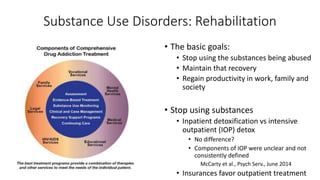
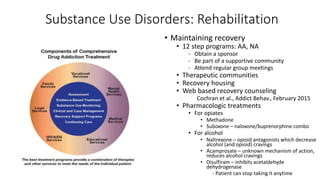
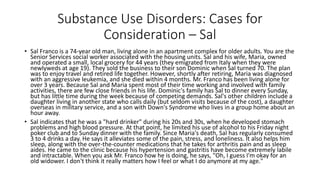
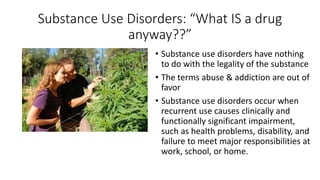
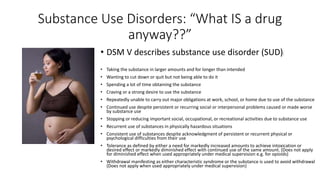
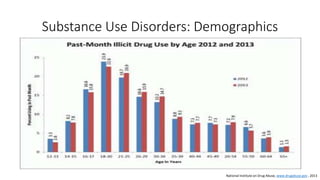
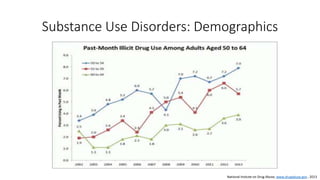
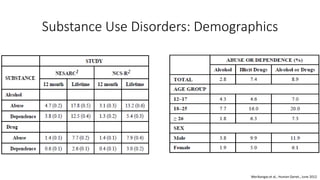
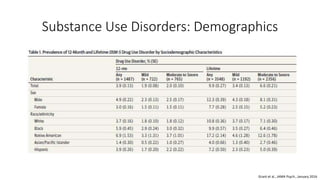
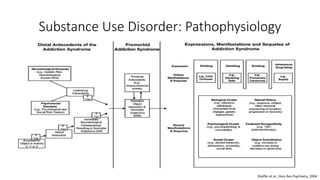
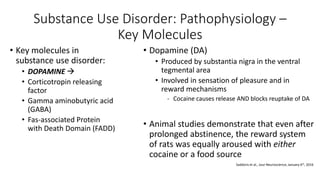
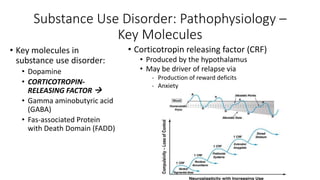
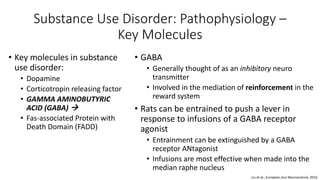
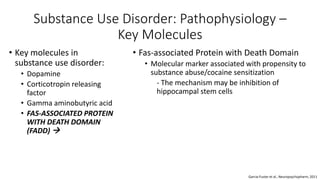
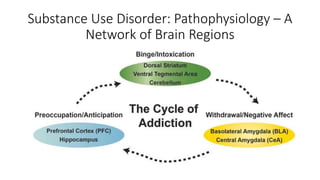
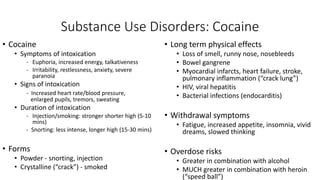
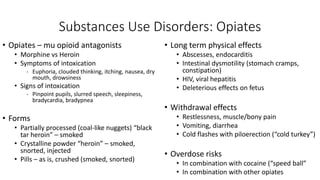
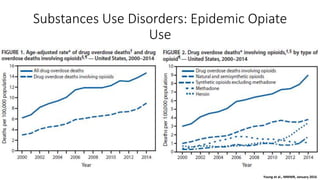
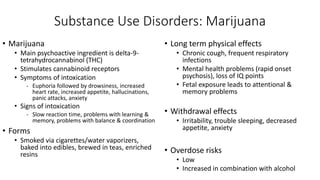
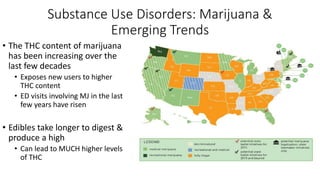
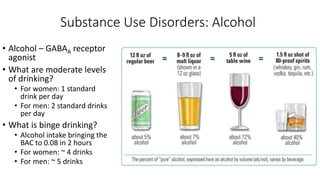
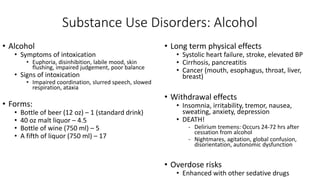
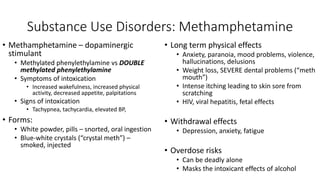
This document discusses substance use disorders and provides several case examples. It begins with definitions of key terms like abuse versus addiction. It then reviews demographics of those with substance use disorders and the pathophysiology of addiction, focusing on key molecules like dopamine, corticotropin, GABA, and FADD. Specific substances like cocaine, opiates, marijuana, alcohol, and methamphetamine are examined in depth. The document concludes with a discussion of substance use rehabilitation and approaches to diagnosis, including asking questions and urine drug screening.

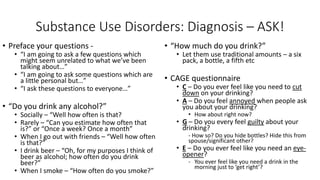
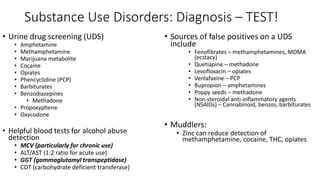
![Substance Use Disorders: Diagnosis – ASK!
• Do you use any illegal drugs?
• Don’t say illicit drugs
• Don’t say street drugs
• “Yes.”
• What drug do you use?
• Then - “Do you use any other drugs?”
• Then – Specify some choices…
• “No.”
• Have you ever used an illegal substance in
the past? Which one? Any others?
• When was the last time you used an illegal
drug? How/why did you stop?
• Ask specifically about marijuana!
• For each substance identified, ask how
often and how much is consumed
• “How much money do you spend a week on
[X]?”
• “Can you estimate it for me?”
- Then in your mind, increase that amount by at
least 50%!
• “Have you ever overused prescription
drugs?
• Has a doctor ever stopped prescribing a drug
to you when you weren’t ready to stop??](https://image.slidesharecdn.com/cb5576c1-970c-4fcb-8381-25825aade295-160419015510/85/Substance-Use-Disorders-29-320.jpg)