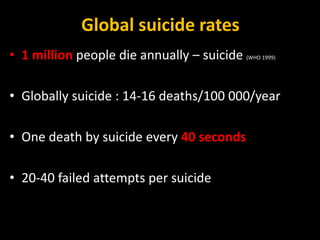
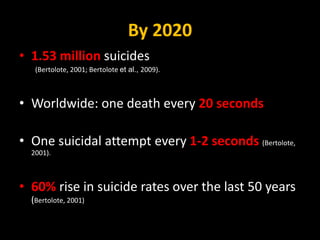
1) Suicide is a major global public health problem, with over 1 million deaths by suicide annually worldwide and rates expected to rise 60% by 2020.
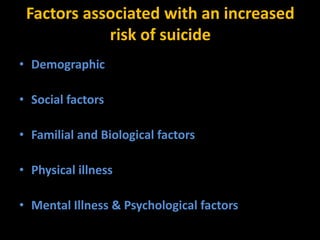
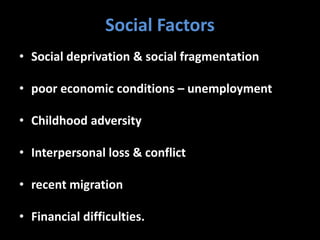
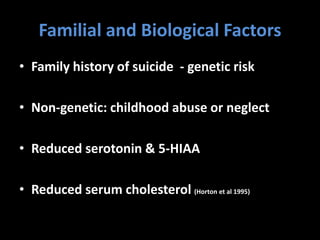
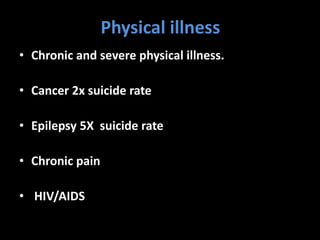
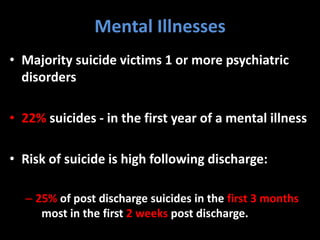
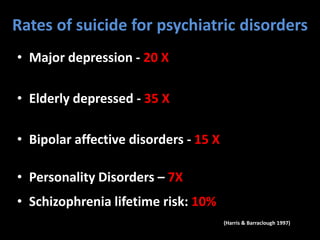
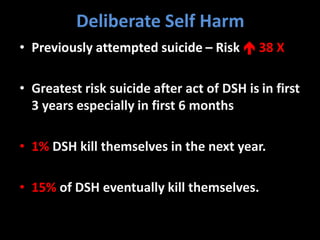
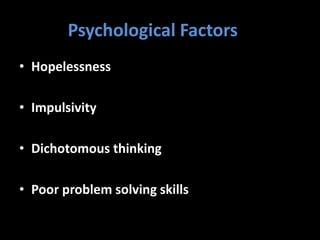
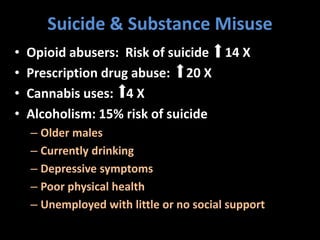
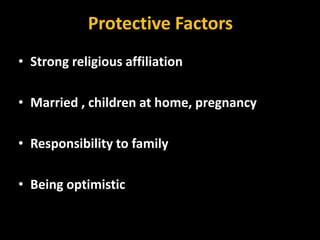
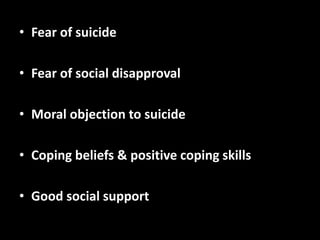
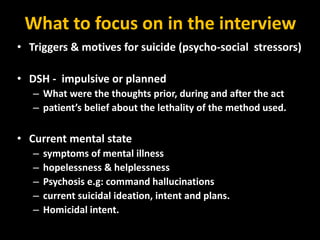
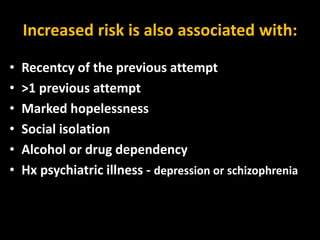
2) Suicide is influenced by numerous interrelated demographic, social, familial, biological, physical health, mental health, and psychological factors. Those with a previous suicide attempt, mental illness such as depression, or substance abuse disorder are especially at high risk.
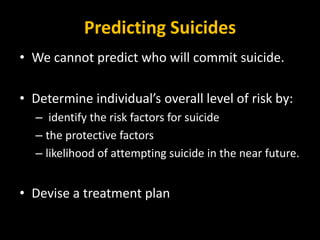
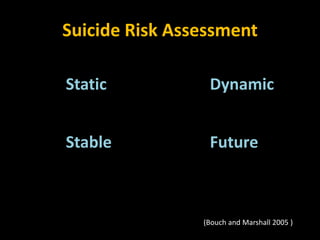
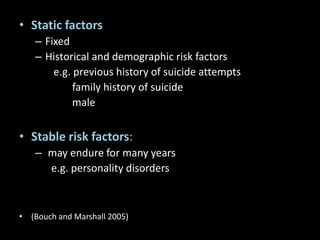
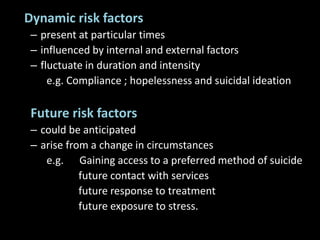
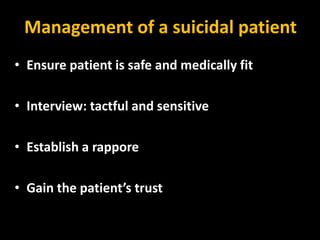
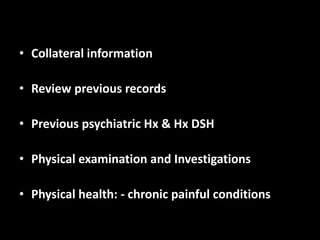
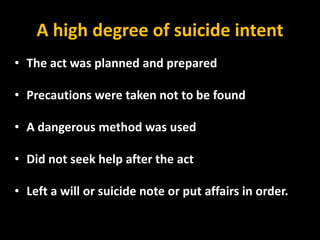
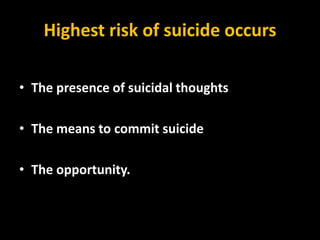
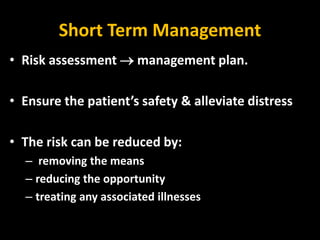
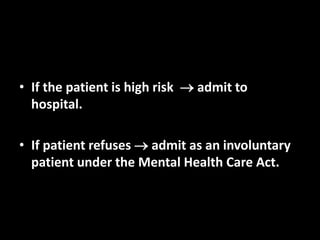
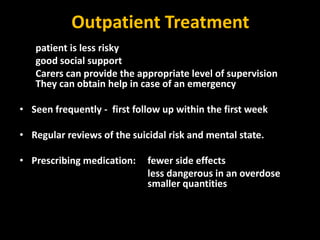
3) A thorough suicide risk assessment considers both static historical factors and dynamic current factors to determine level of risk and devise a treatment plan, with the highest risk periods being when suicidal thoughts, means, and opportunity coincide. For high-risk patients, hospitalization may be required for safety.