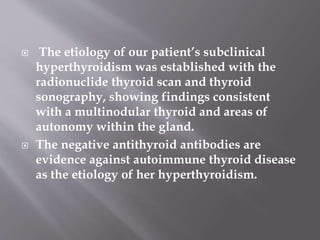
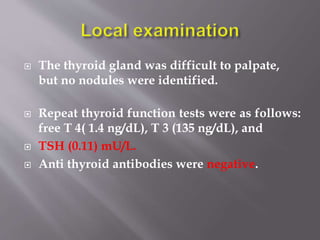
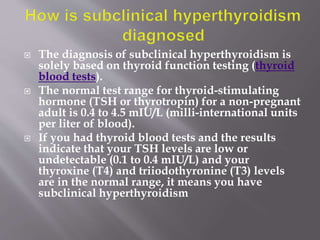
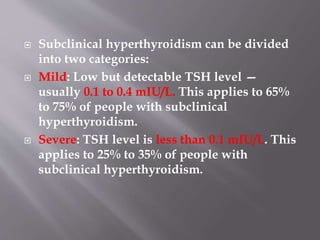
1. The patient is a 48-year-old woman found to have subclinical hyperthyroidism on routine screening, with a TSH of 0.17 mU/L and no symptoms of hyperthyroidism.
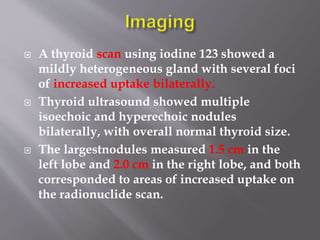
2. Thyroid ultrasound showed multiple isoechoic and hyperechoic nodules bilaterally, with the largest measuring 1.5 cm and 2.0 cm.
3. Given her stable thyroid function, lack of symptoms, and normal bone density, the decision was made not to treat and monitor her thyroid levels every 6 months.

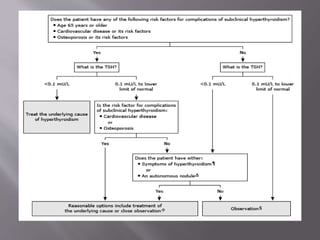
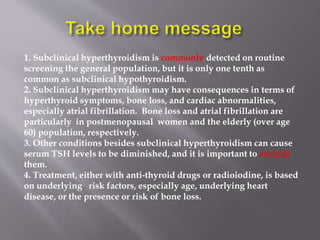
![ The principal issues surrounding the clinical
management of subclinical hyper- thyroidism are :
[1] possible symptoms of mild hyperthyroidism
(2)bone loss, especially in postmenopausal women.
(3) possible cardiovascular disease, especially atrial
fibrillation.
Indications of treatment:-](https://image.slidesharecdn.com/casepresentation3-240415224734-e0296a81/85/case-presentationof-the-endocrine-3-pptx-20-320.jpg)