This document discusses the localization of stroke based on clinical findings. It covers the basics of stroke classification and vascular territories. Key points include:
1. Stroke is classified as either ischemic (80%) due to thrombosis, embolism or hypoperfusion, or hemorrhagic (20%) due to ICH or SAH.
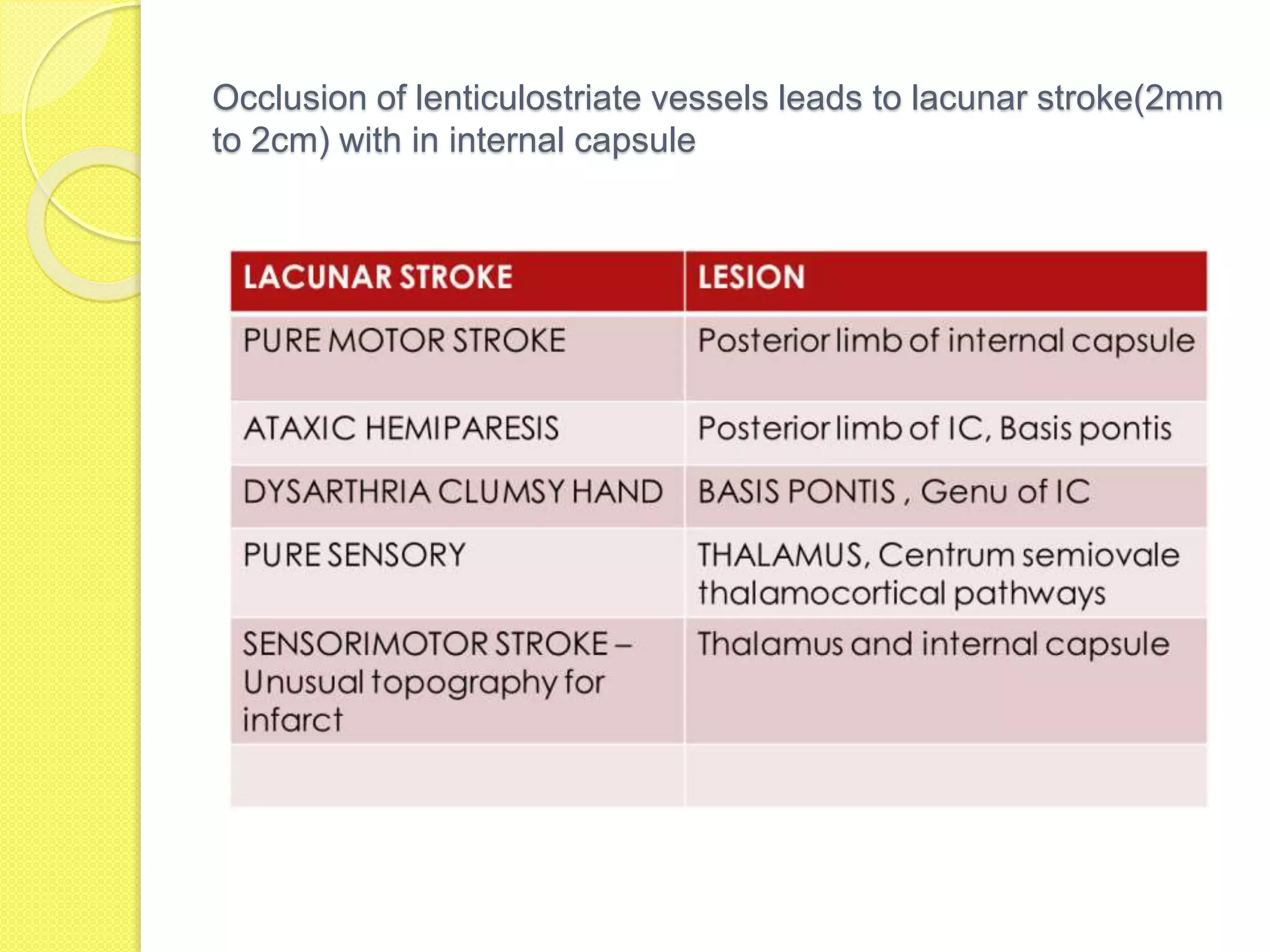
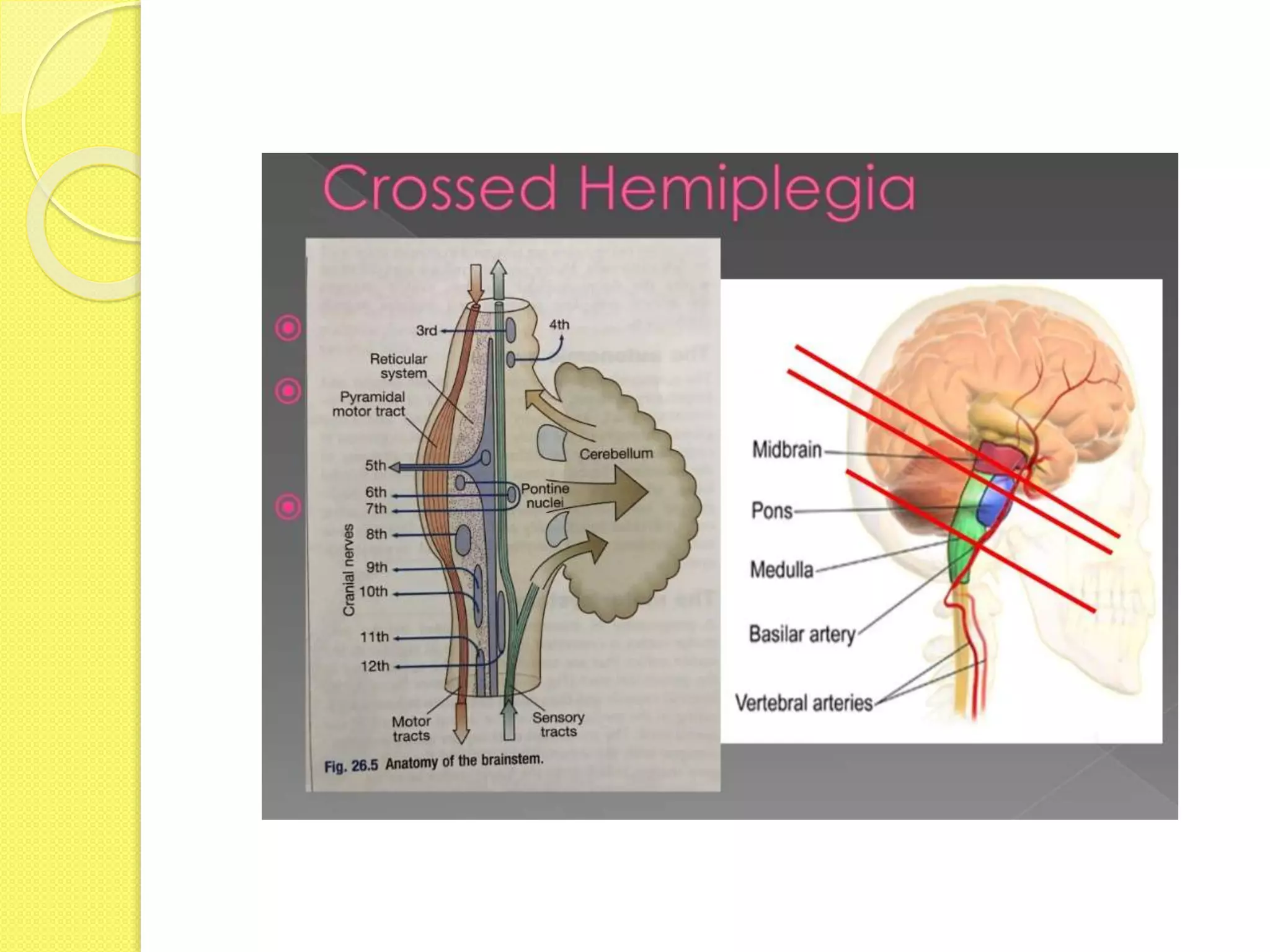
2. Localizing the site of a stroke lesion involves correlating the clinical exam with the involved vascular territory and imaging findings.
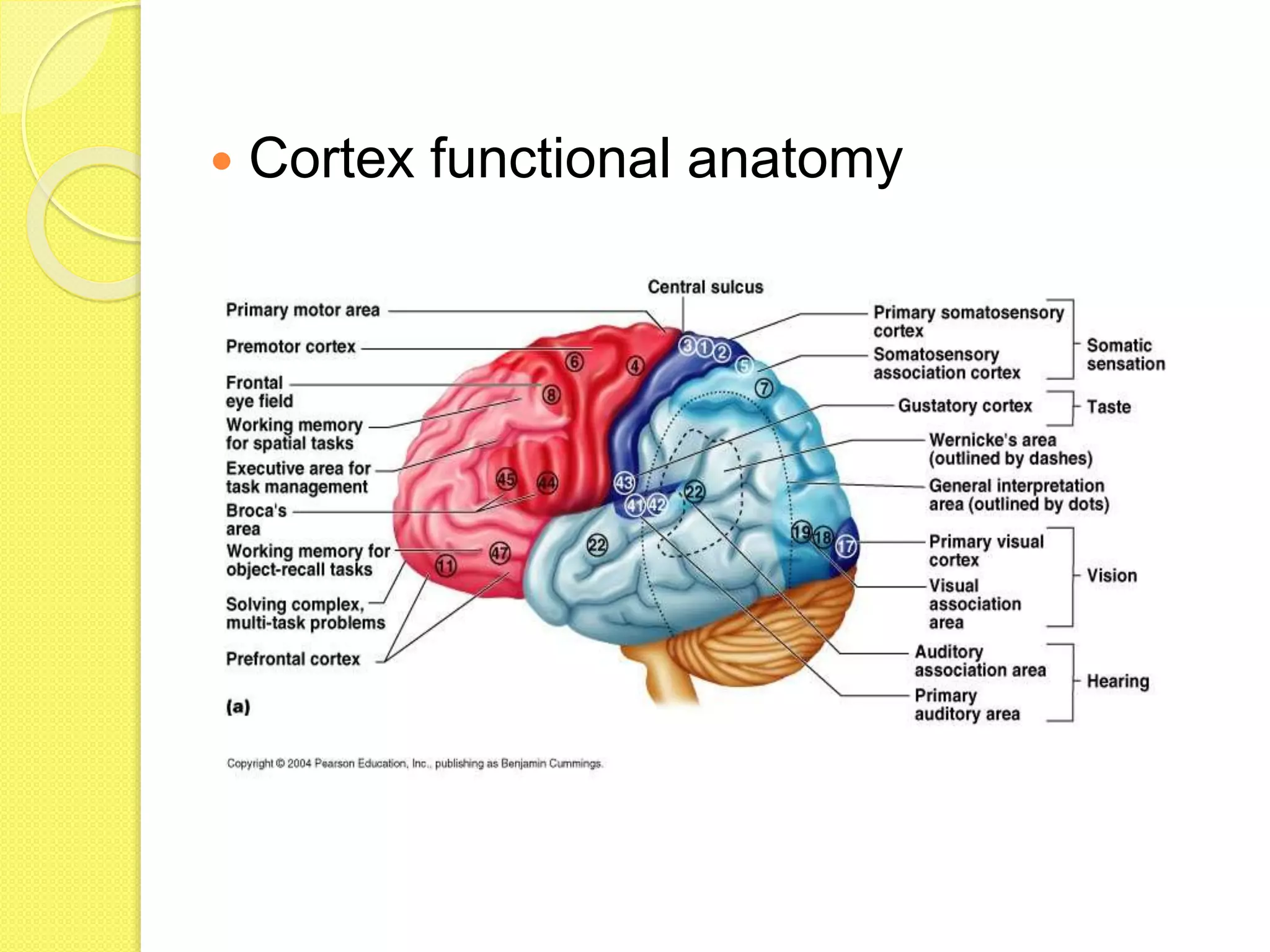
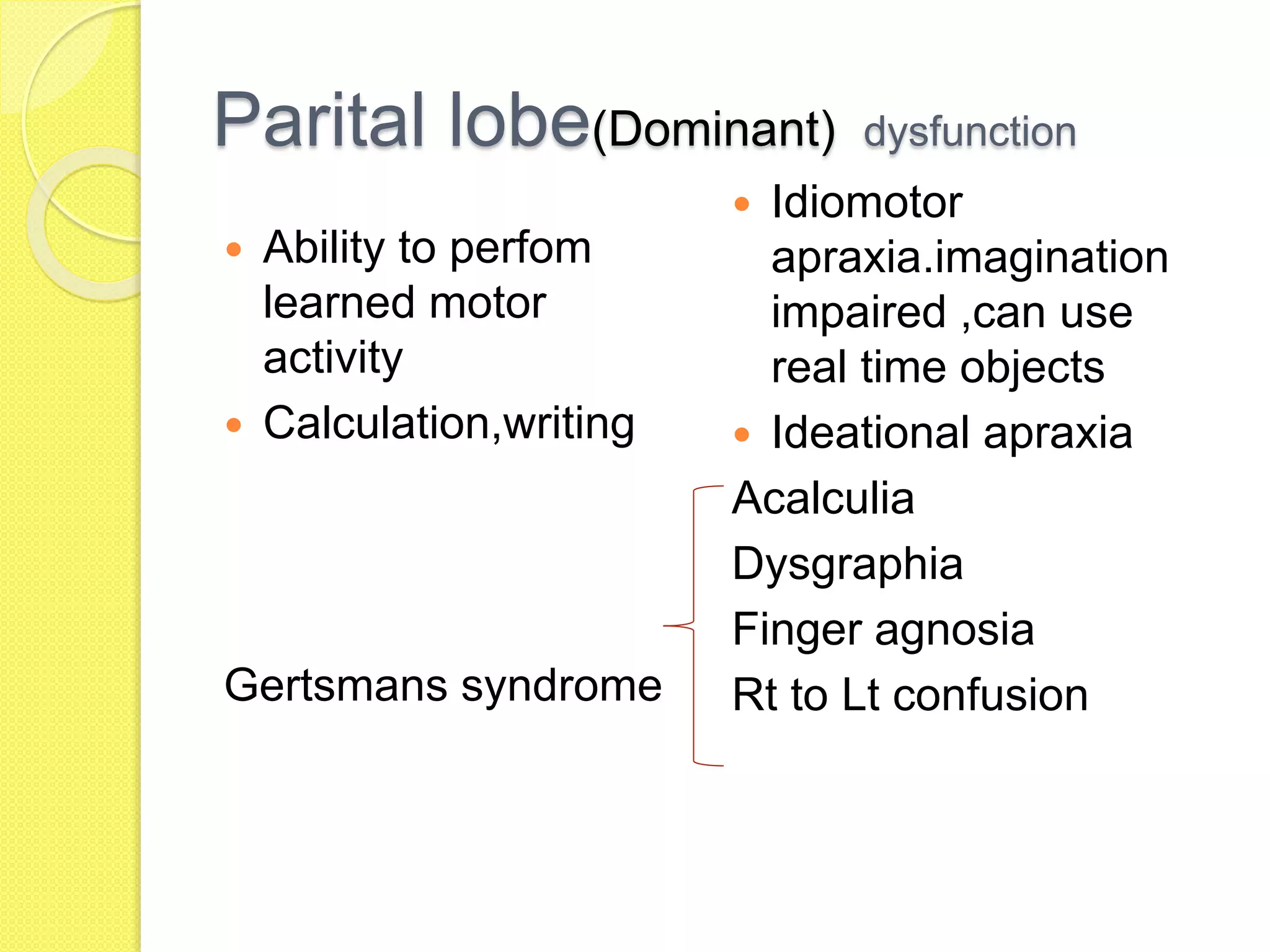
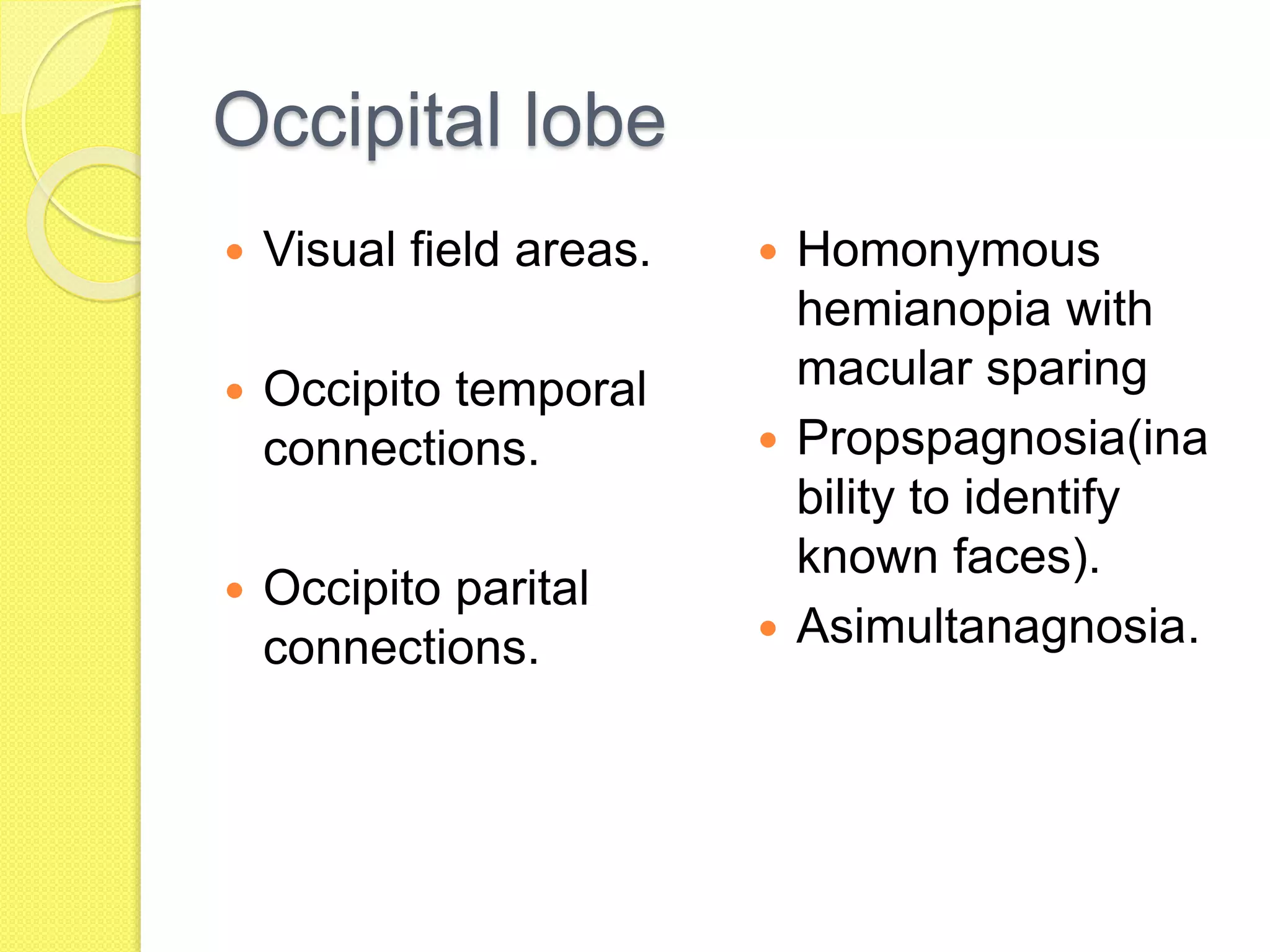
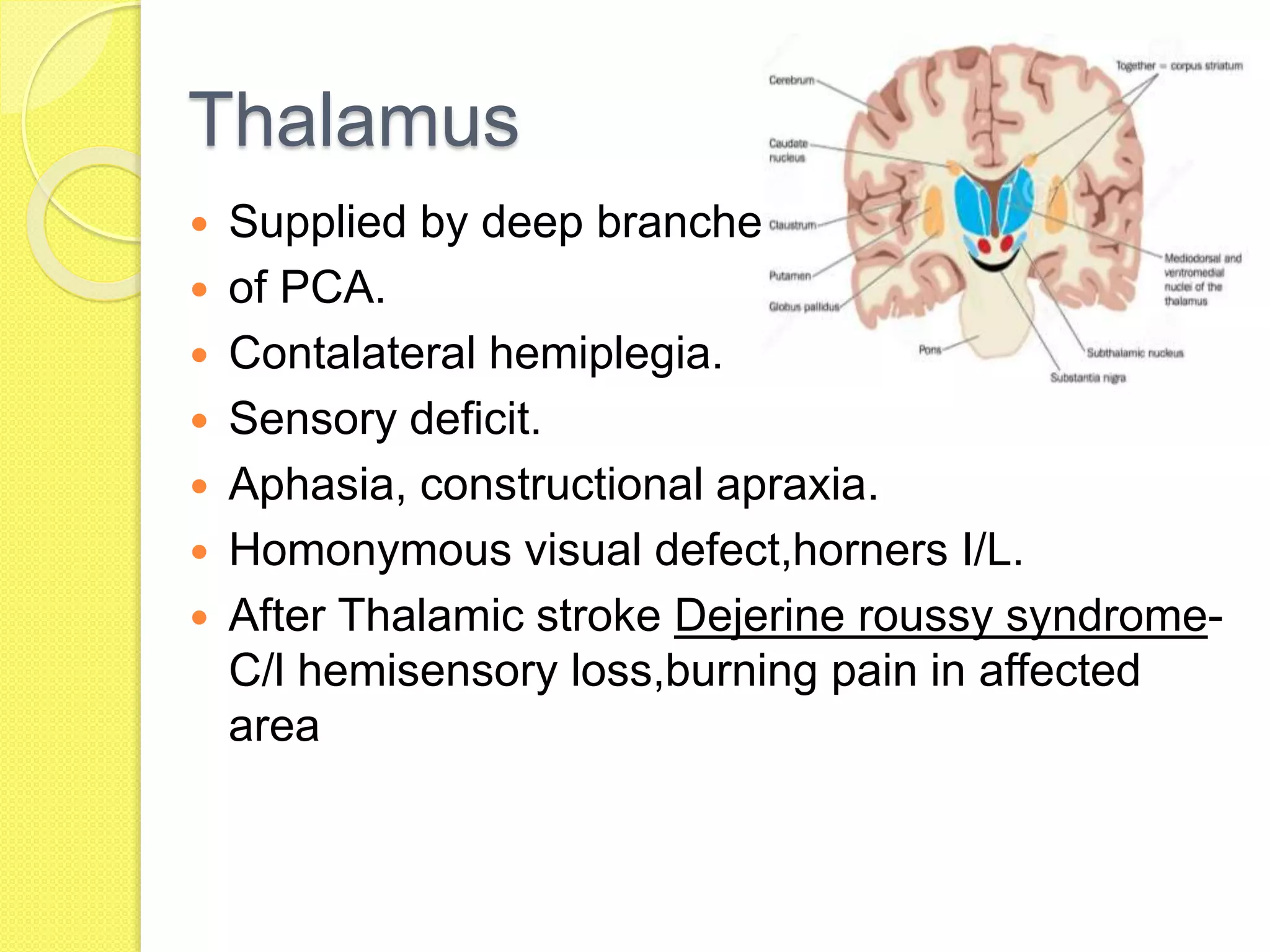
3. Symptoms vary based on the specific region affected, such as frontal lobe dysfunction presenting with behavioral changes while occipital strokes cause homonymous hemianopsia.
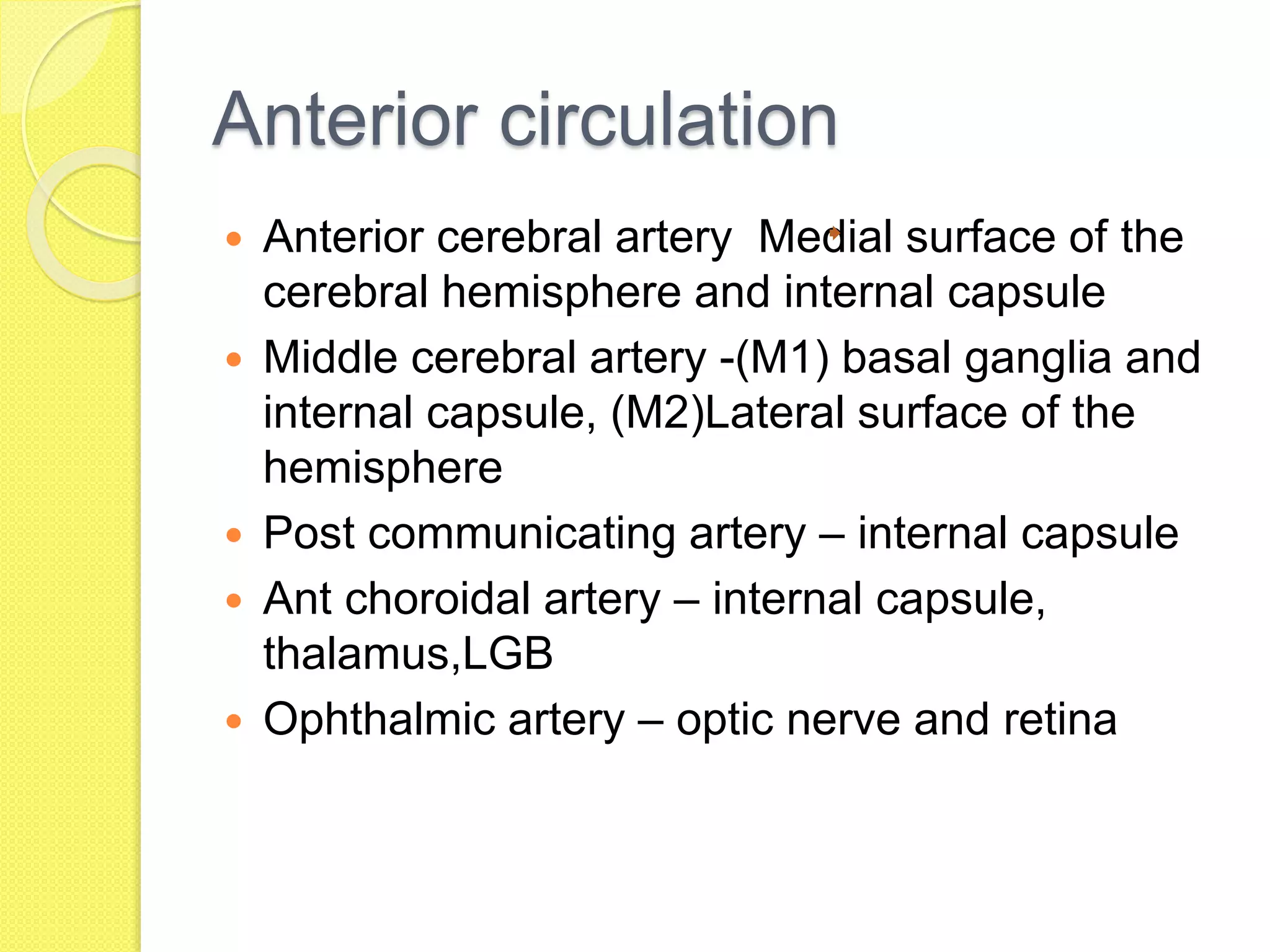
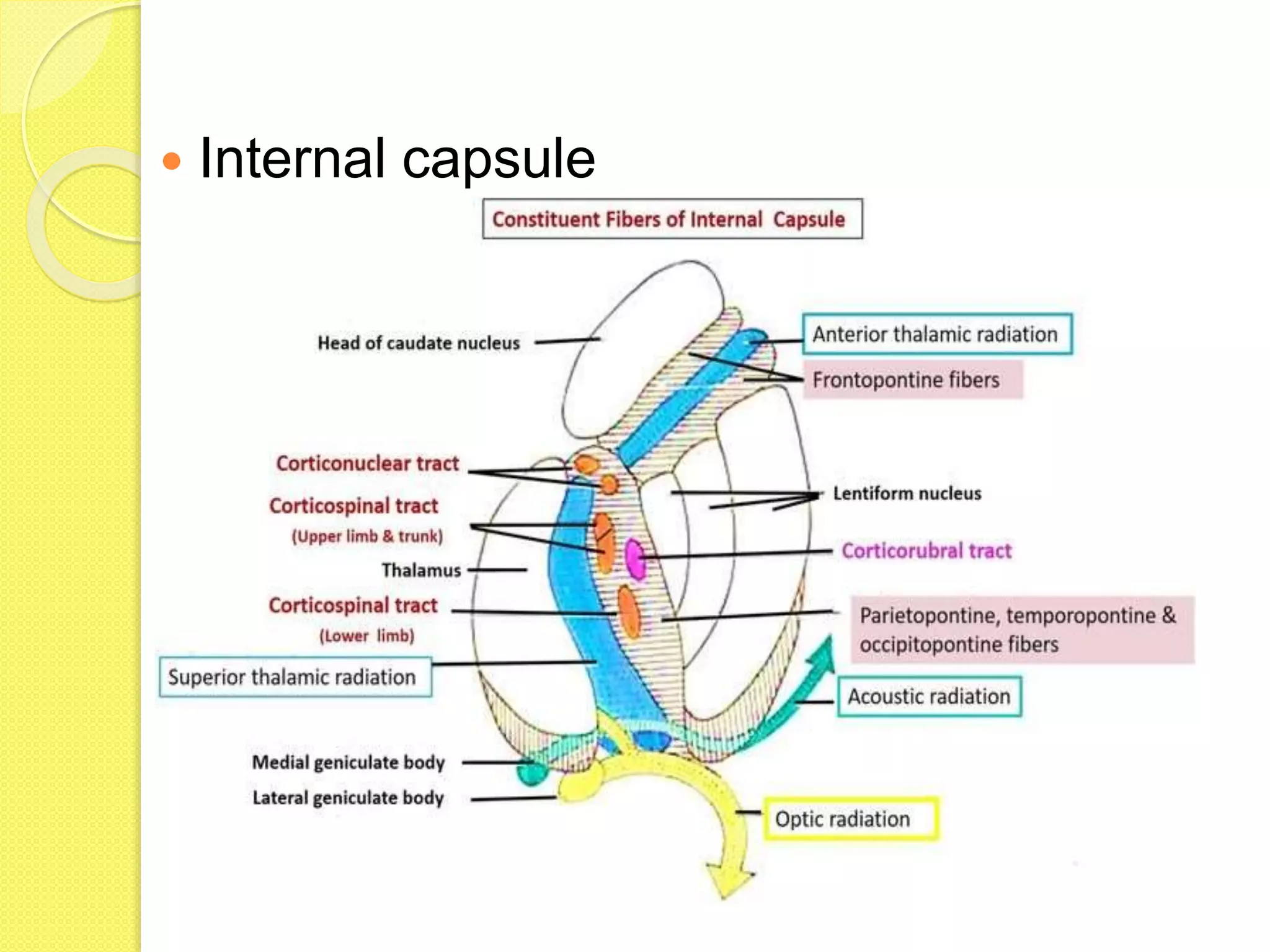
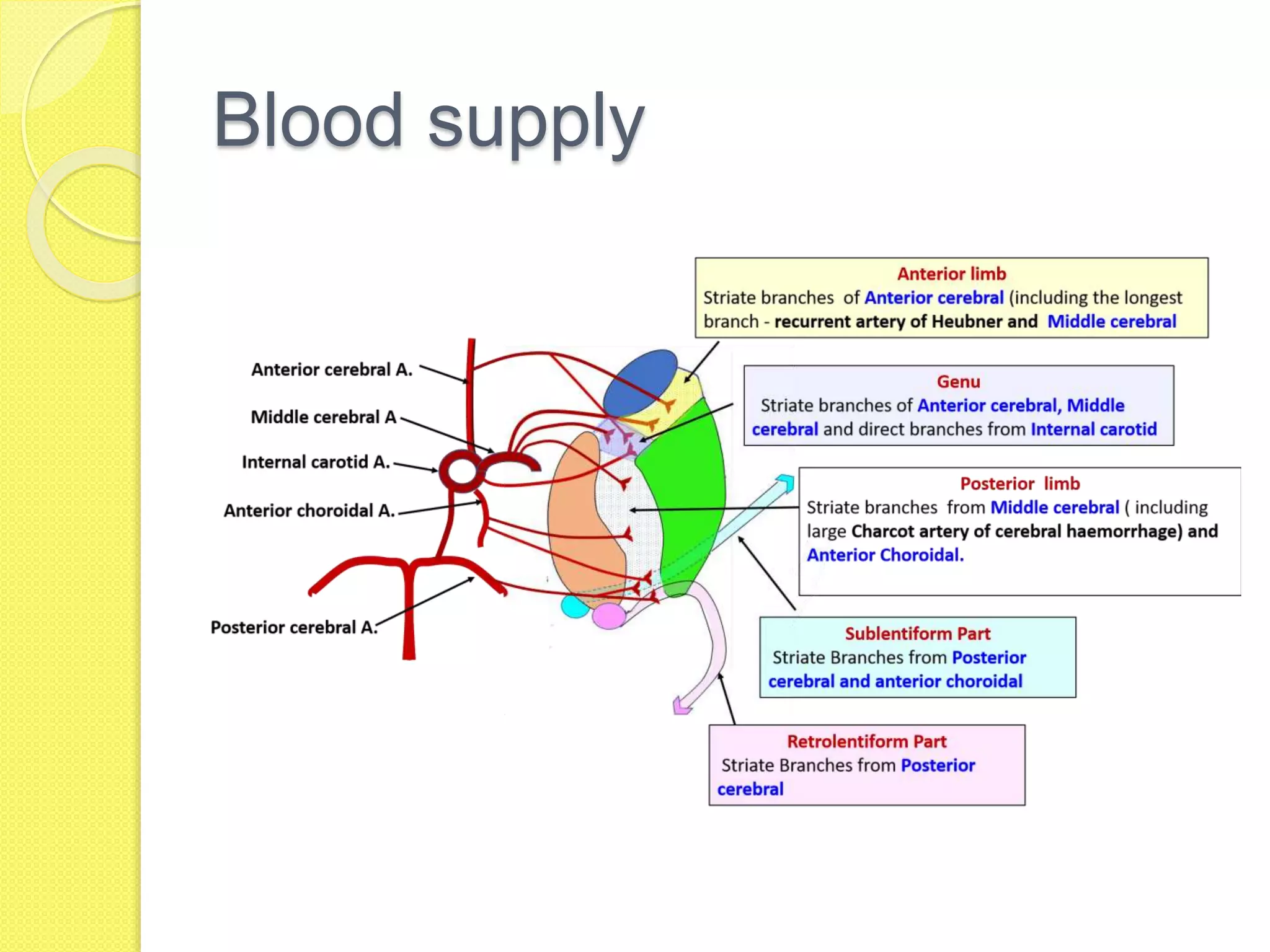
4. Different vascular territories include the anterior circulation supplied by