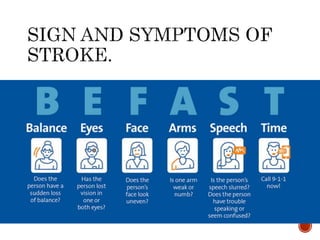
1) A woman experienced sudden onset left-sided weakness, facial asymmetry, slurred speech and drooling while at a neighbor's house. She was brought by ambulance to the emergency department.
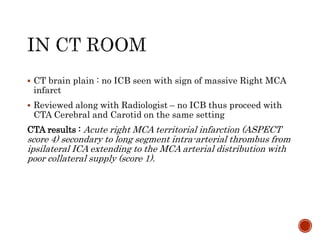
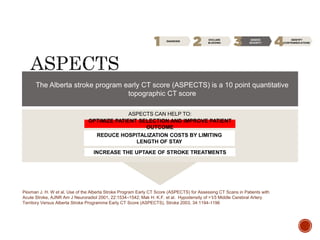
2) In the ED, her neurological examination found significant left-sided weakness. A CT scan showed a large right middle cerebral artery infarction.
3) Despite arriving within the time window, she was not eligible for thrombolysis due to the extensive area of brain injury seen on the CT scan. She was admitted for supportive care and monitoring.