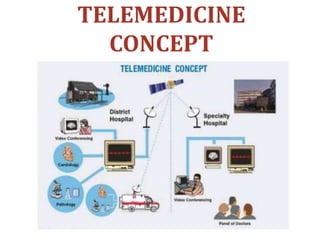
Telemedicine involves using telecommunication technologies to provide remote clinical healthcare. It overcomes barriers of distance and improves access to services for rural communities. There are three main types: interactive medicine with real-time communication between doctors and patients; remote patient monitoring using mobile devices; and store-and-forward sharing of health information. The first telemedicine system was set up in 1967 between Boston and Massachusetts. Telemedicine has advanced healthcare access and has limitations such as technical issues and state laws restricting access to out-of-state doctors.