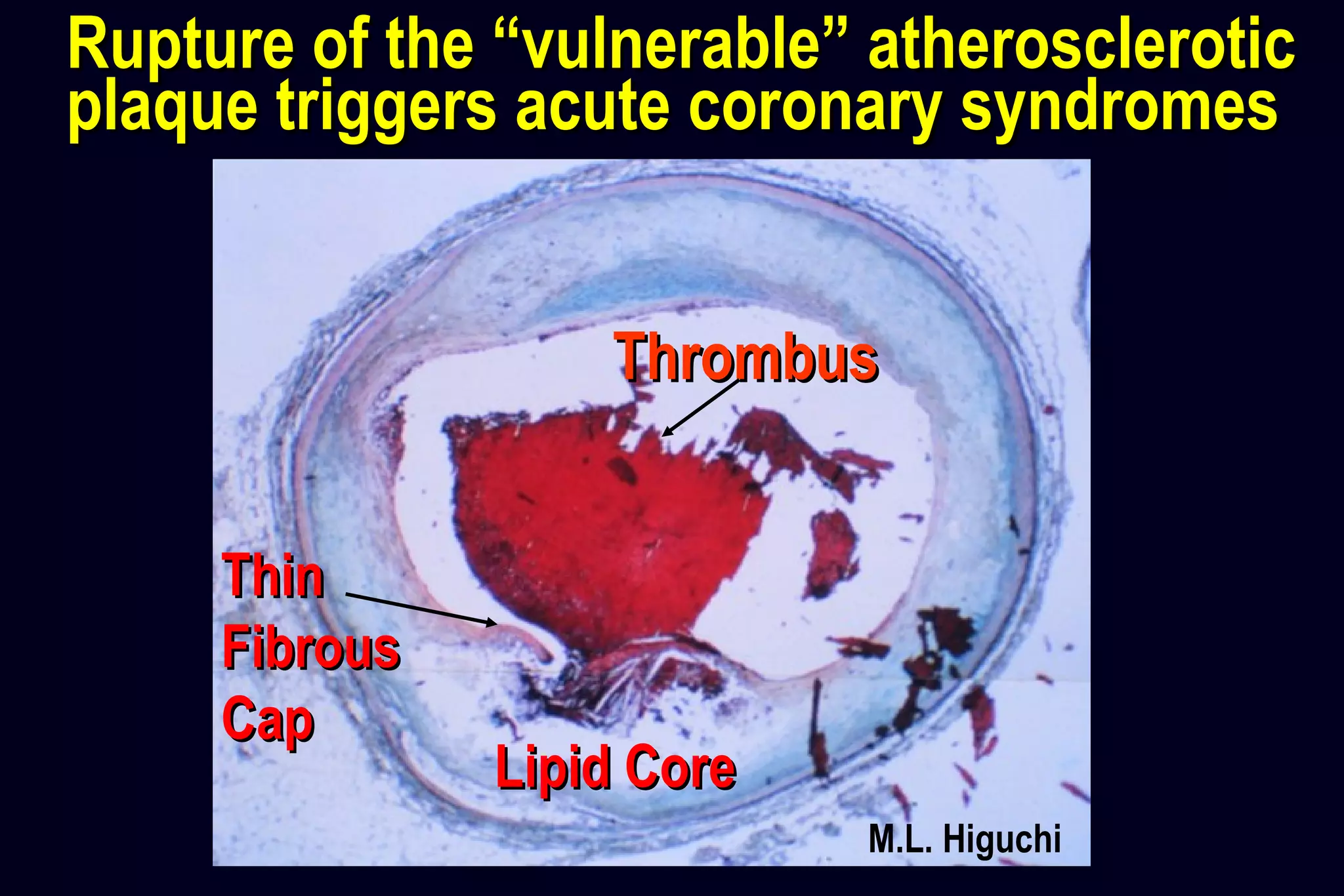
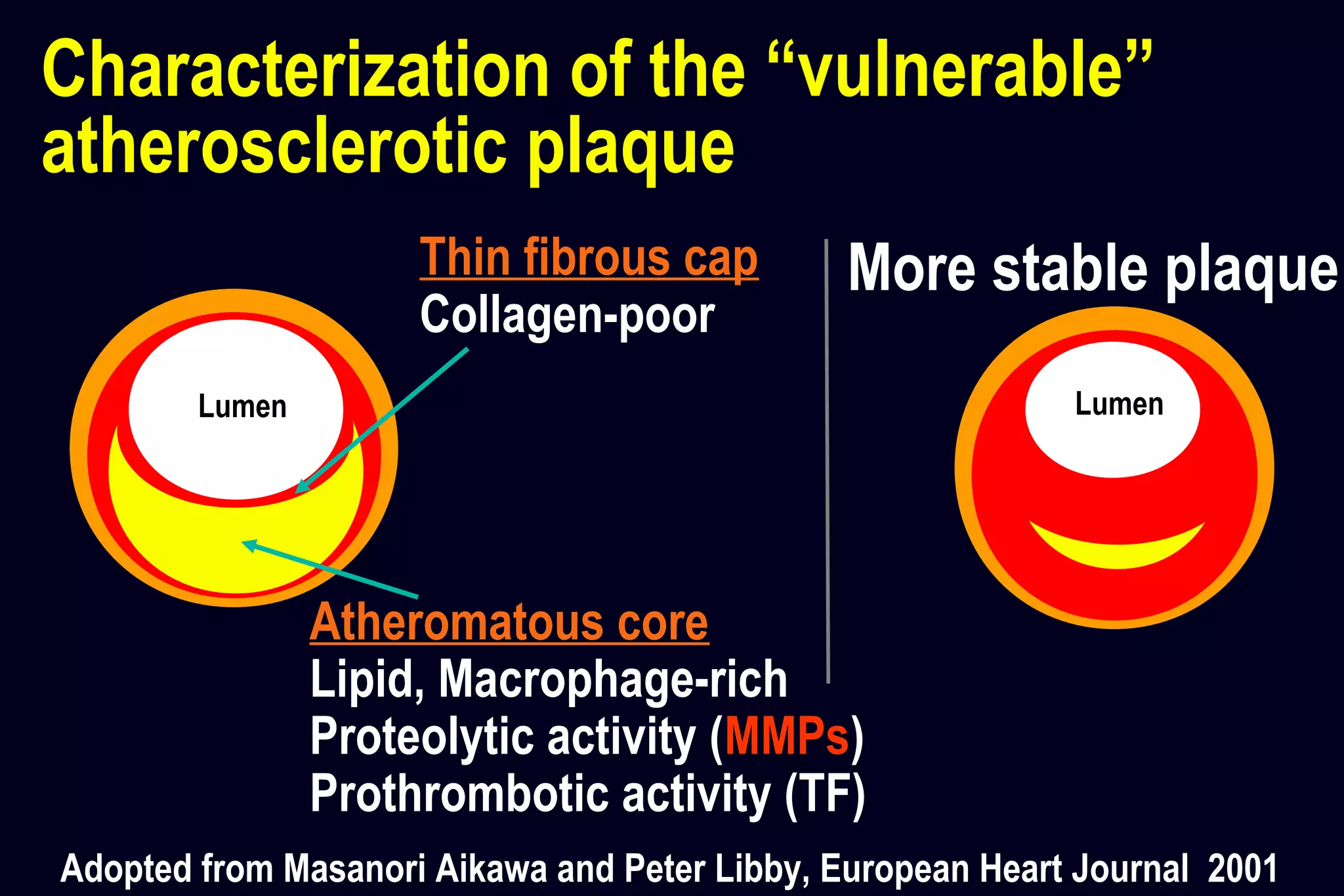
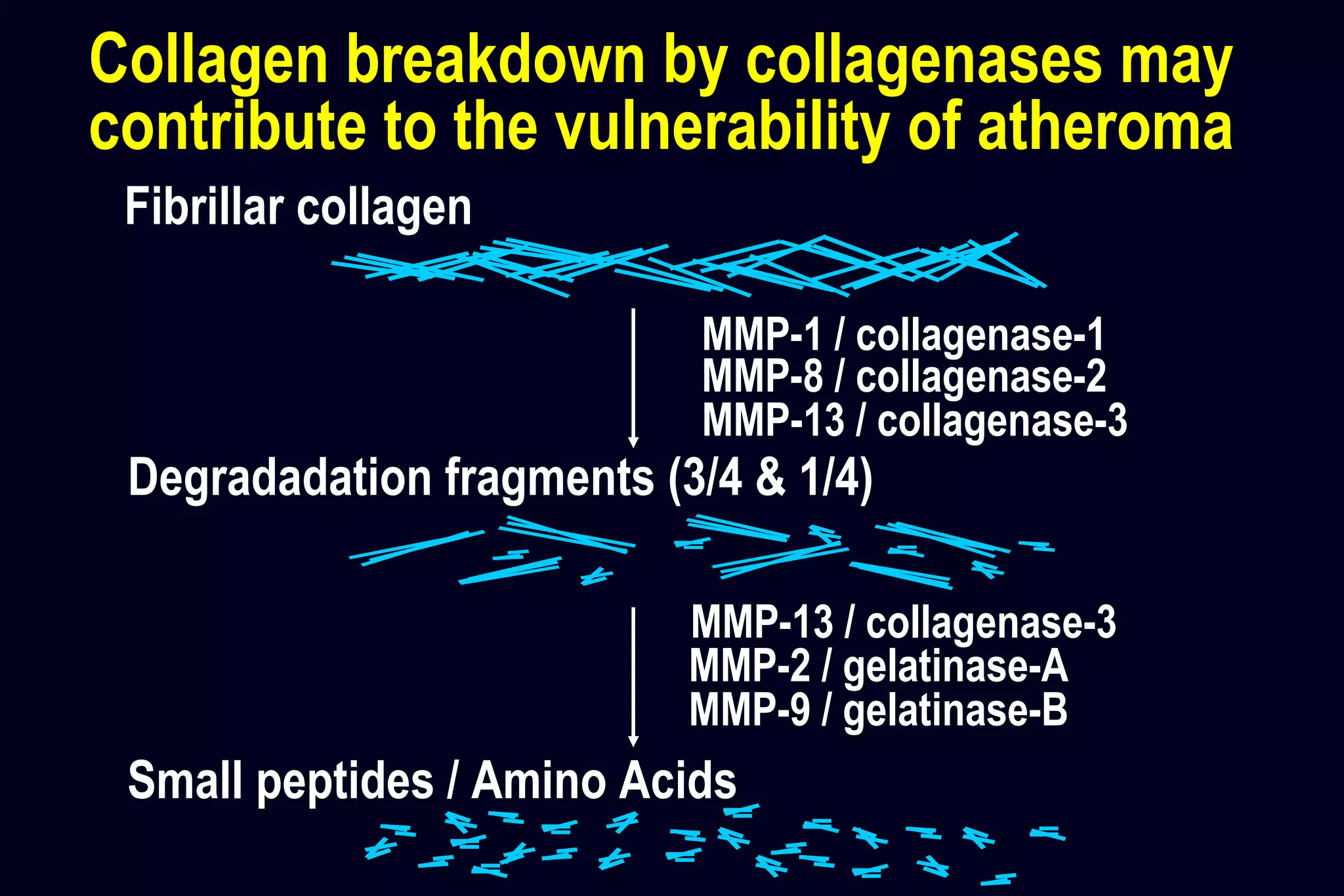
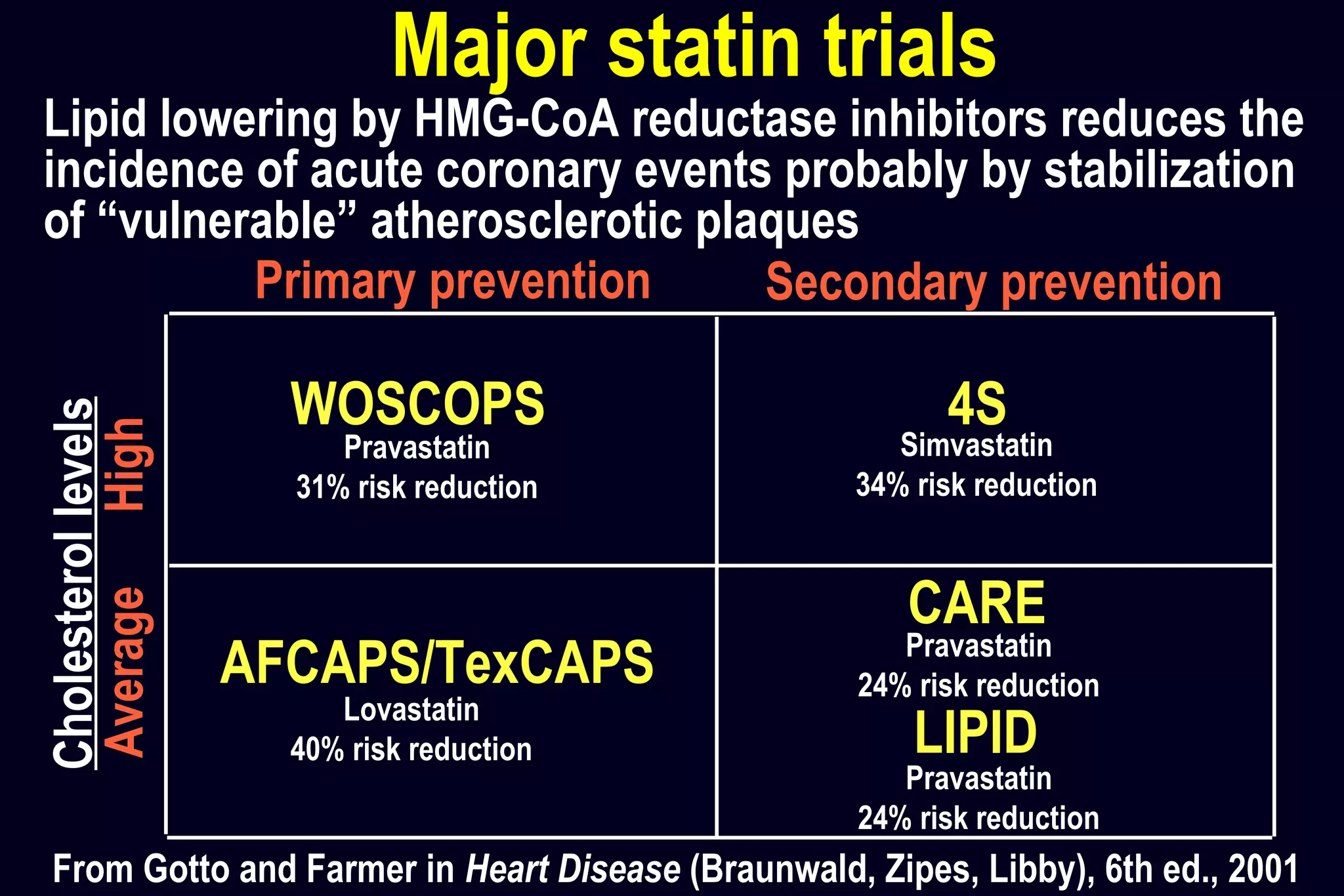
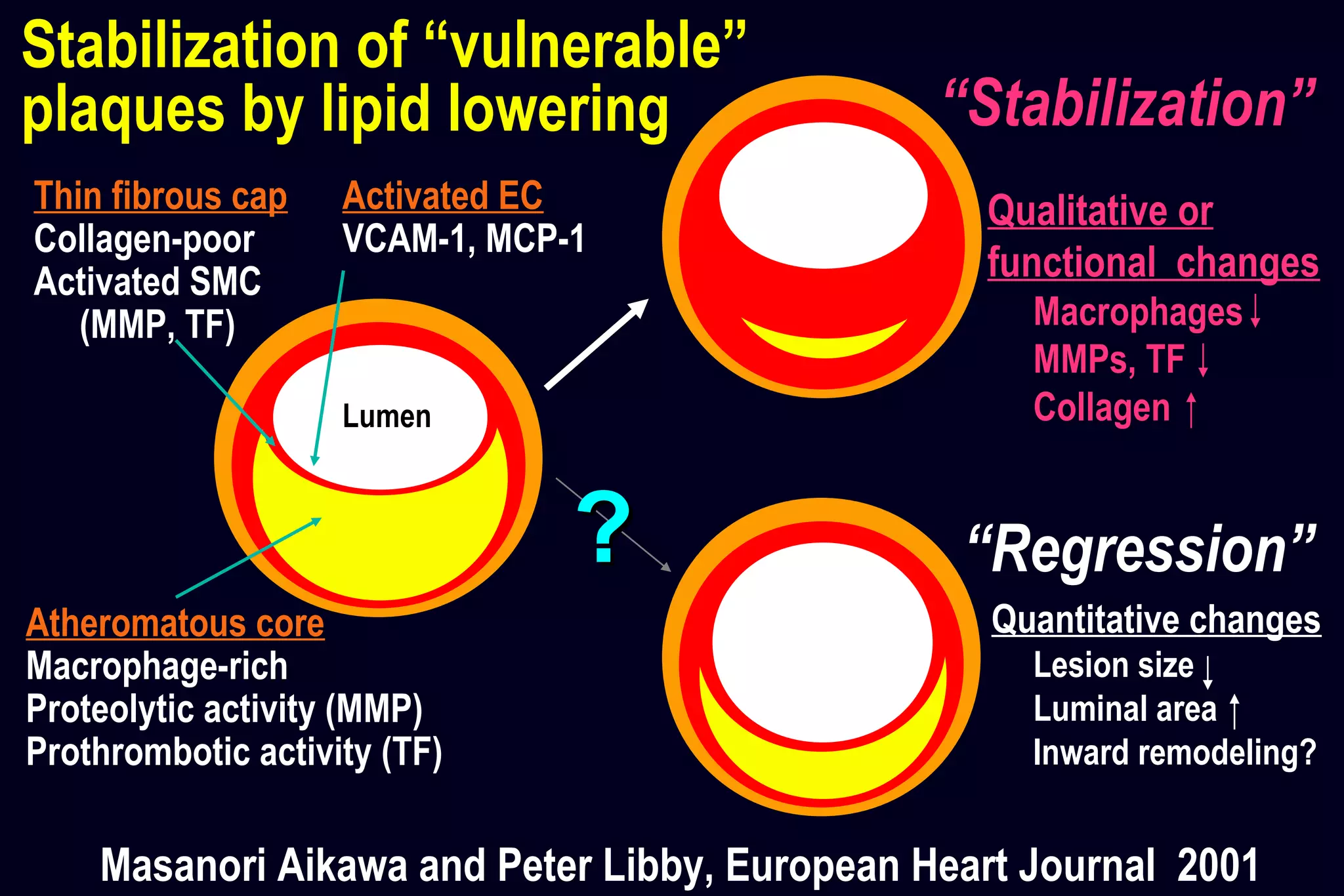
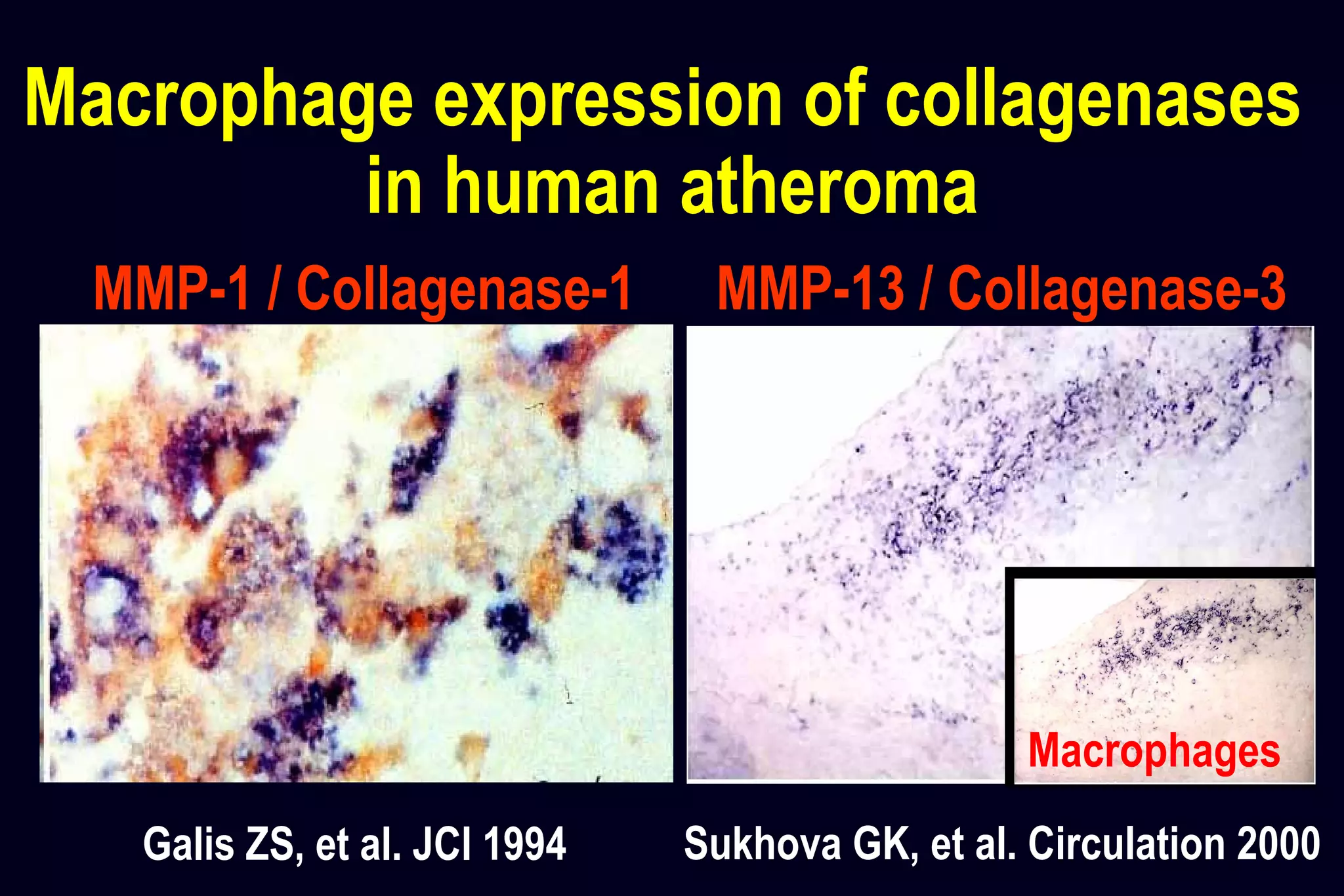
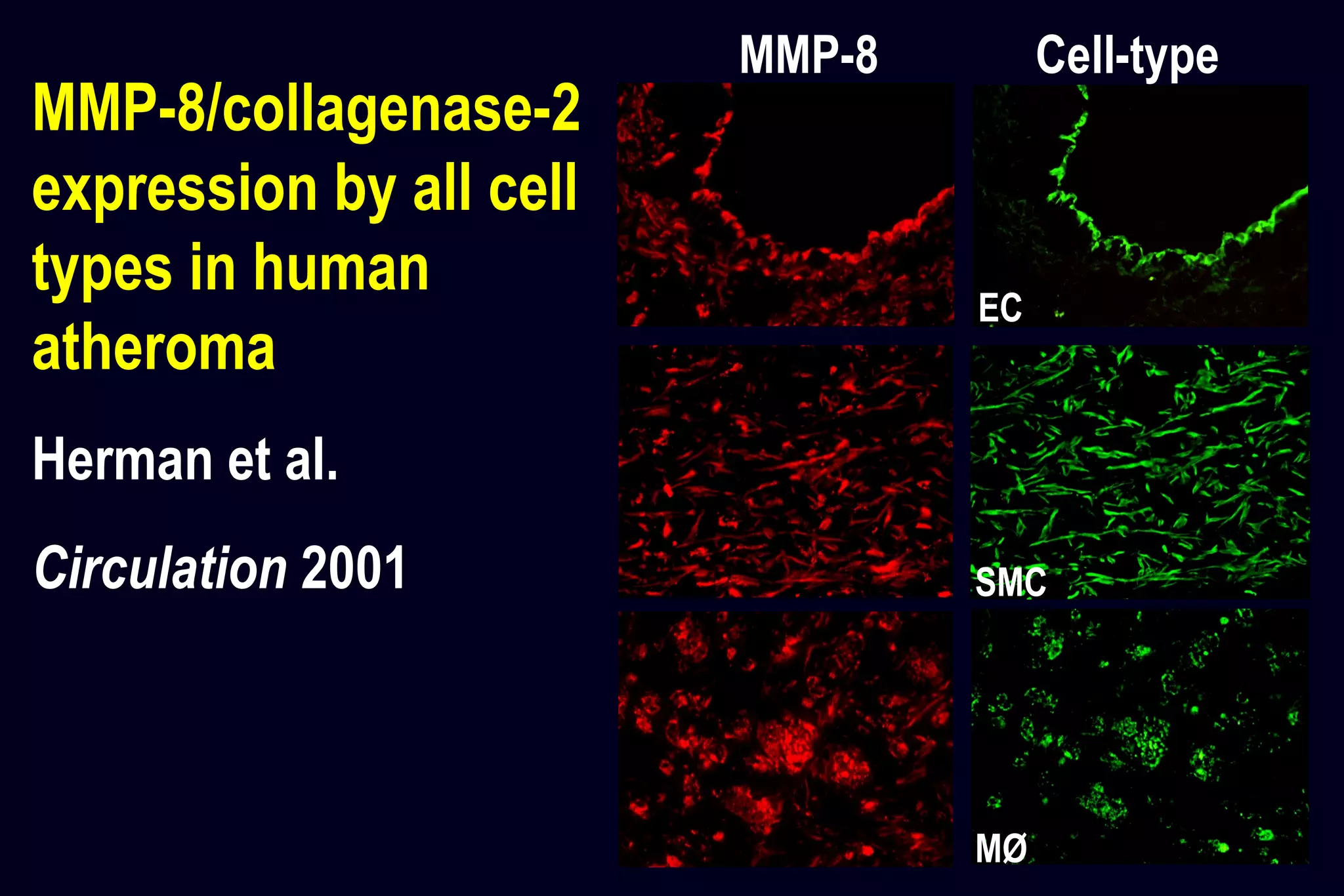
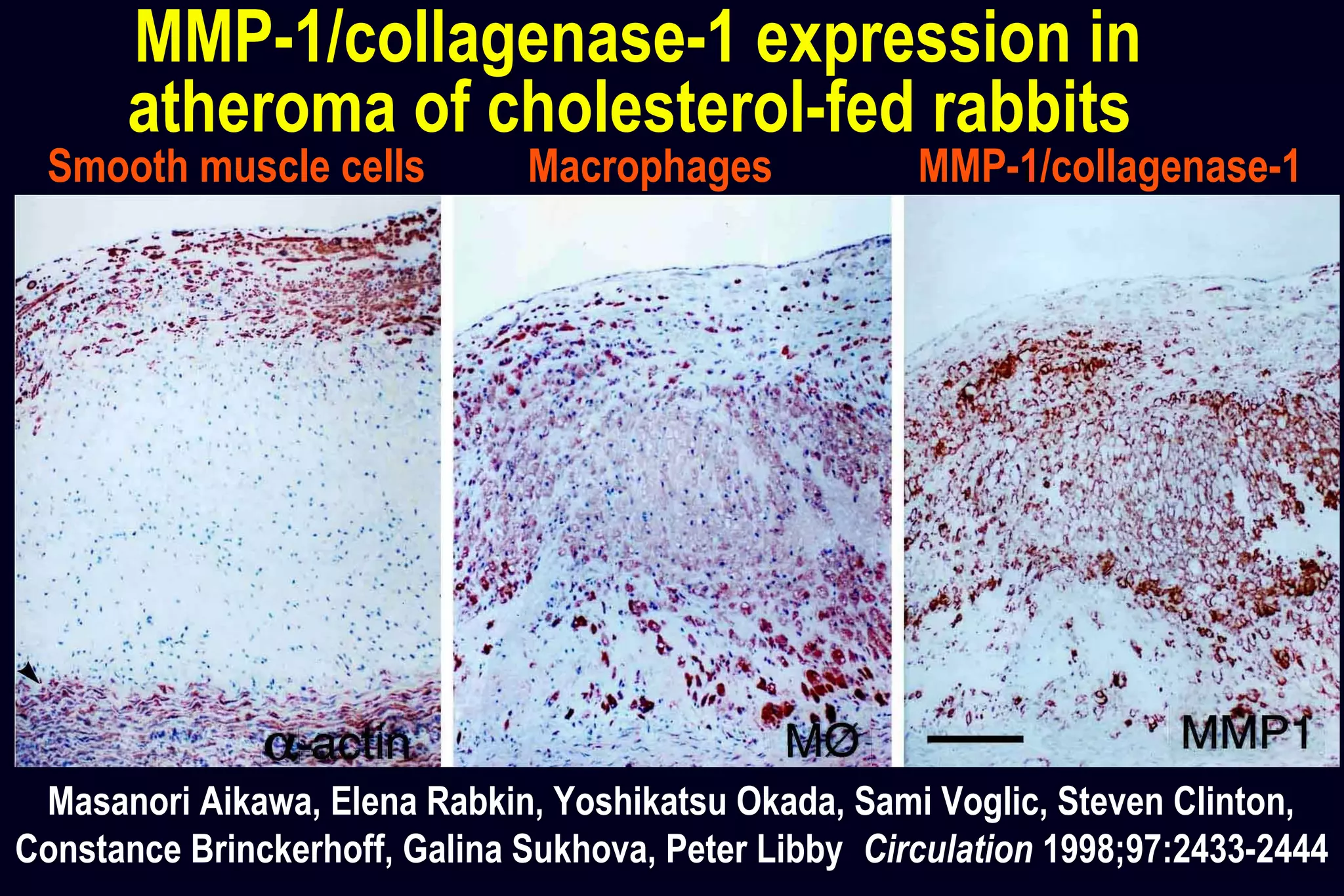
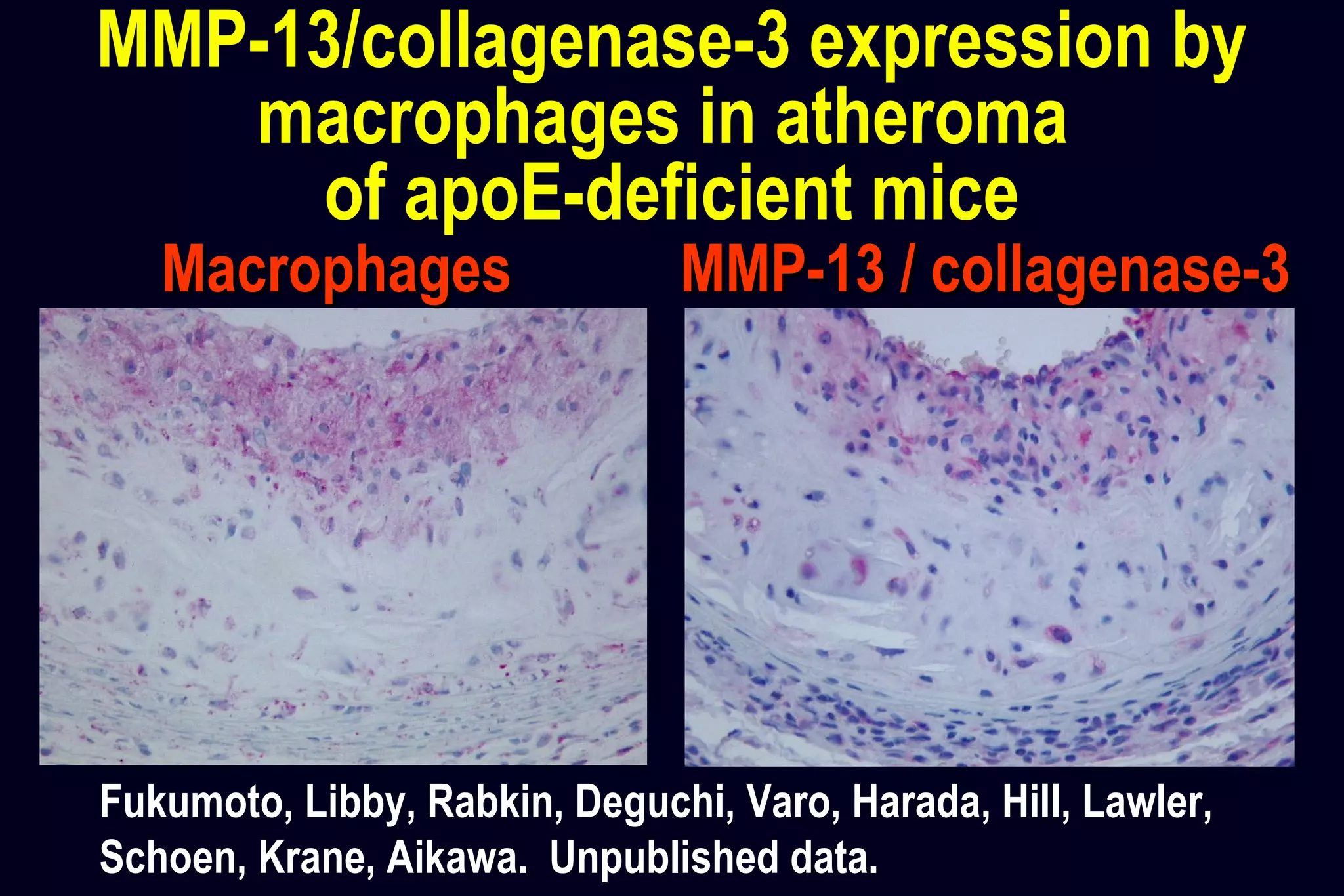
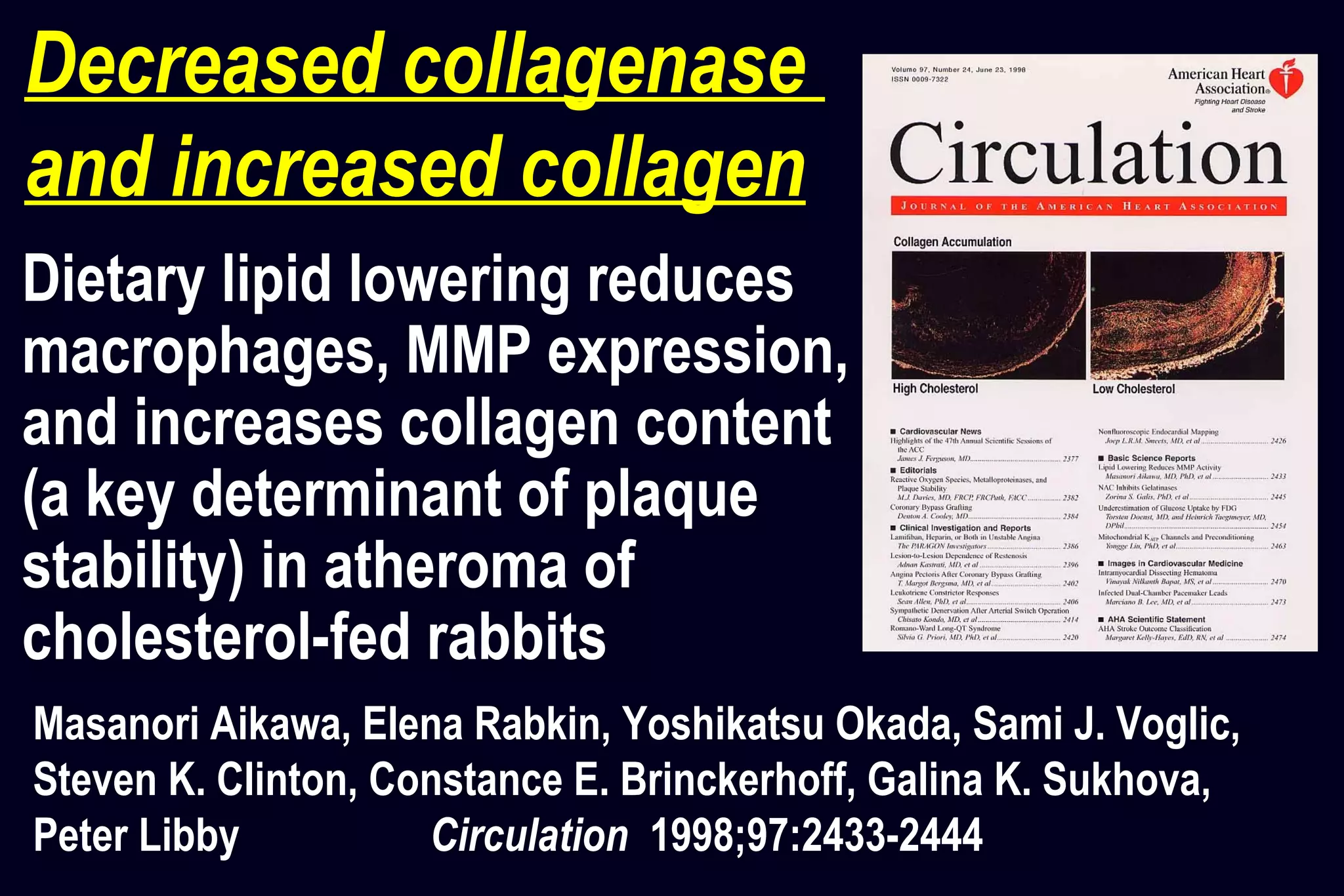
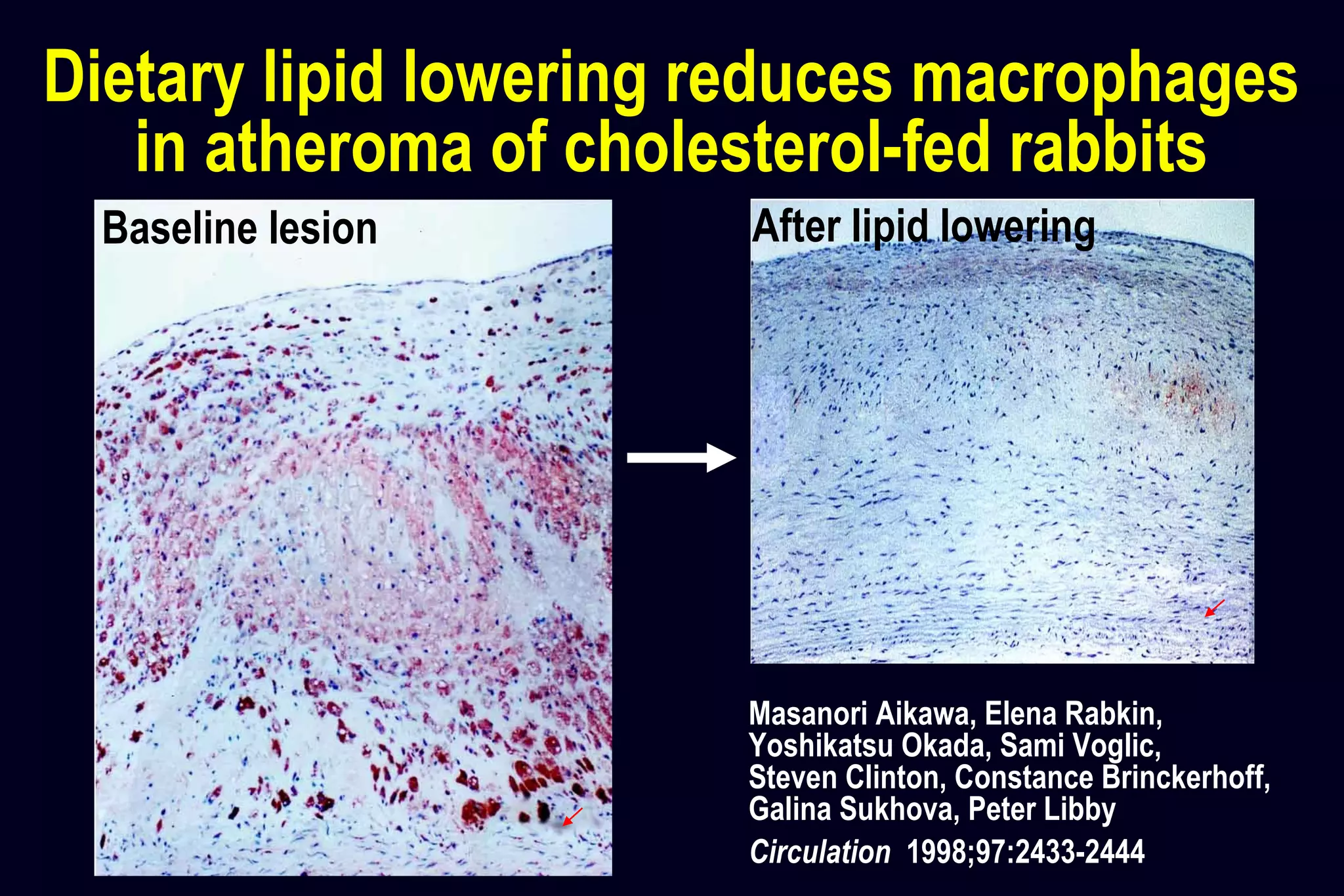
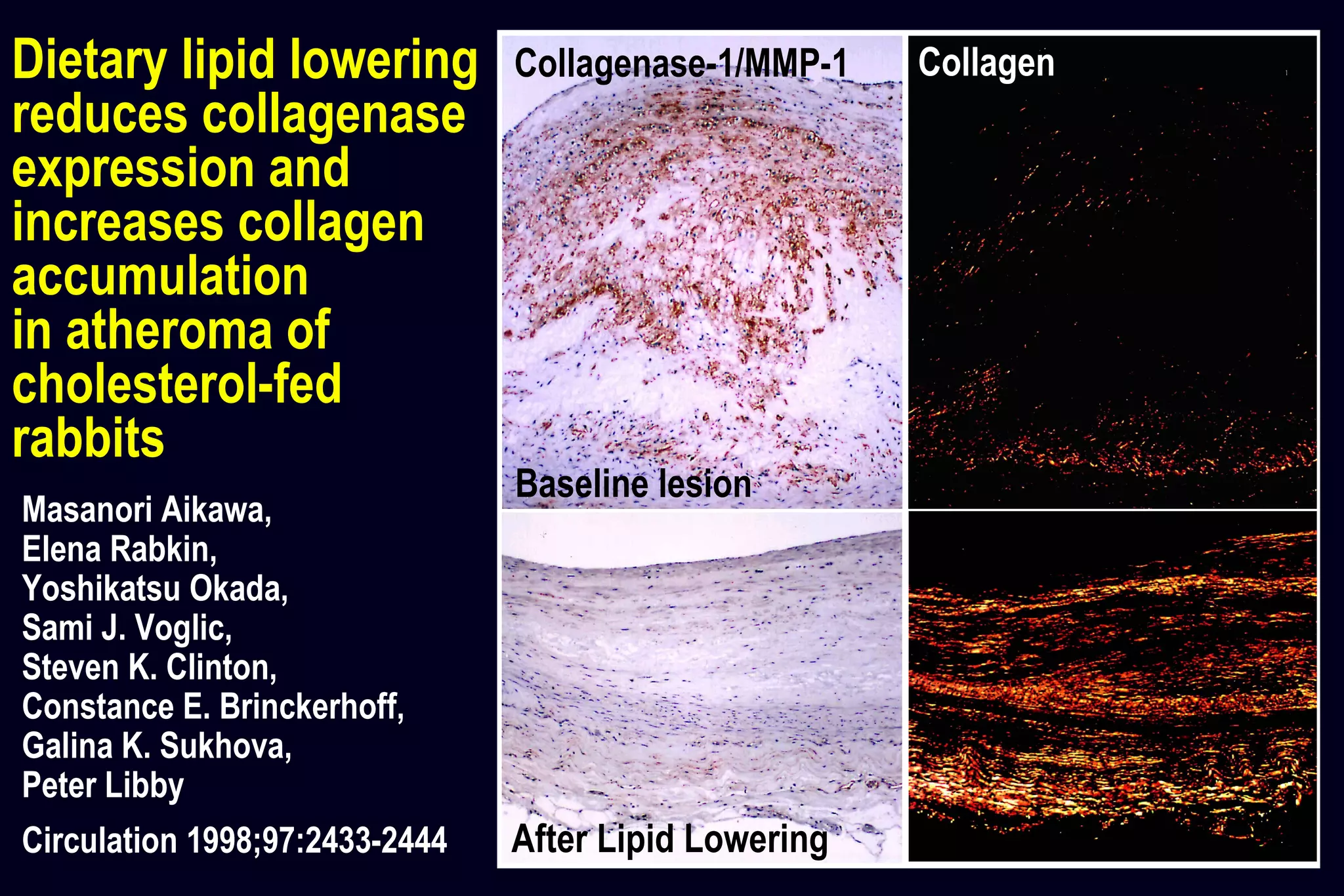
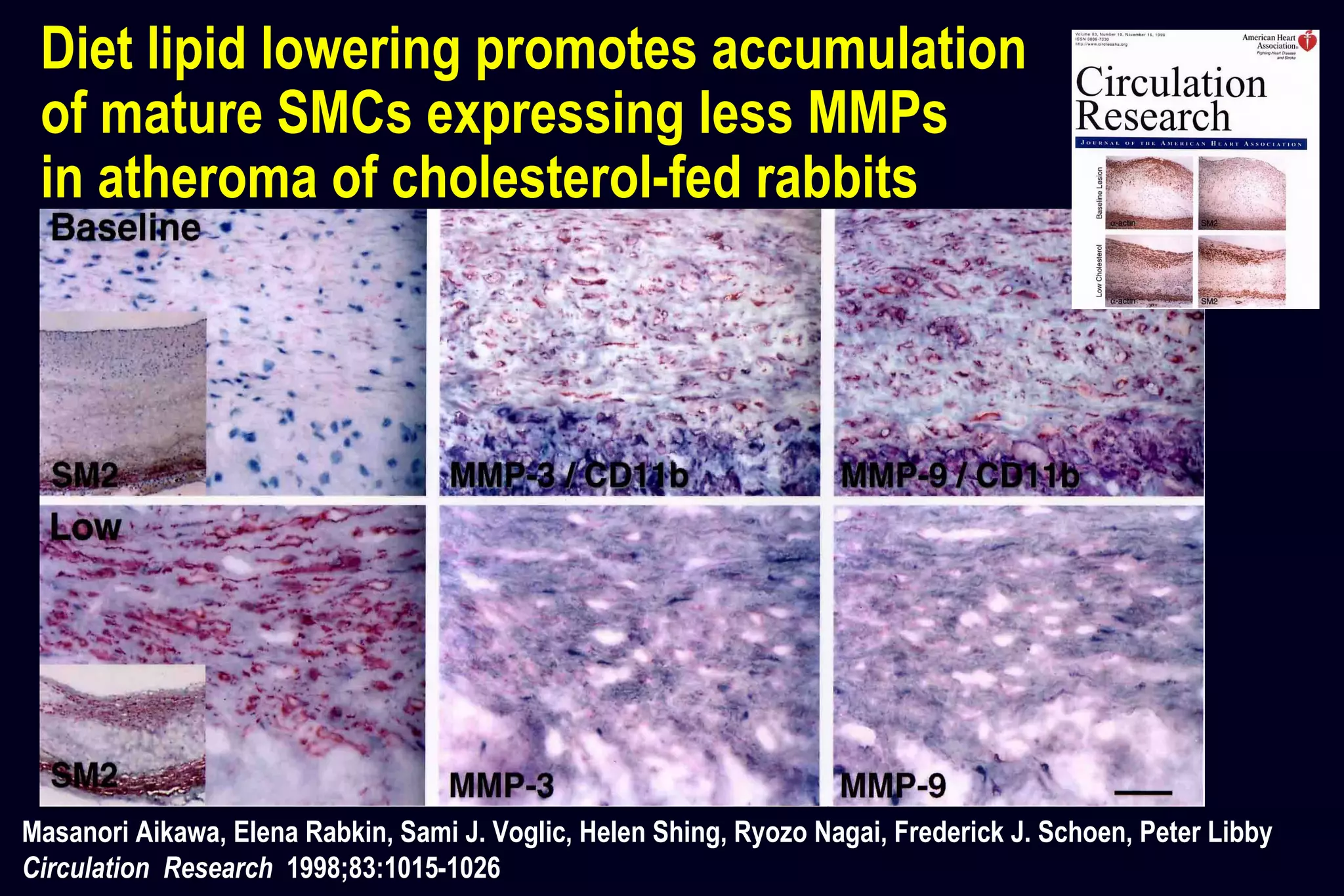
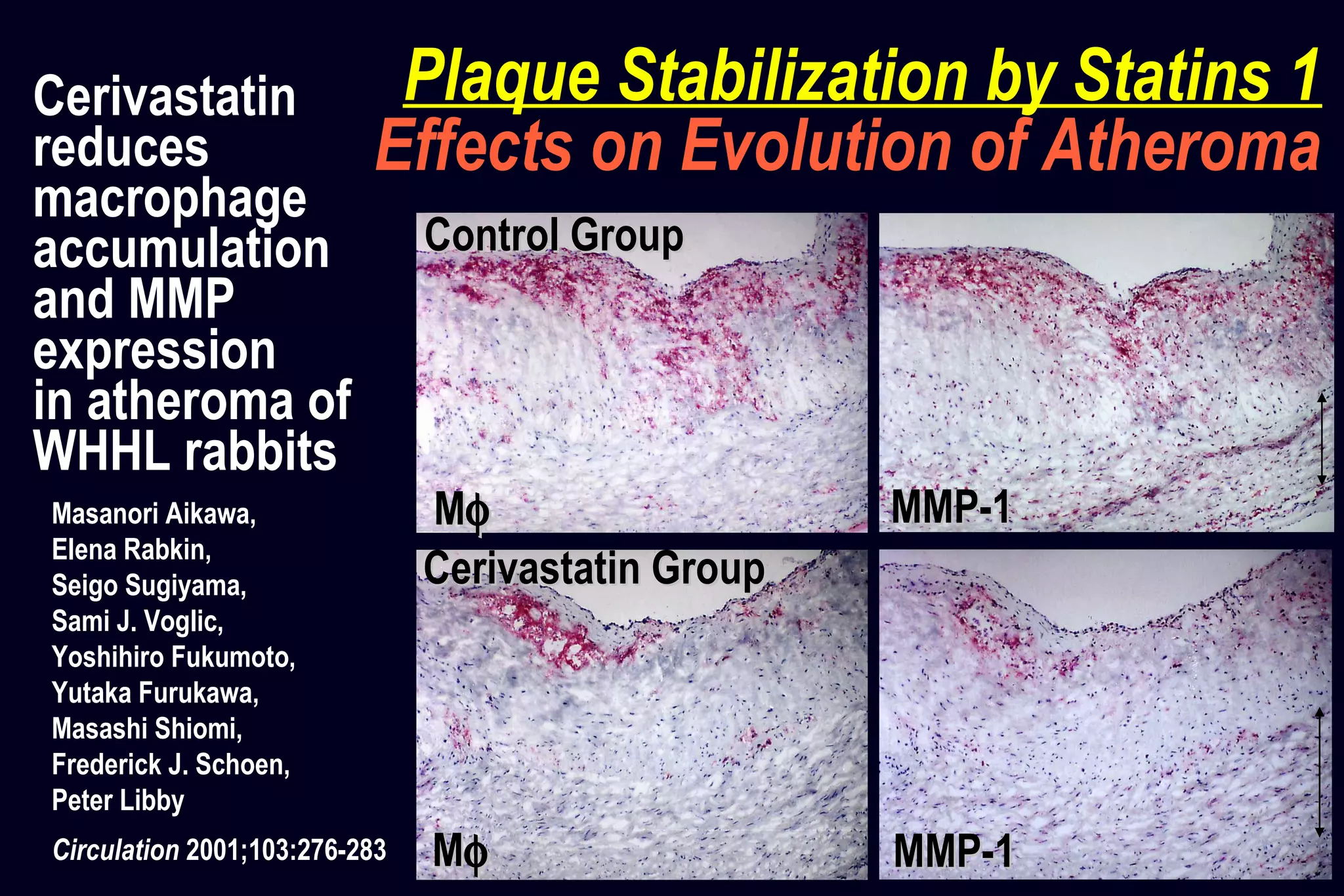
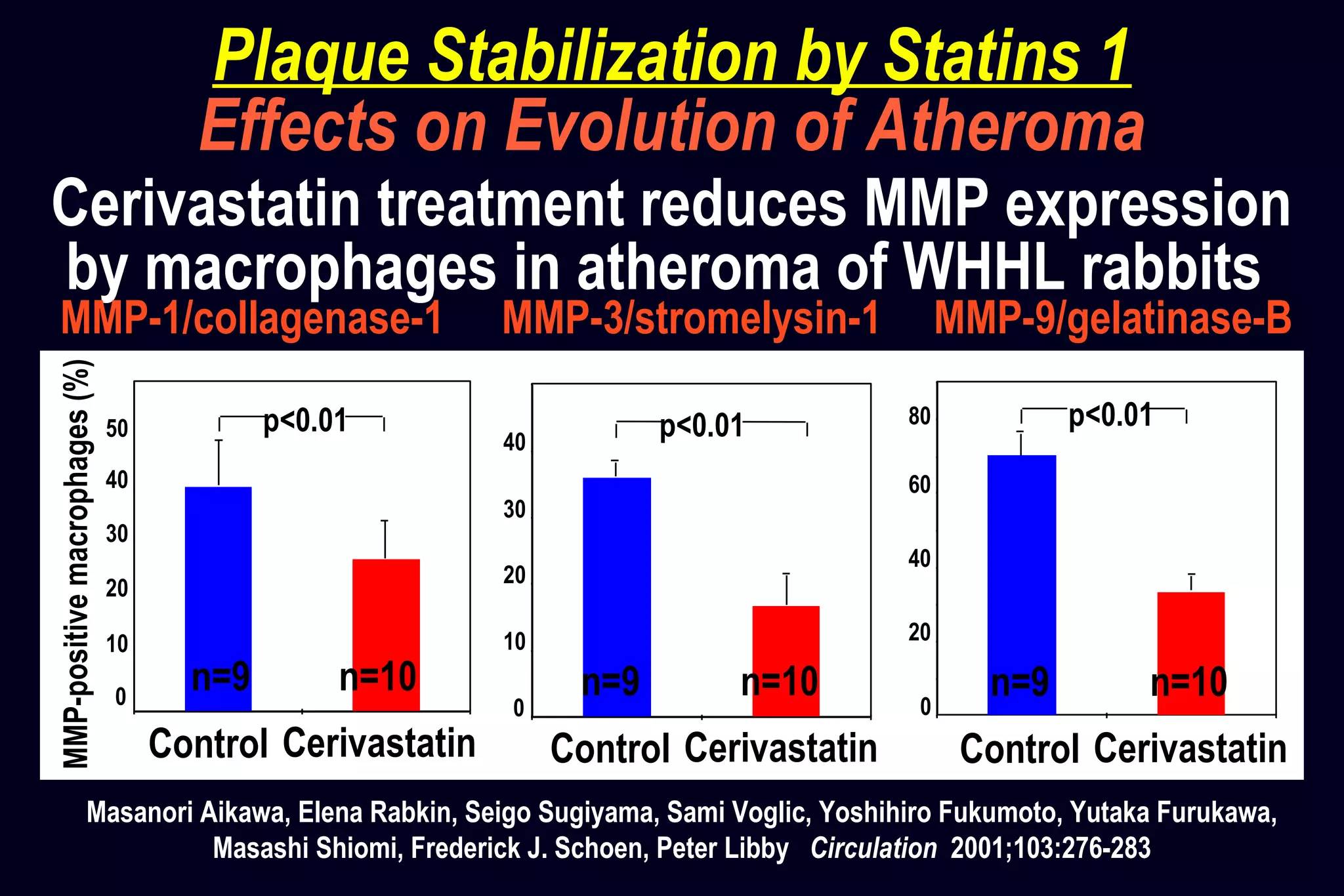
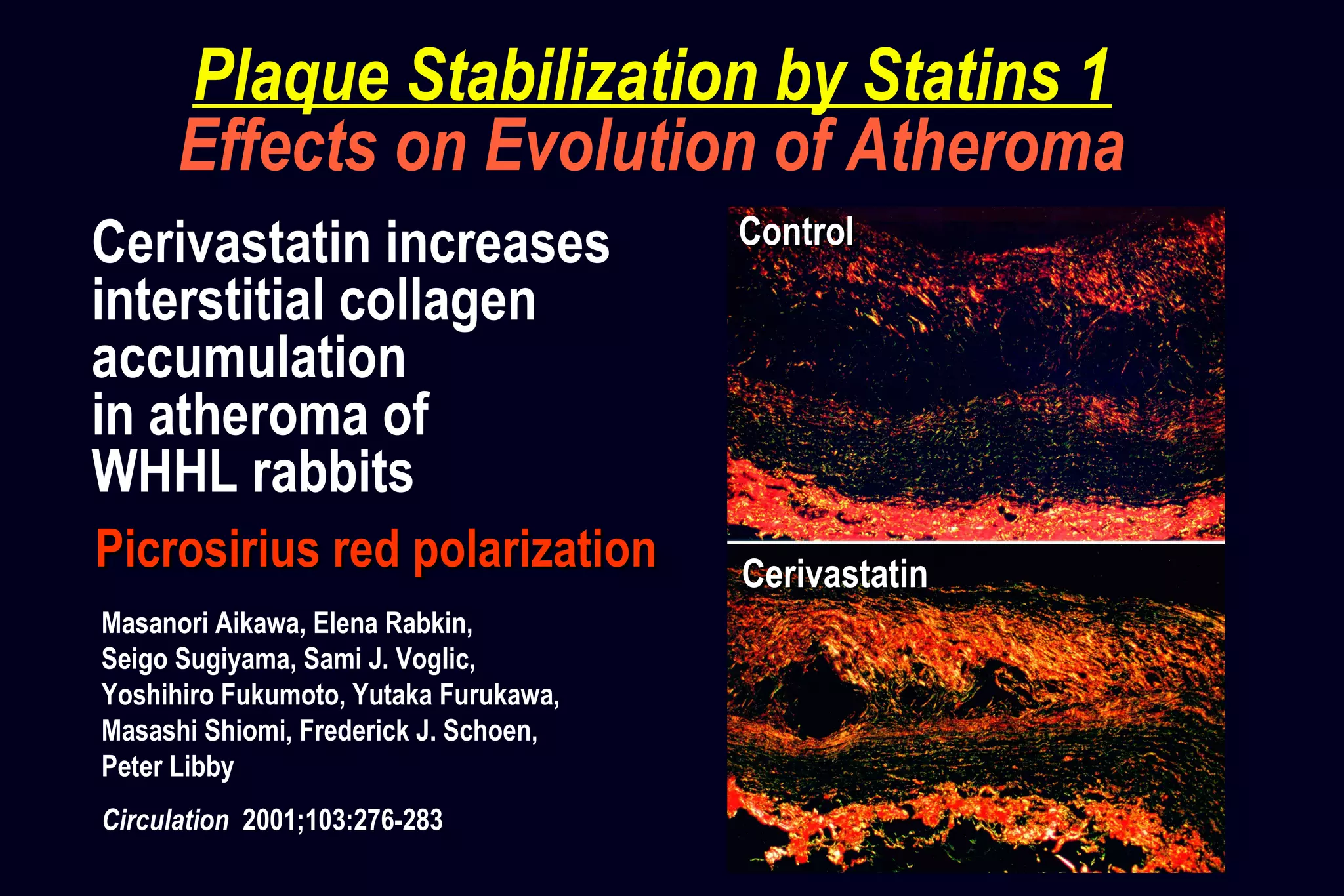
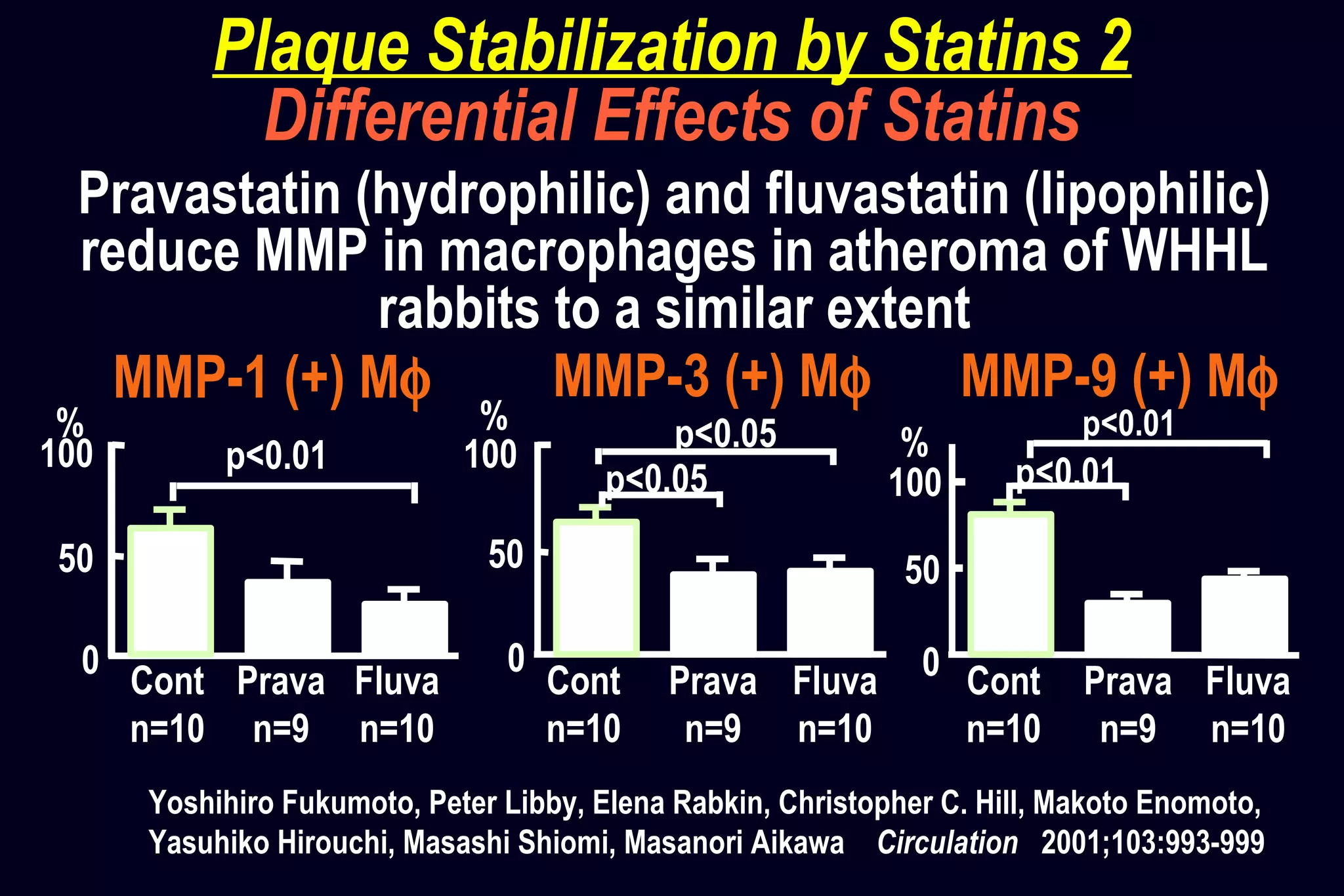
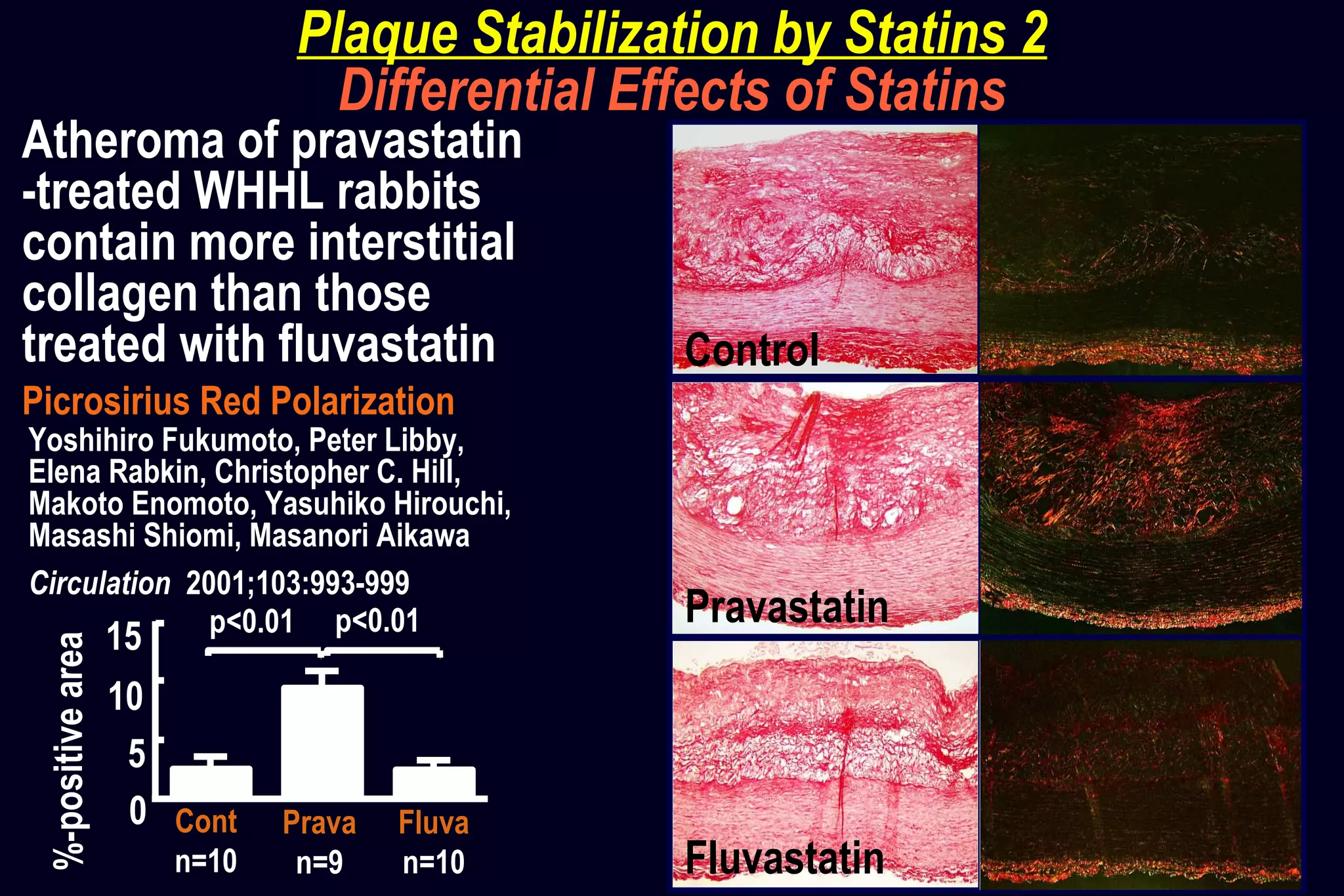
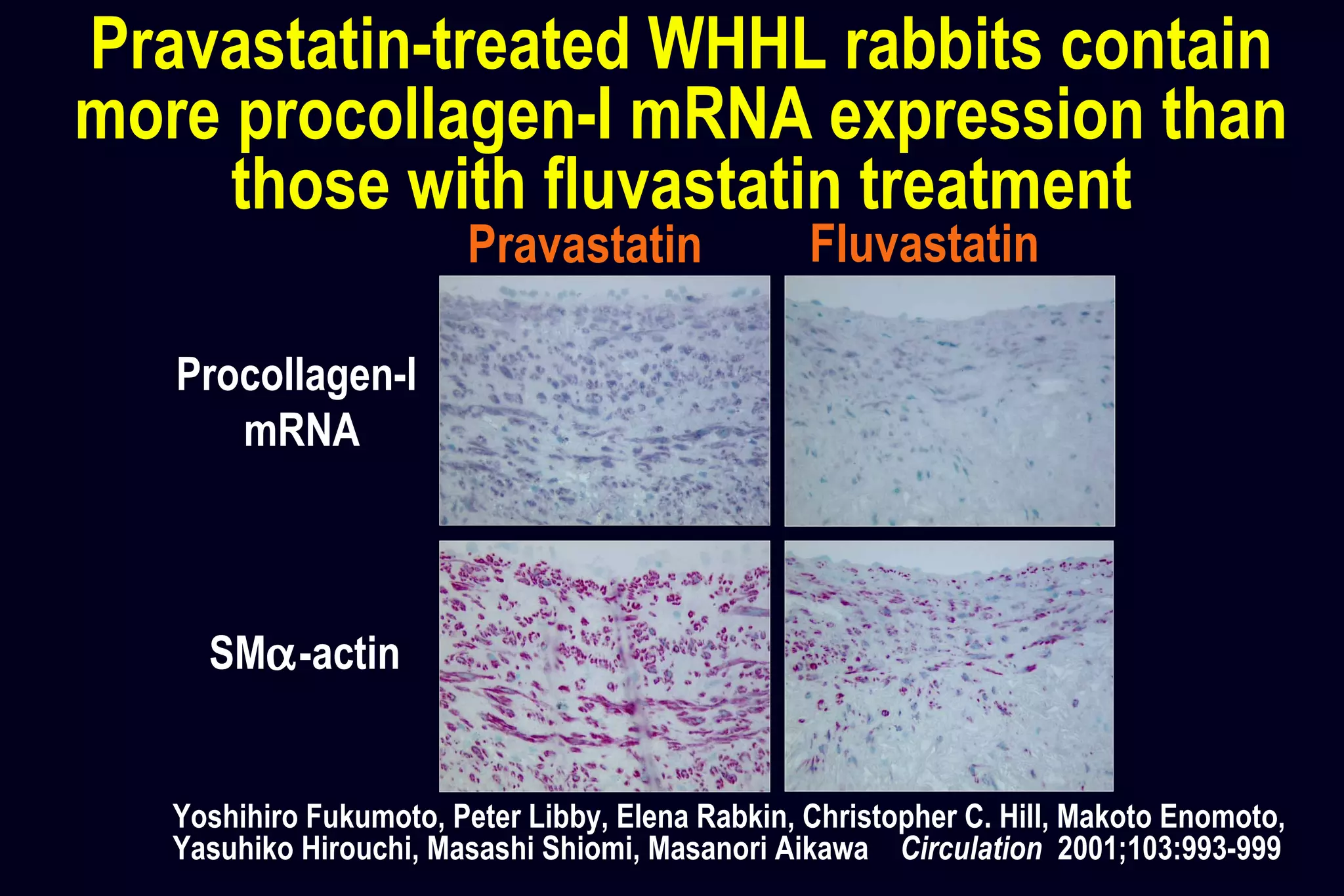
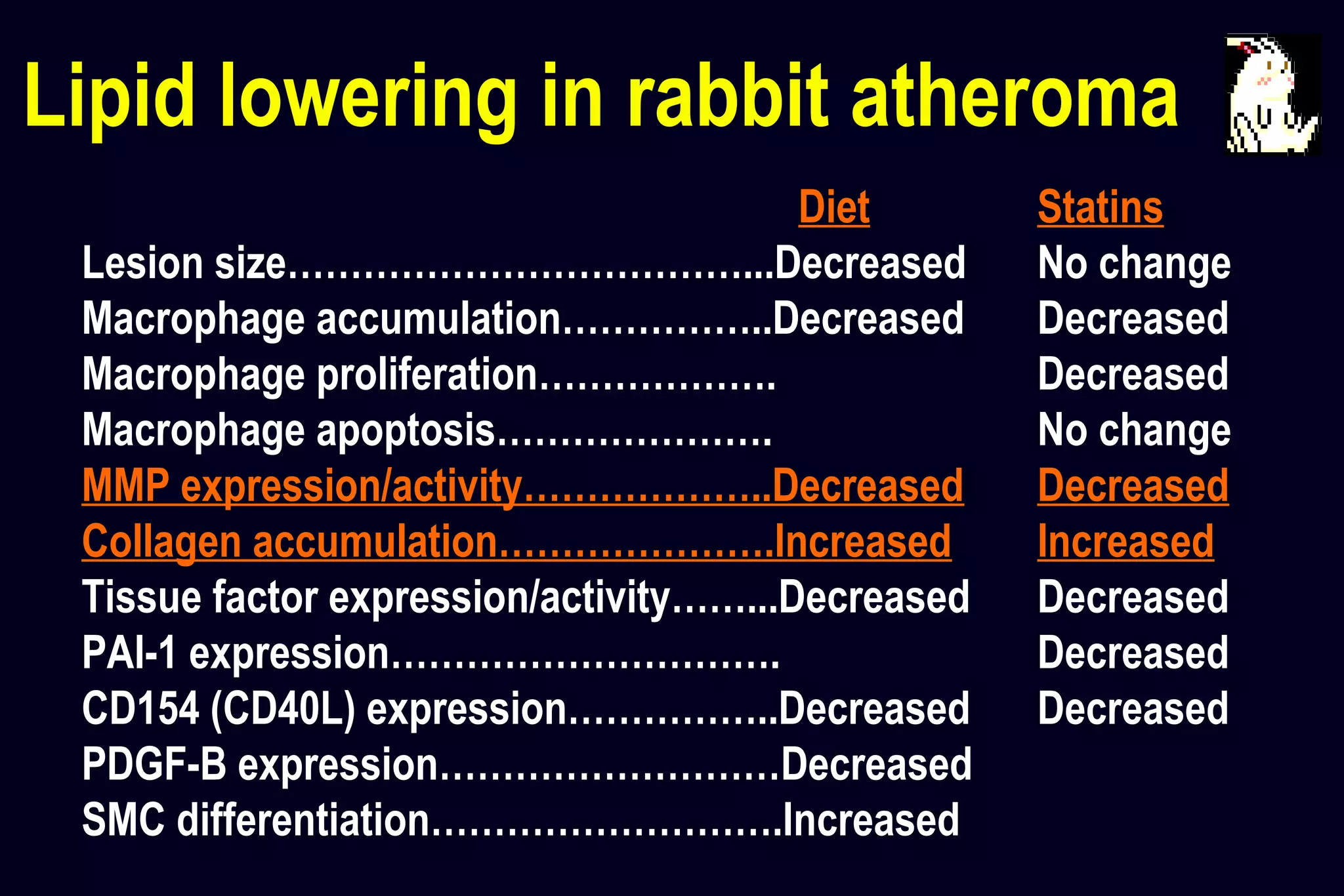
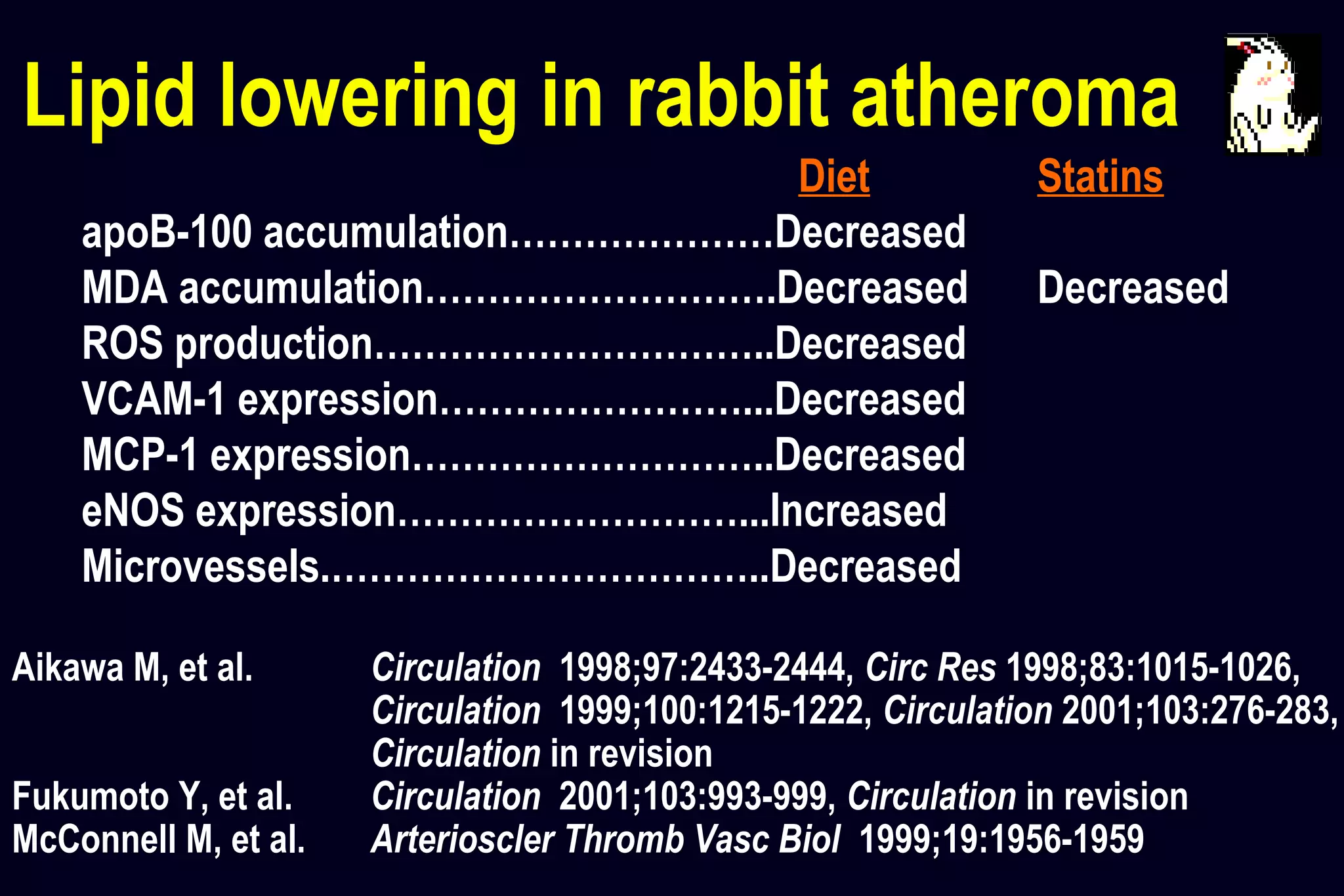
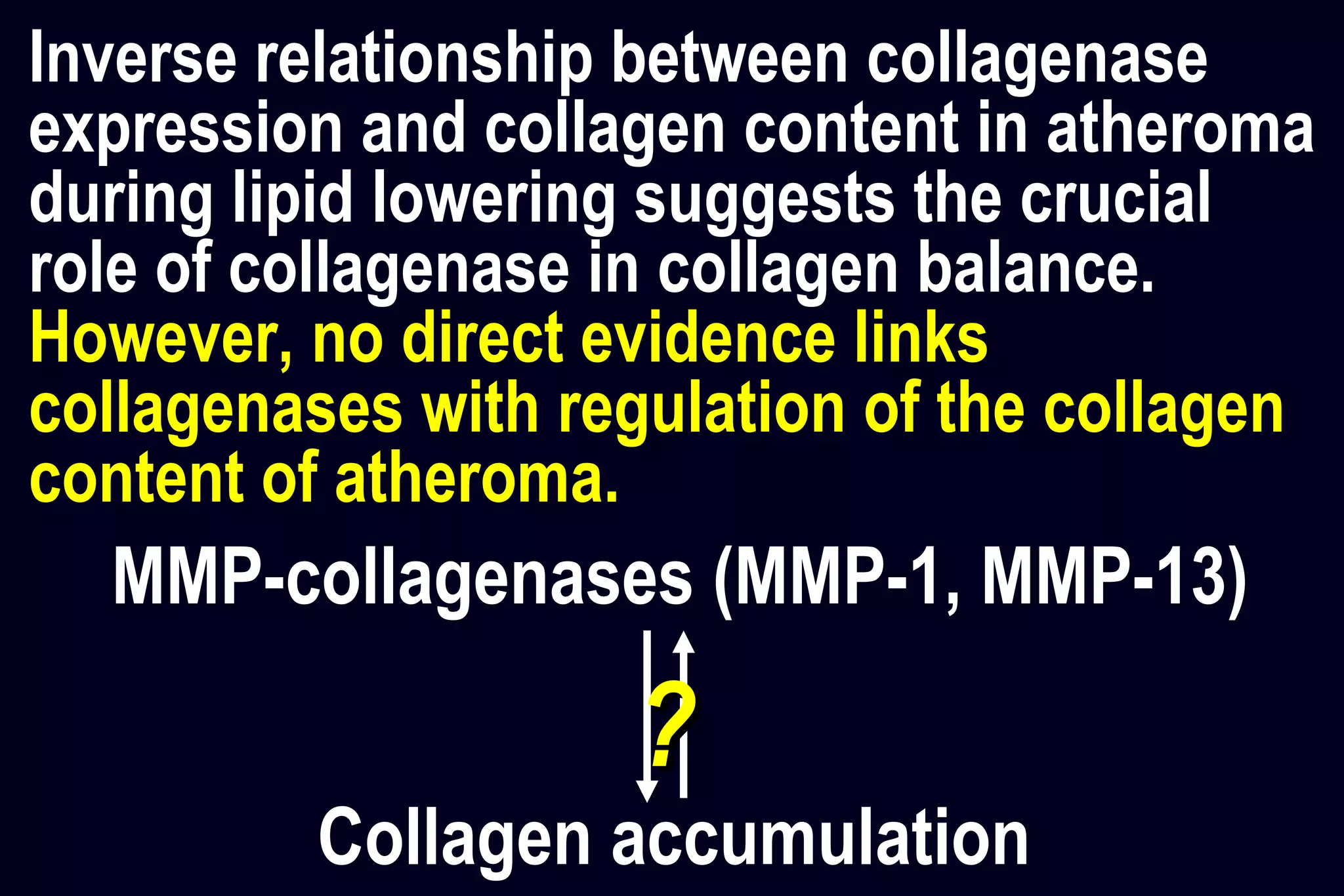
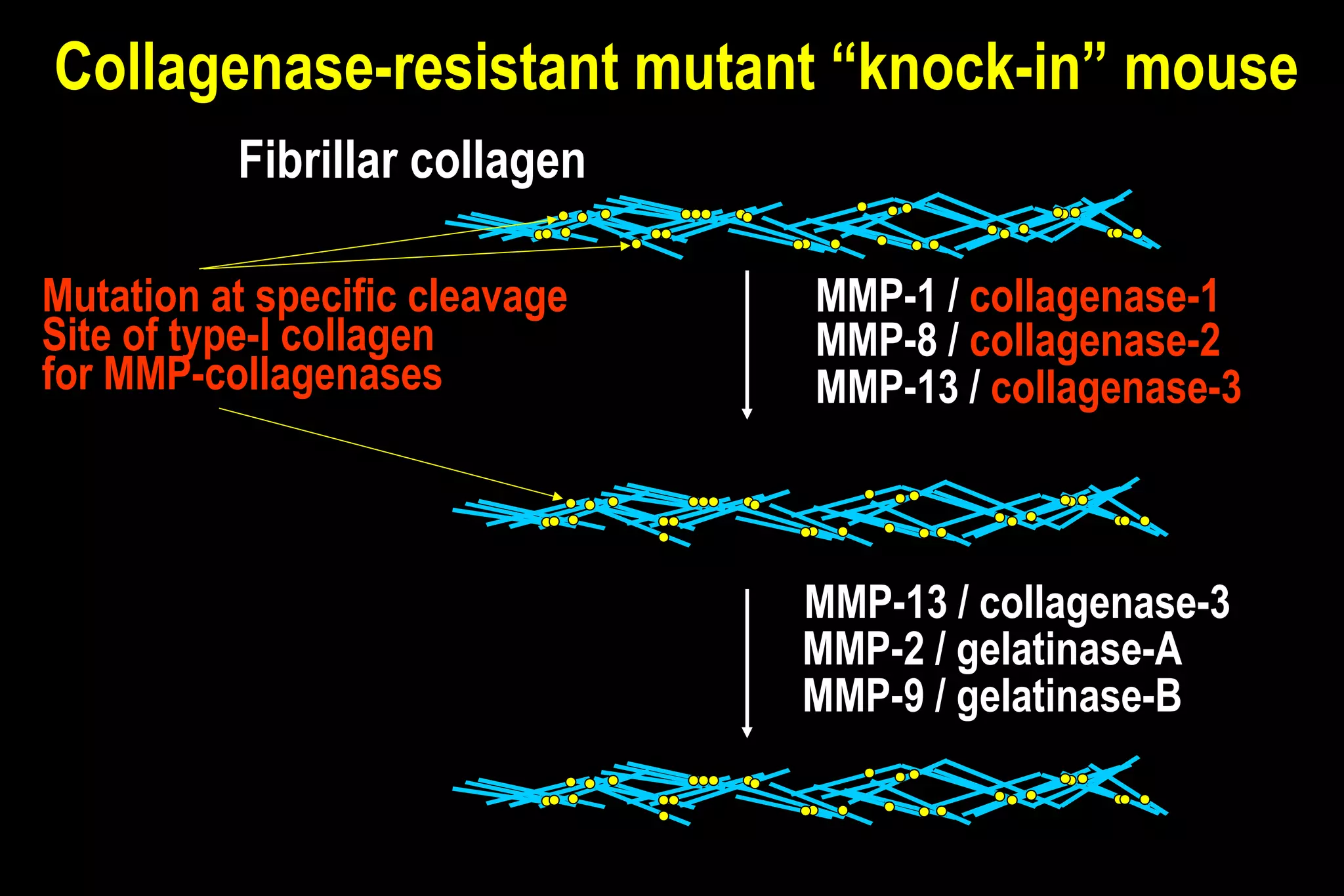
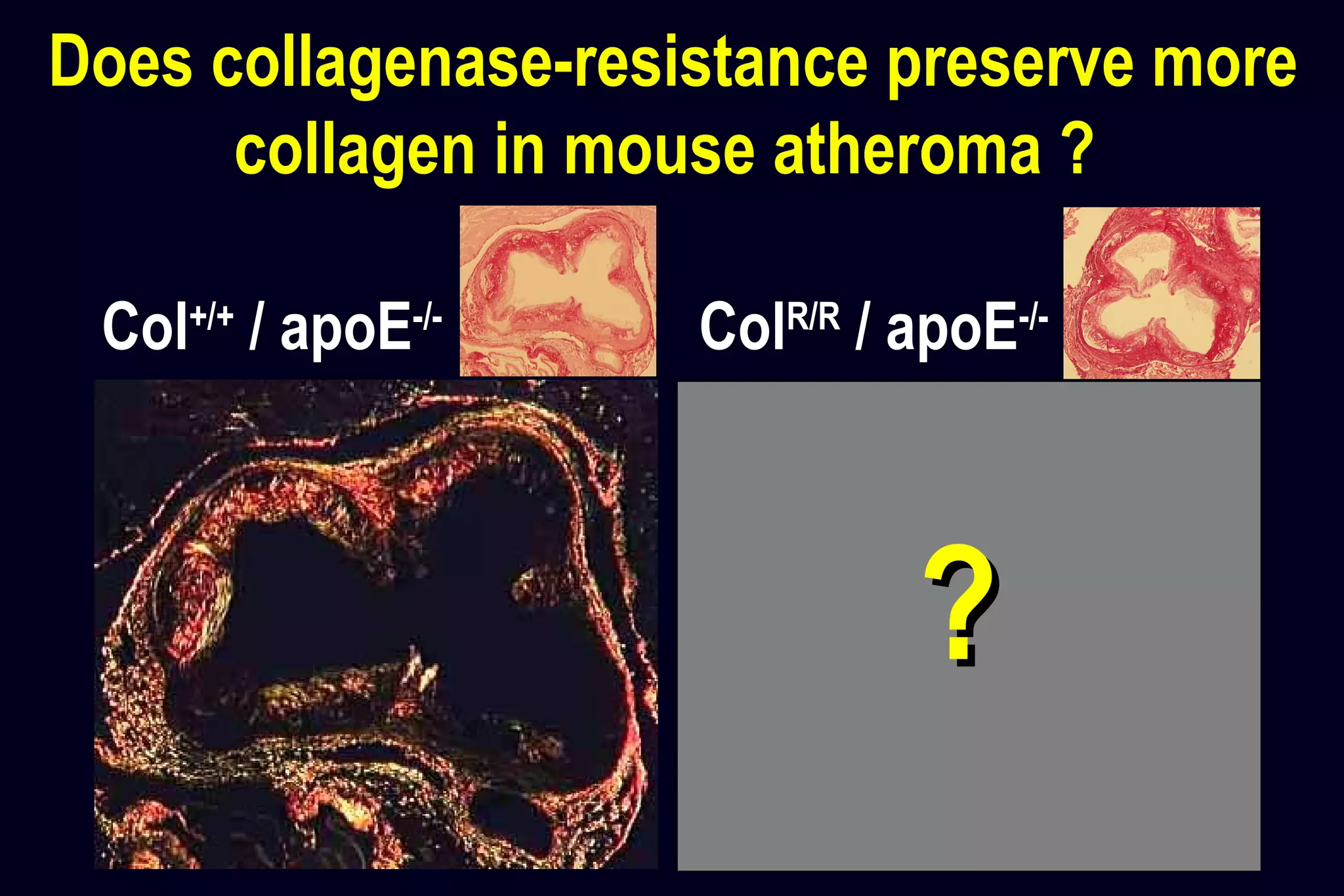
This document discusses research on the roles of collagen and collagenases in atherosclerotic plaque vulnerability. It presents several hypotheses: 1) that human and experimental plaques contain collagenases, 2) that lipid lowering improves features associated with vulnerability by reducing macrophages and collagenase expression while increasing collagen, and 3) that collagenolysis regulates collagen accumulation in plaques of genetically altered mice. Several studies are described that provide evidence supporting these hypotheses, showing that collagenases are expressed in human and animal plaques, lipid lowering reduces vulnerability features in rabbits, and collagenase-resistant mice have altered collagen content in plaques. The research suggests collagenases play a critical role in plaque collagen metabolism and vulnerability.