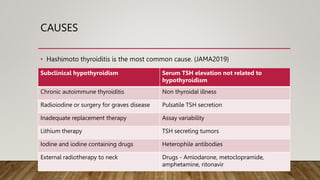
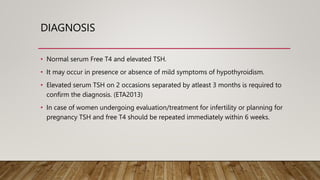
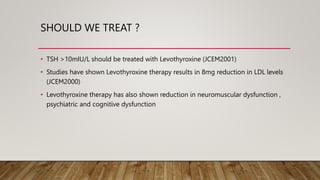
Subclinical hypothyroidism is defined as normal serum free T4 levels with an elevated serum TSH. It has a prevalence of 3-15% in the adult population in India, and is more common in women, the elderly, and iodine-sufficient areas. Hashimoto's thyroiditis is the most common cause. A diagnosis requires two elevated TSH levels at least 3 months apart. Treatment with levothyroxine is recommended for TSH levels over 10 mIU/L and may help reduce risks of overt hypothyroidism, heart disease, stroke, infertility and other issues. Treatment goals are a TSH below 3 mIU/L.