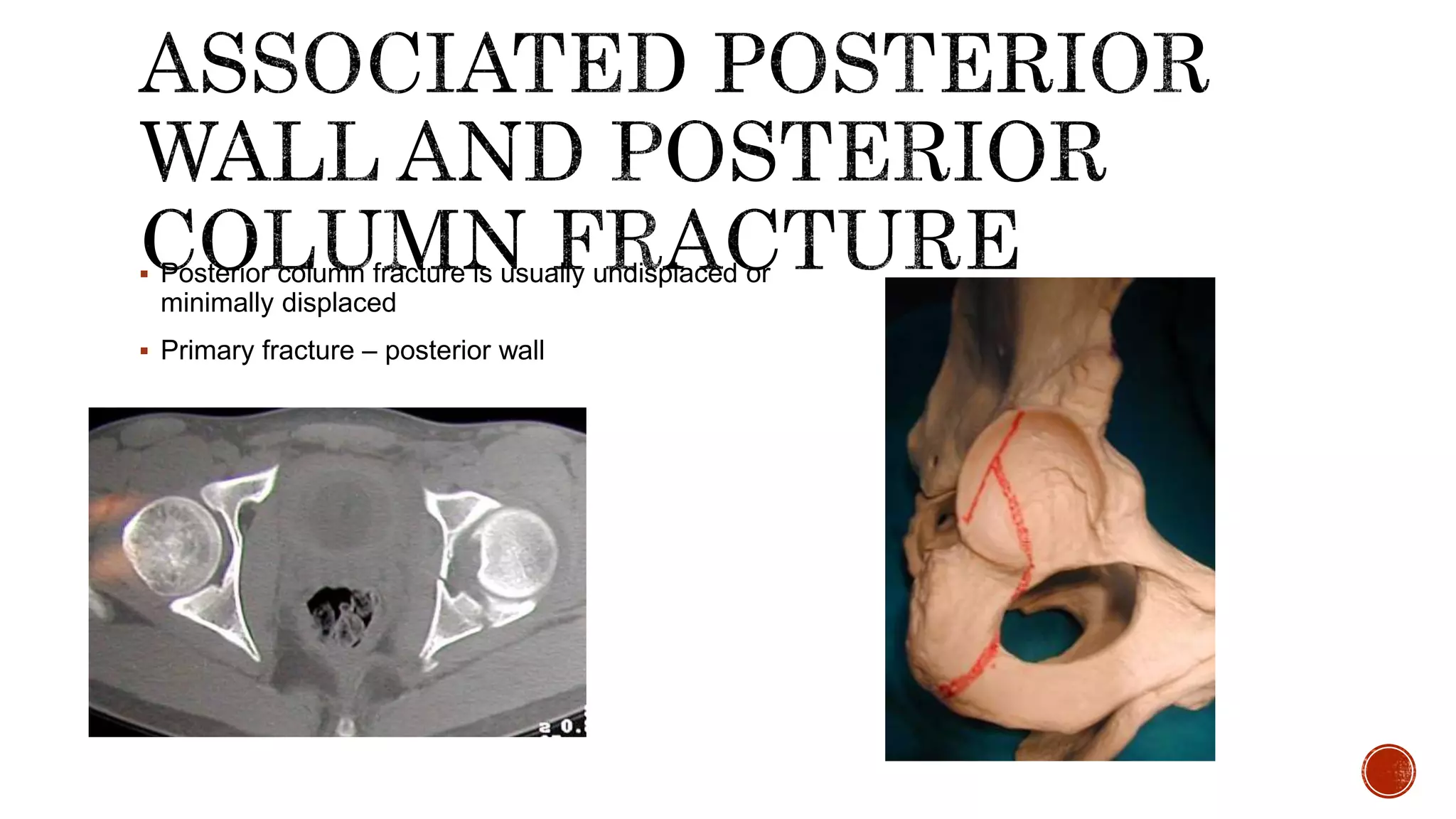
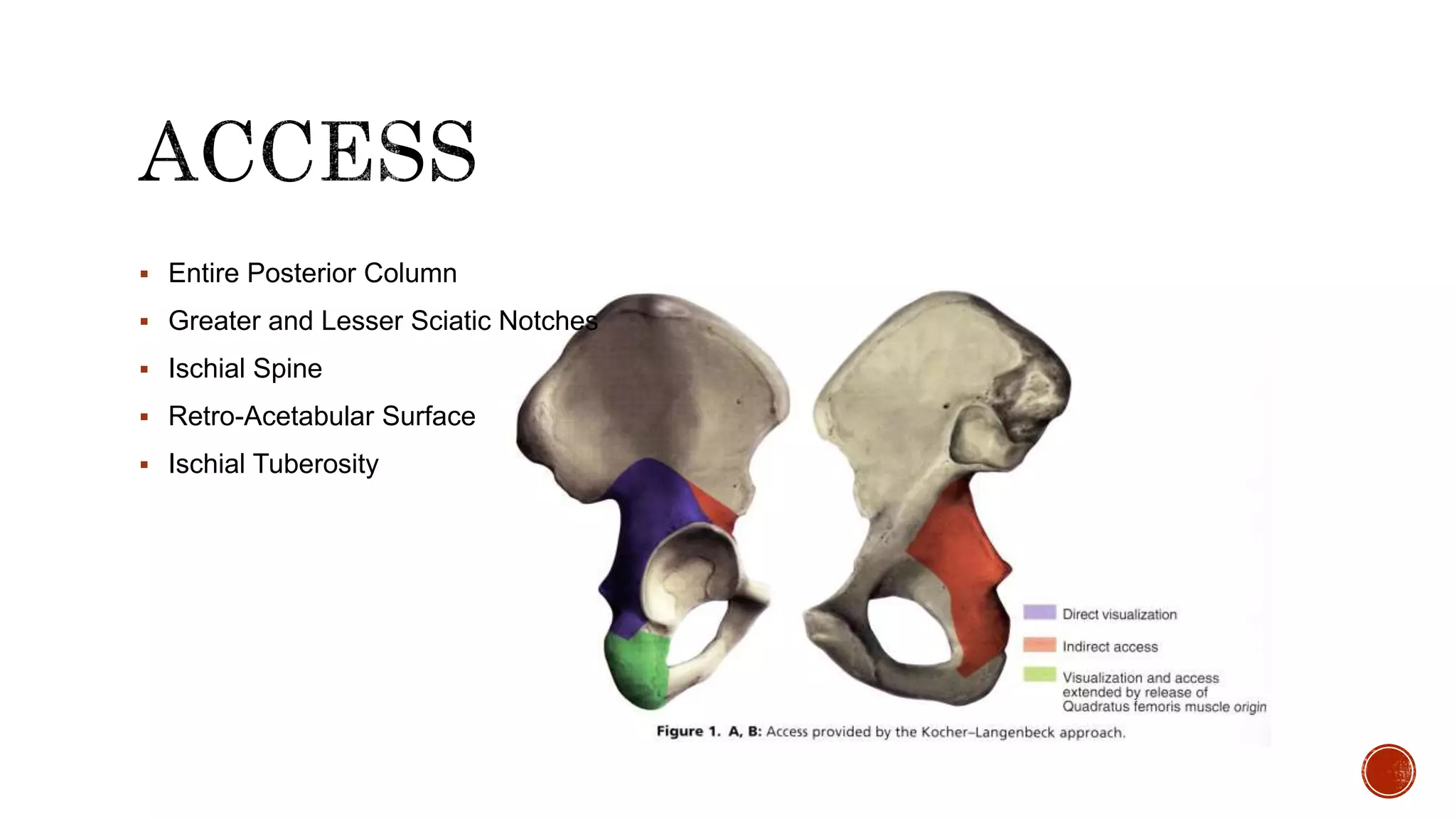
This document describes the anatomy and classification of acetabular fractures, as well as surgical approaches for treating different types of acetabular fractures. It discusses the Kocher-Langenbeck and Stoppa approaches for posterior and anterior fractures, respectively. Key points include that acetabular fractures can be classified into 5 simple and 5 associated fracture patterns, and surgical timing within 3 weeks of injury leads to better outcomes. The document provides details on surgical techniques for each approach.