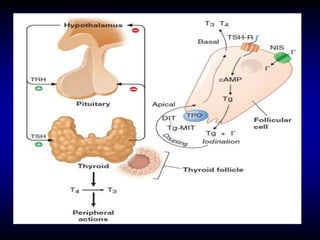
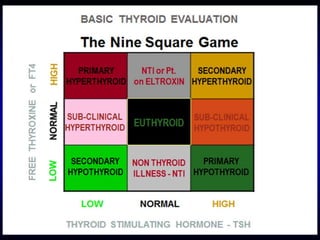
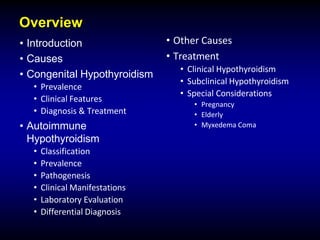
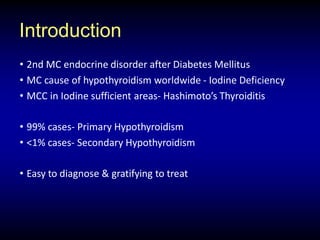
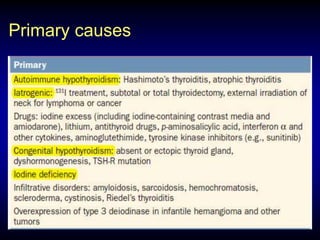
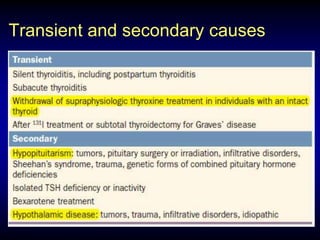
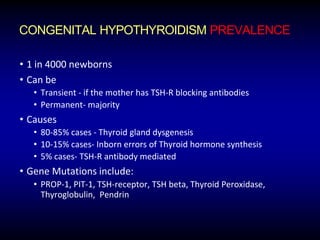
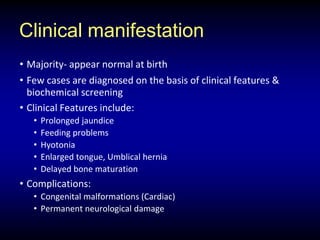
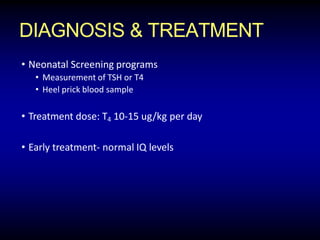
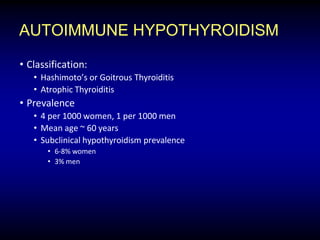
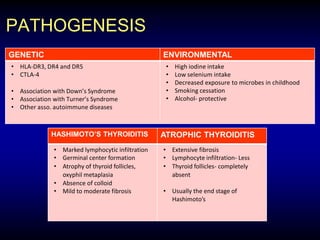
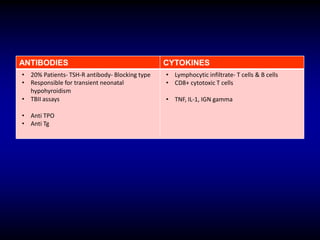
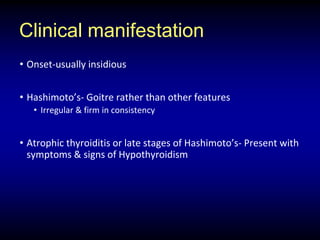
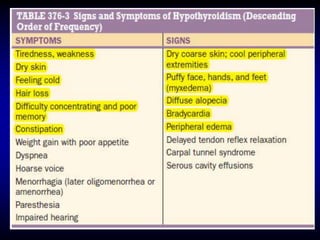
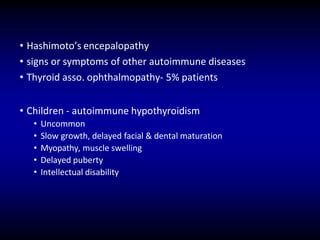
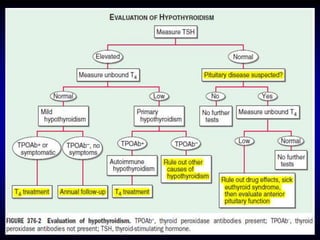
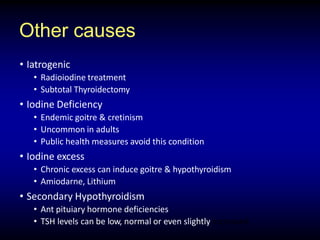
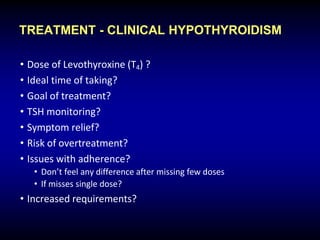
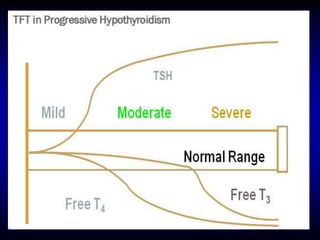
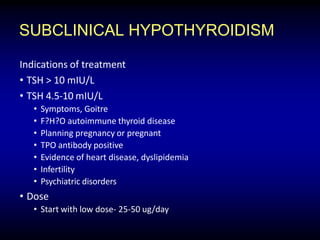
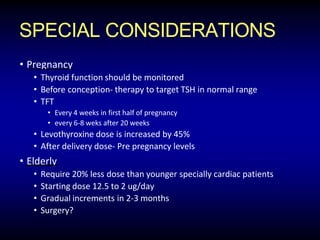
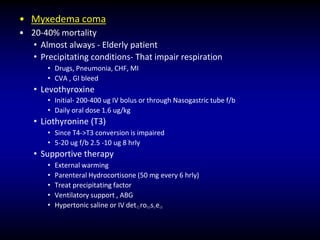
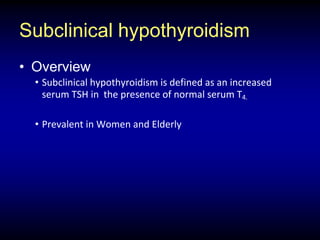
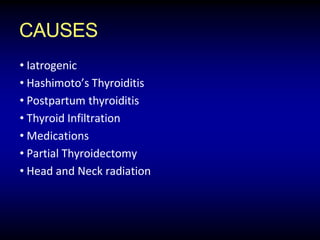
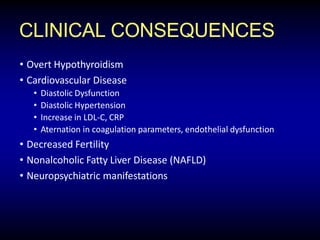
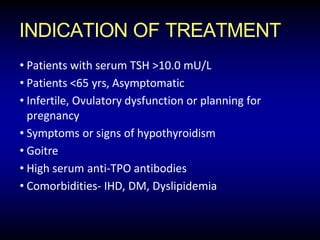
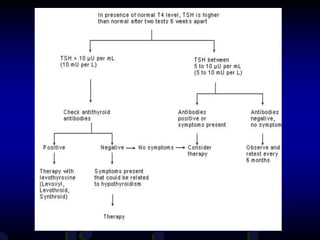
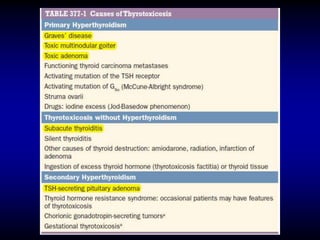
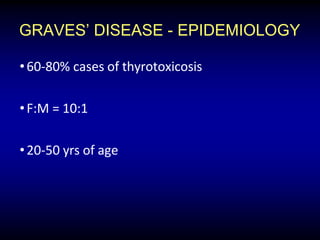
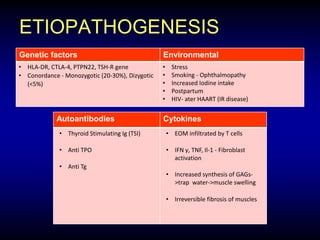
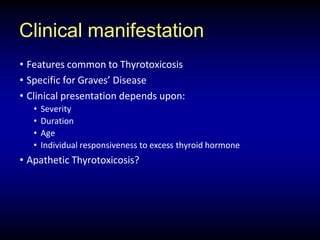
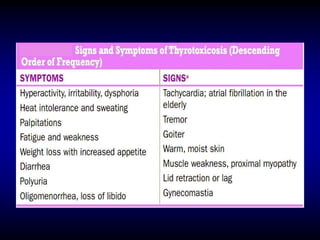
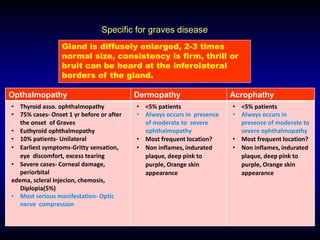
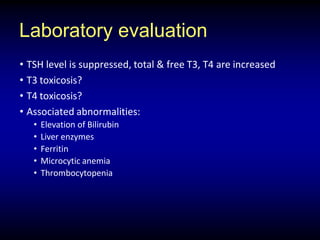
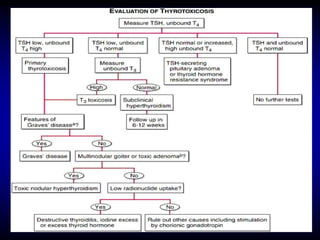
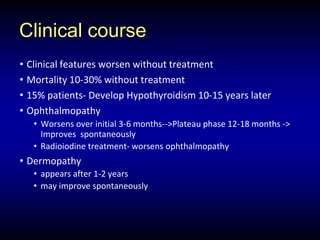
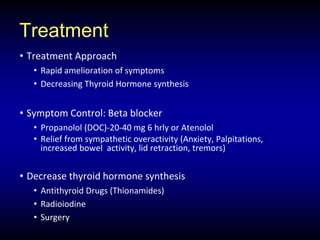
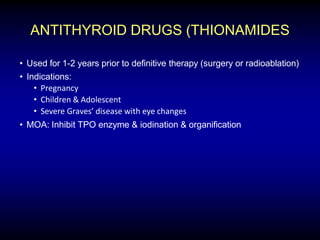
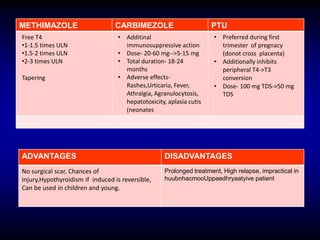
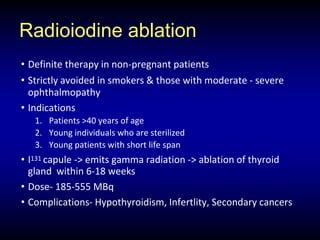
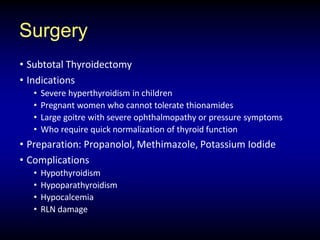
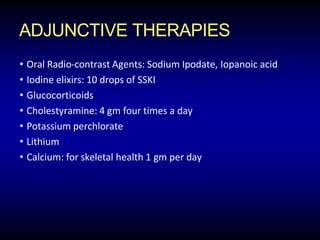
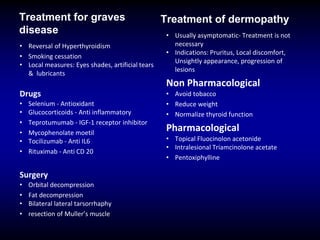
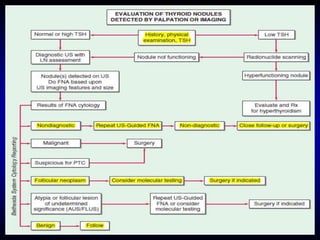
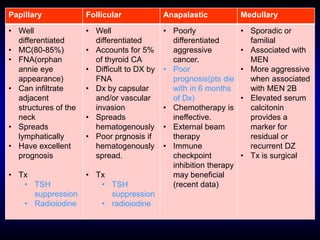
This document provides an overview of thyroid function and diseases of the thyroid gland. It discusses the assessment of thyroid function including common tests. It then covers the topics of hypothyroidism and hyperthyroidism in detail. For hypothyroidism, it describes the causes, presentations, diagnoses and treatment approaches for congenital hypothyroidism, autoimmune hypothyroidism, subclinical hypothyroidism and special considerations in pregnancy and the elderly. For hyperthyroidism, it focuses on Graves' disease, outlining its epidemiology, pathogenesis, clinical manifestations, diagnostic evaluation, clinical course and treatment options including antithyroid medications and radioiodine.