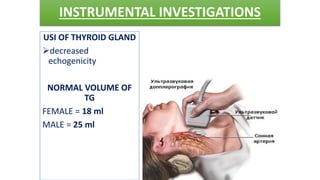
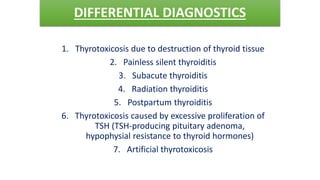
Hypothyroidism and diffuse toxic goiter (Graves' disease) are conditions caused by thyroid hormone imbalances. Hypothyroidism is caused by thyroid hormone deficiency and can be primary or central in nature. Diffuse toxic goiter is an autoimmune disease characterized by thyroid hormone excess and extrathyroid symptoms. Diagnosis involves blood tests of thyroid hormones and antibodies. Treatment depends on the condition but may include thyroid hormone replacement, anti-thyroid medications, radioiodine therapy, or surgery.