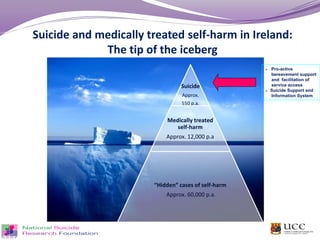
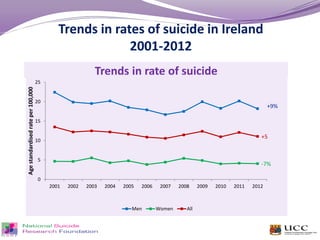
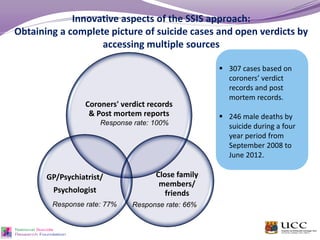
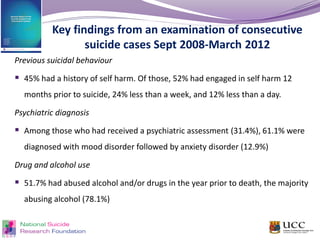
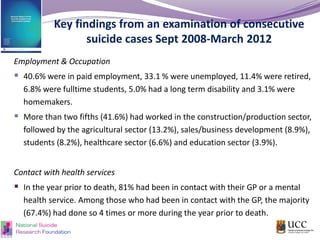
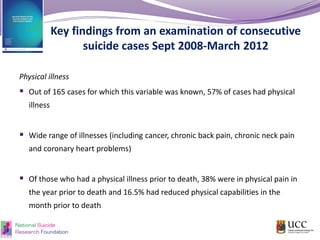
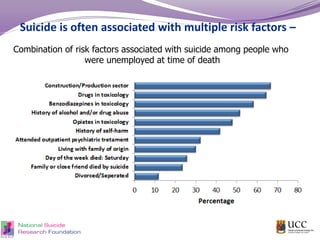
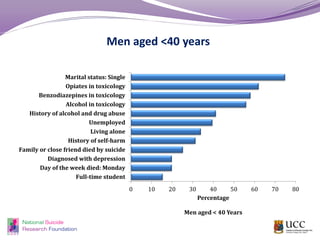
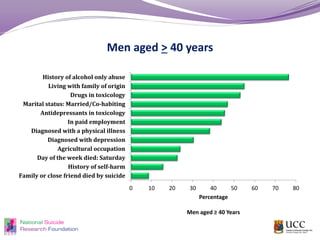
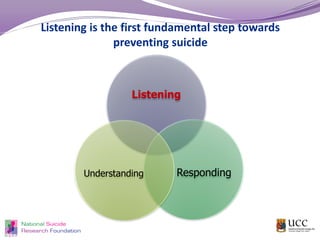
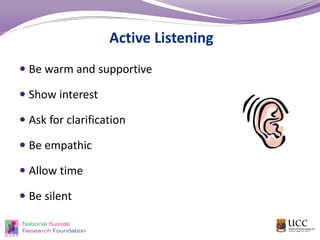
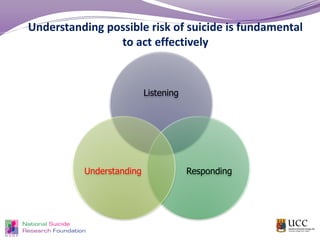
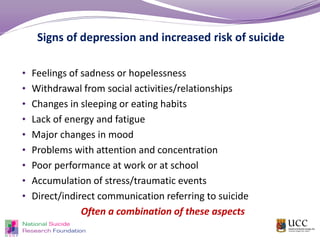
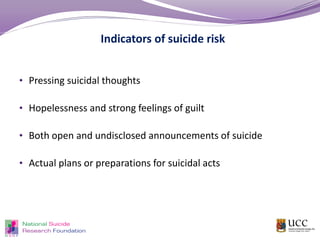
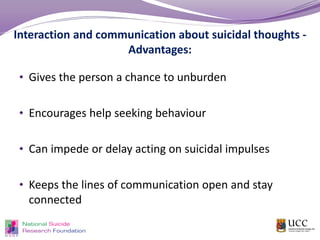
The document discusses the trends, risk factors, and prevention strategies related to suicide in Ireland, presenting data on the prevalence of suicide and self-harm, along with insights into the characteristics of individuals affected. Key findings reveal that many individuals who died by suicide had a history of self-harm or mental health issues and emphasizes the importance of listening and engaging with those at risk. The document also outlines the objectives of the Suicide Support and Information System (SSIS) aimed at improving support for bereaved individuals and understanding the patterns and causes of suicide.