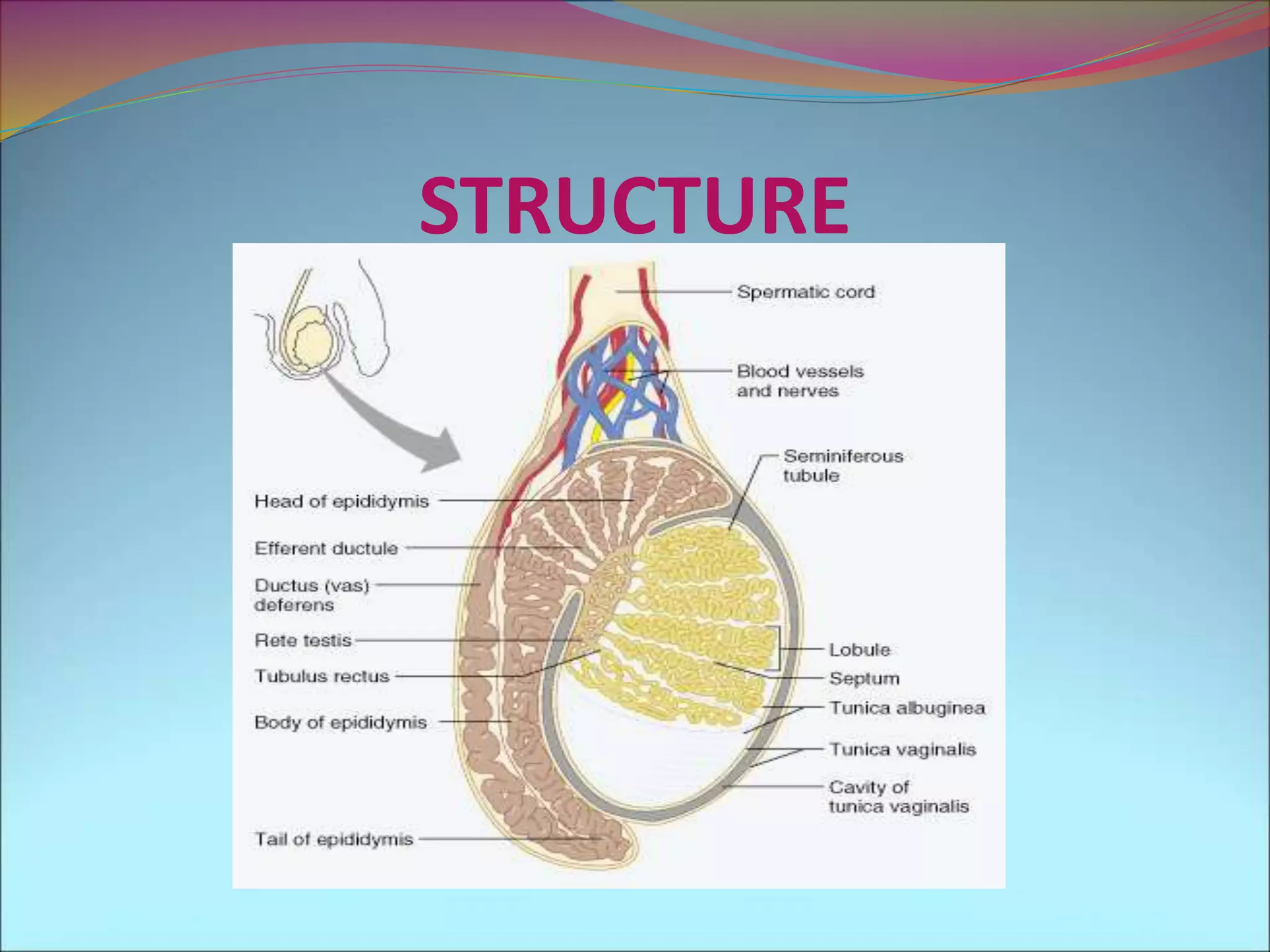
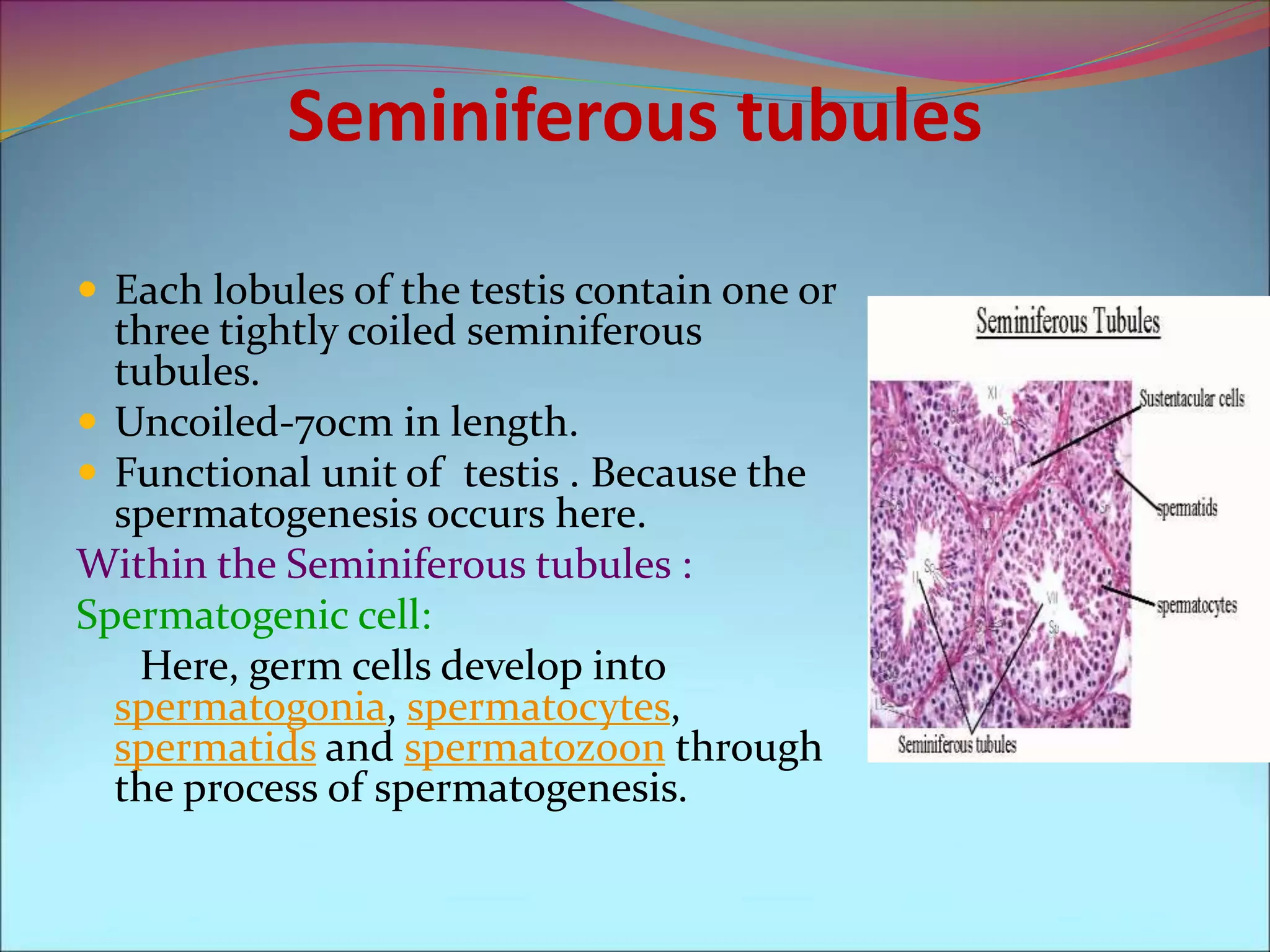
The document provides an overview of the male testis, detailing its embryonic development, anatomy, and functions as both an exocrine and endocrine gland. Key components include seminiferous tubules where spermatogenesis occurs, the supportive role of Sertoli and Leydig cells, and the structural layers of the scrotum. It also explains the hormonal influences during development and the descent of the testes into the scrotum.