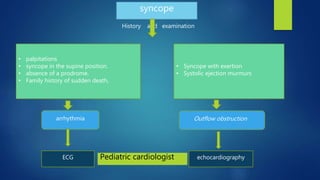
This document discusses syncope (fainting), including its definition, causes, pathophysiology, history and examination, investigations, and treatment. Syncope is defined as a sudden, transient loss of consciousness due to cerebral hypoperfusion. It can be caused by neurological, cardiovascular, orthostatic hypotension, or other factors like anemia or hypoglycemia. Evaluation involves taking a history of symptoms and potential triggers, physical exam including orthostatic vital signs, ECG, echocardiogram if needed, and lab tests like glucose and electrolytes. Treatment depends on the identified cause, and may include rehydration, non-pharmacological approaches, or referral to a cardiologist for potential arr