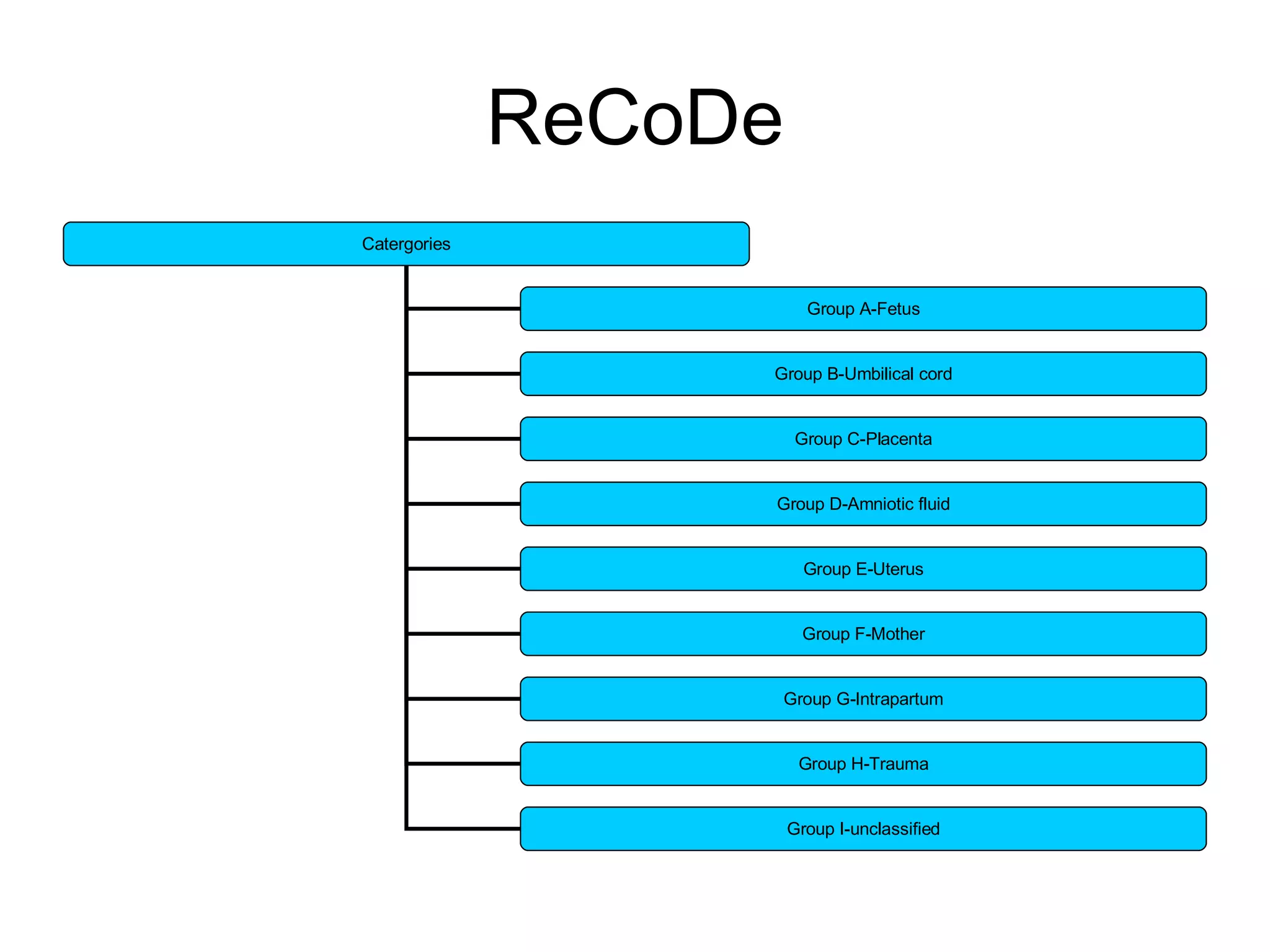
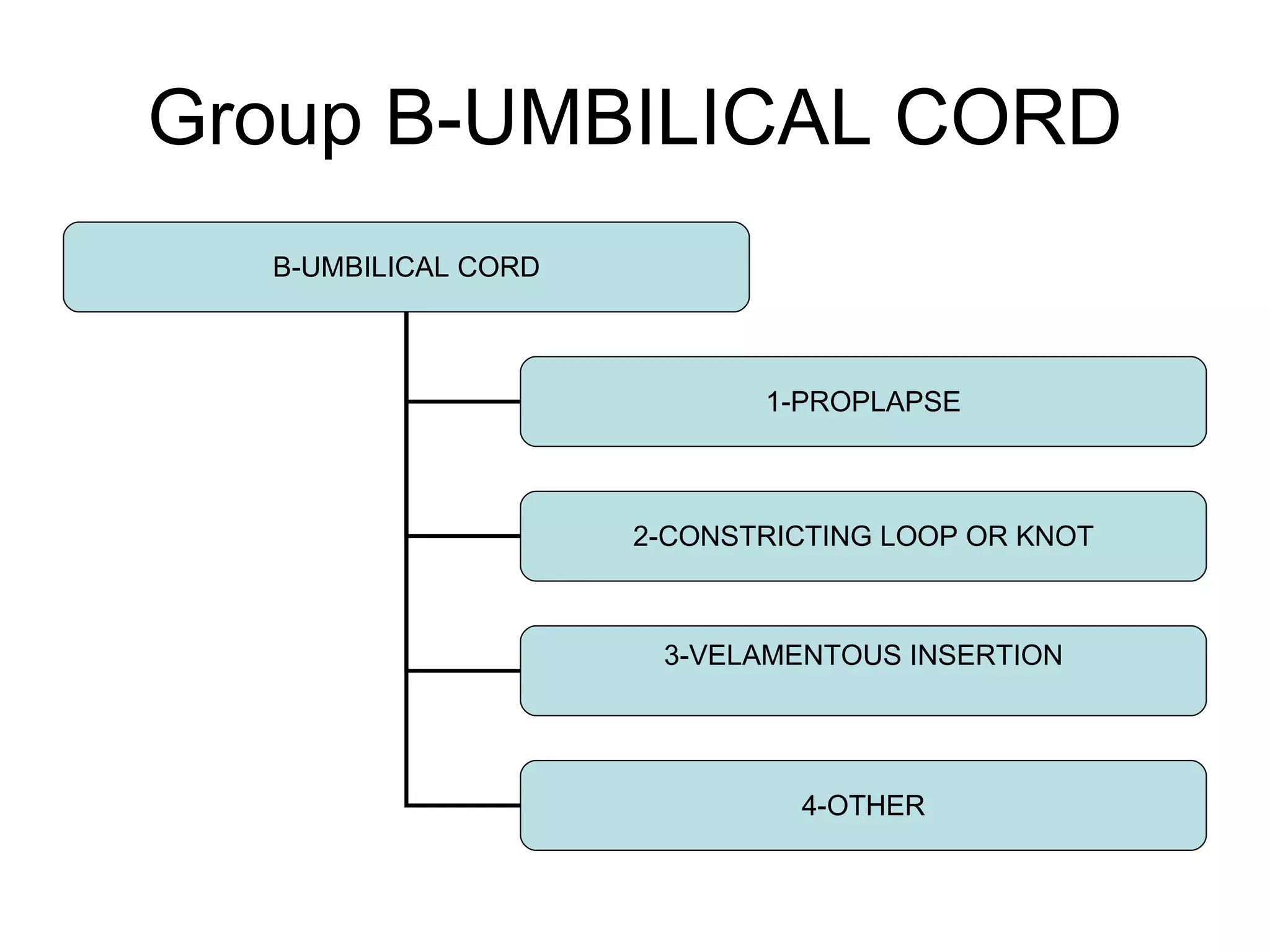
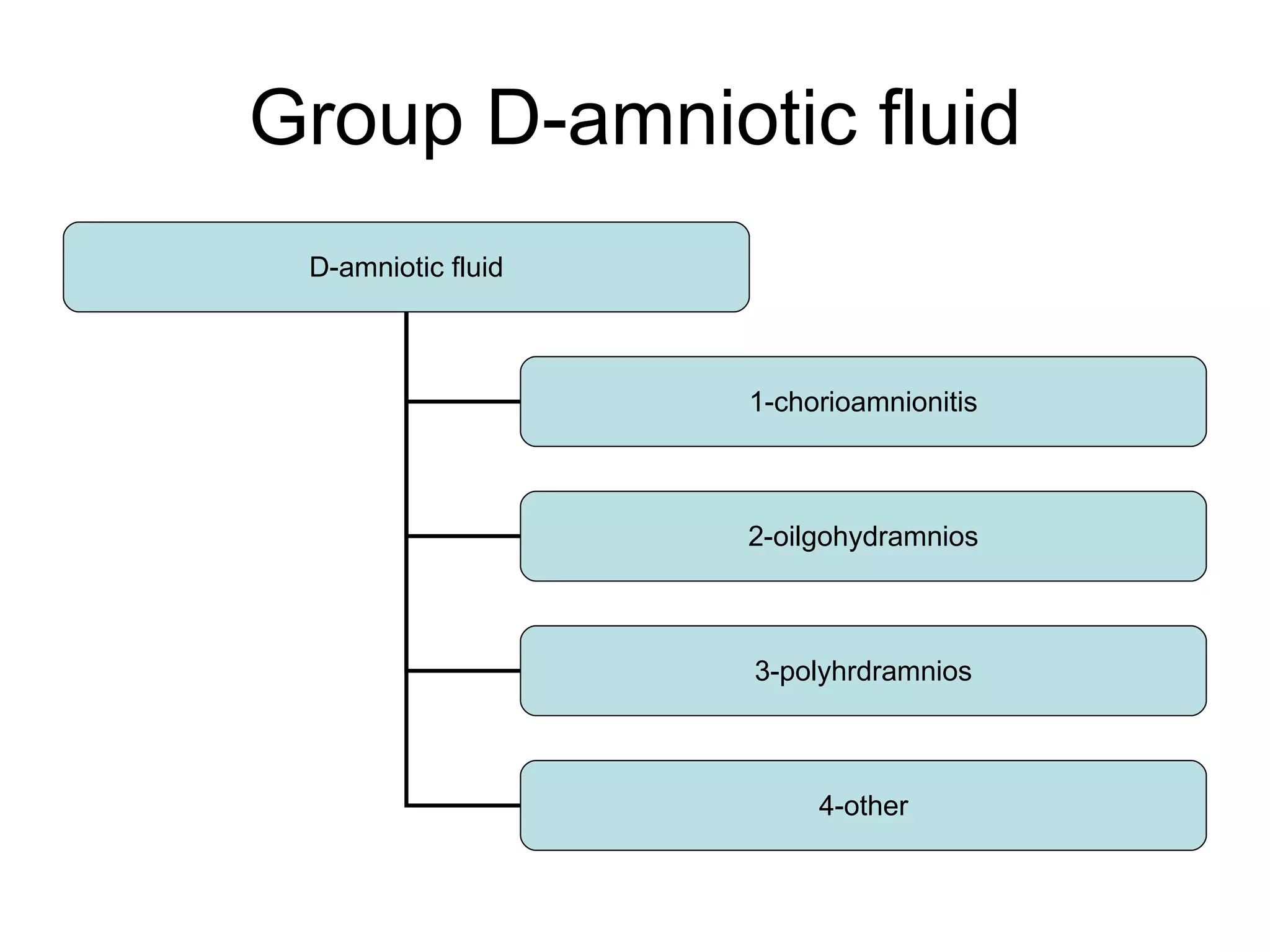
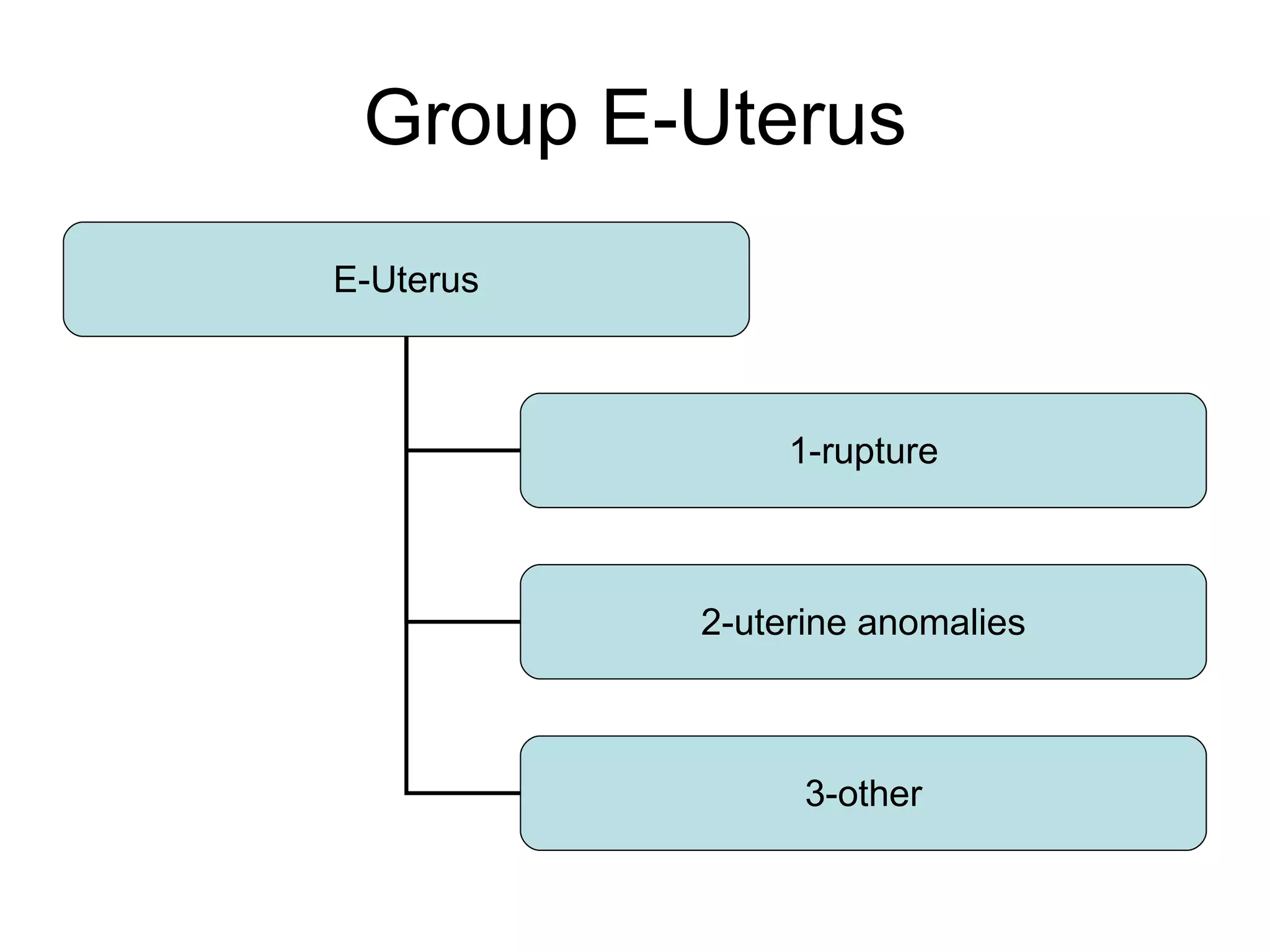
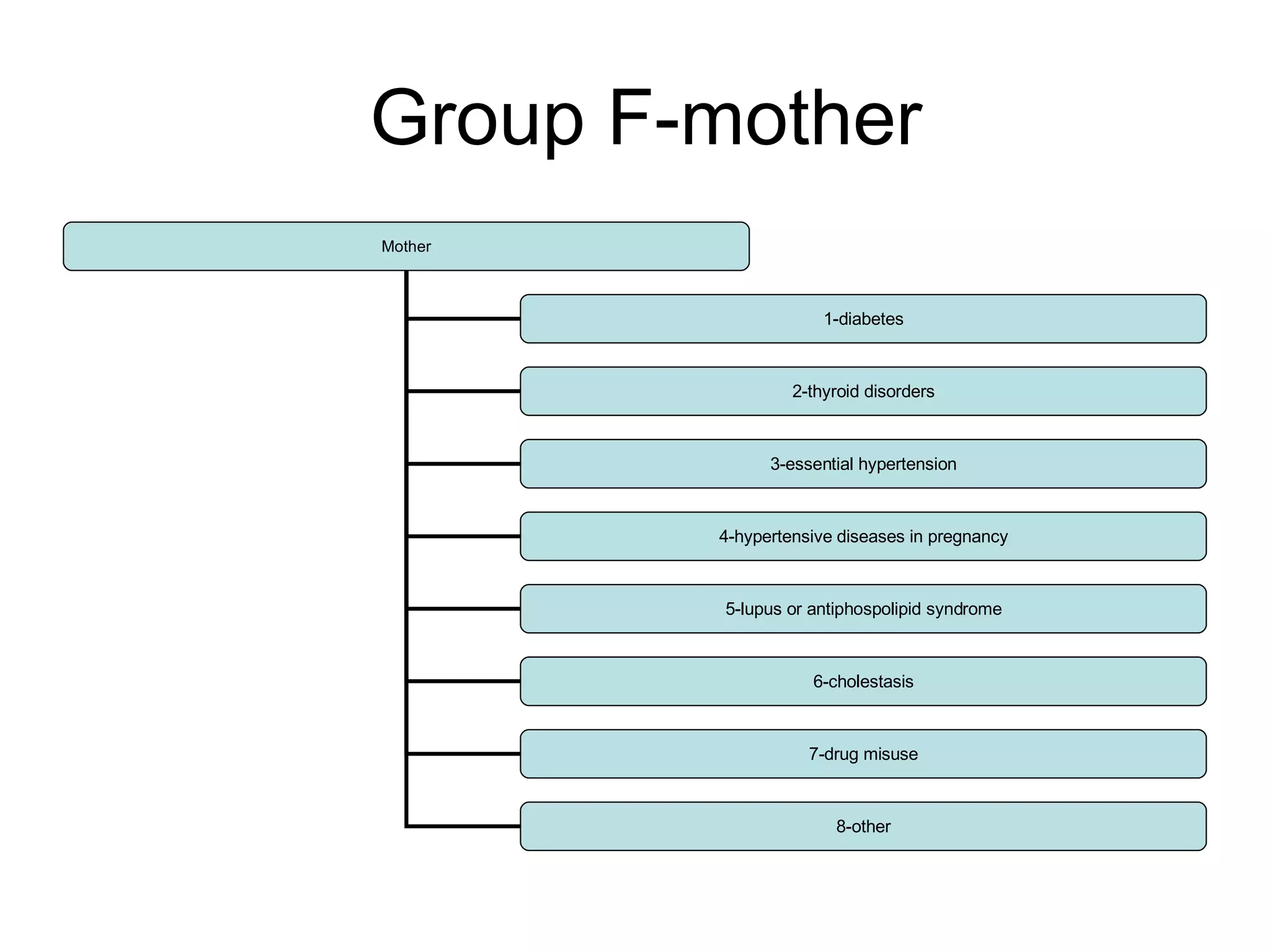
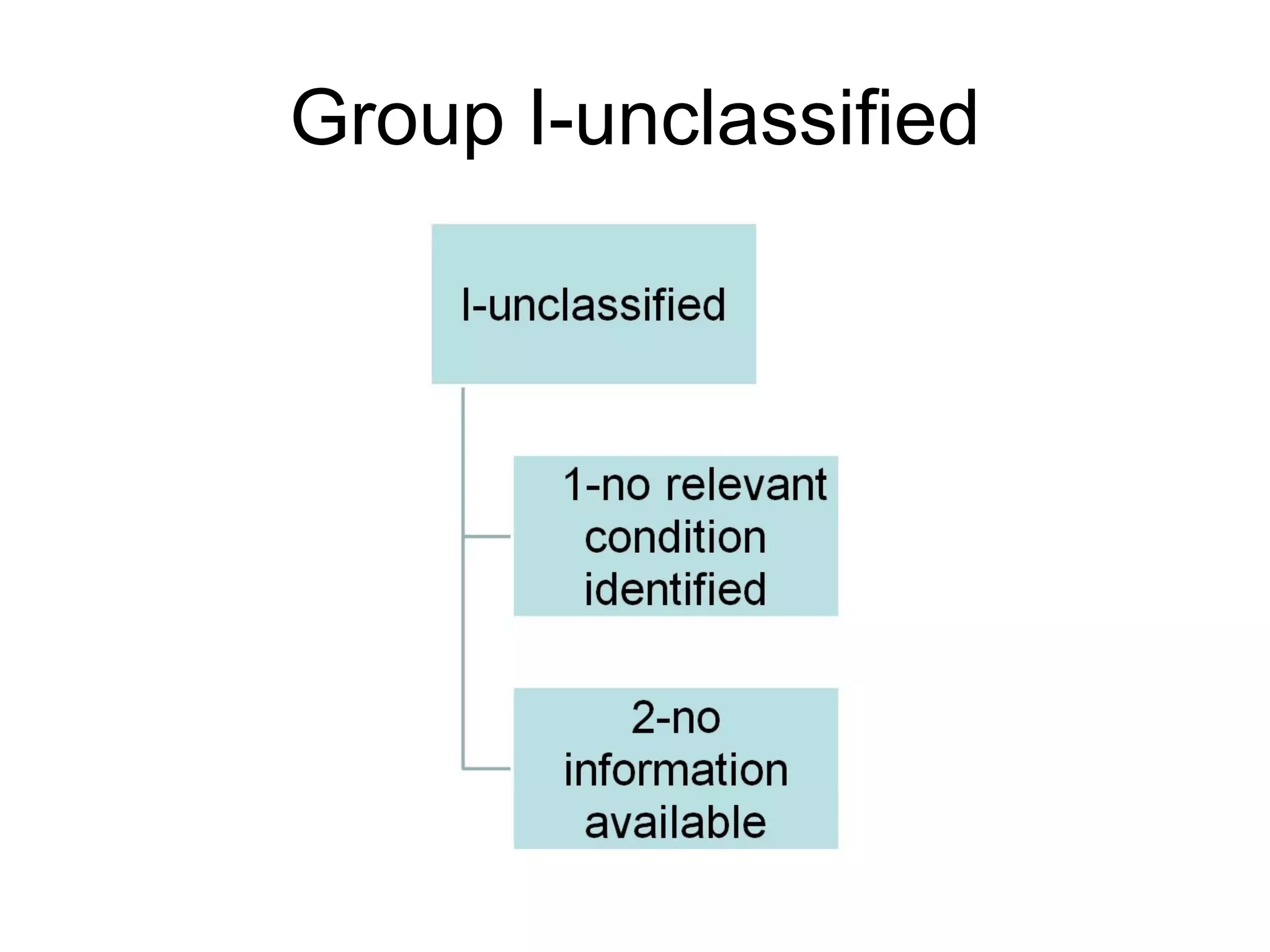
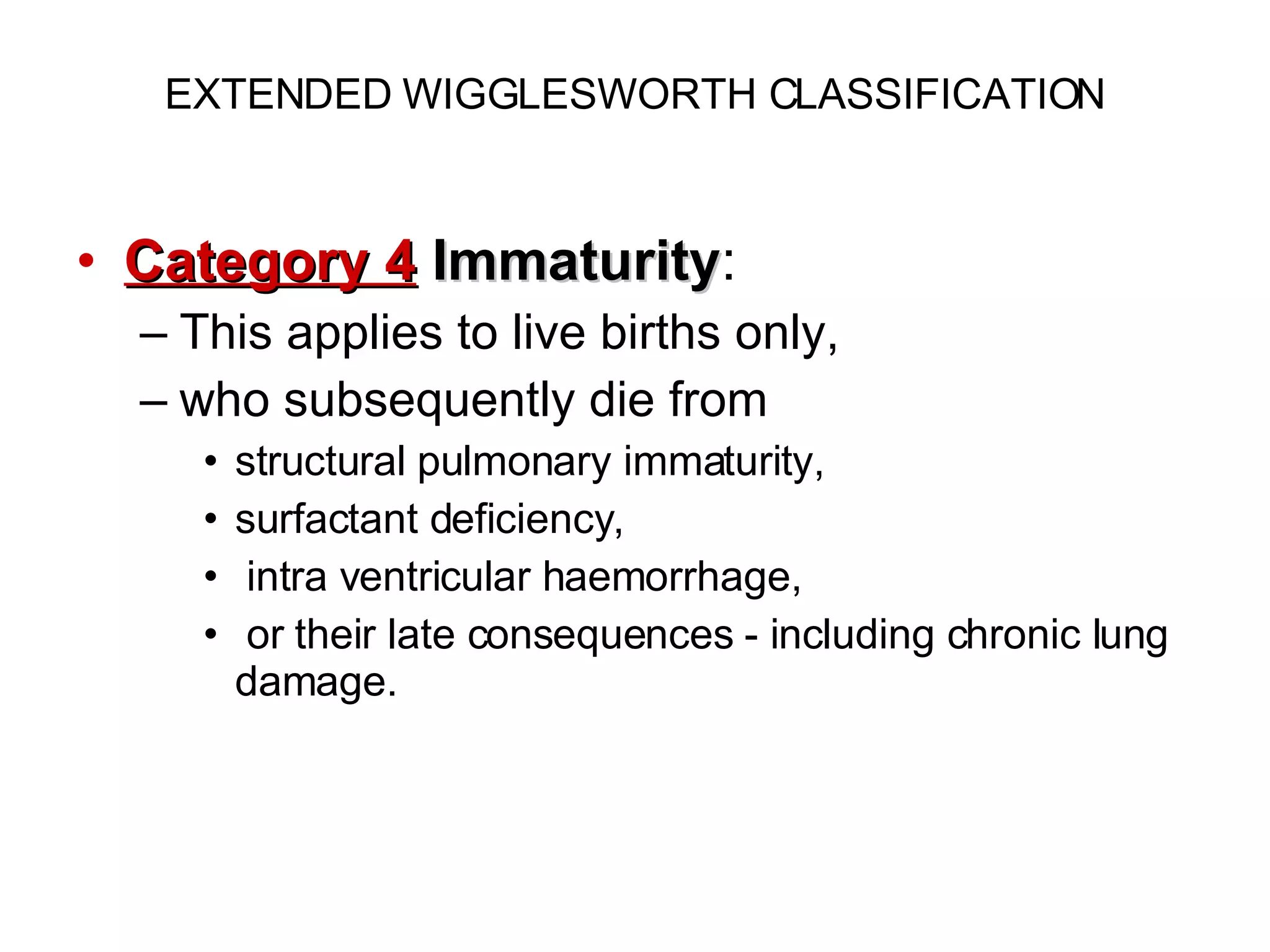
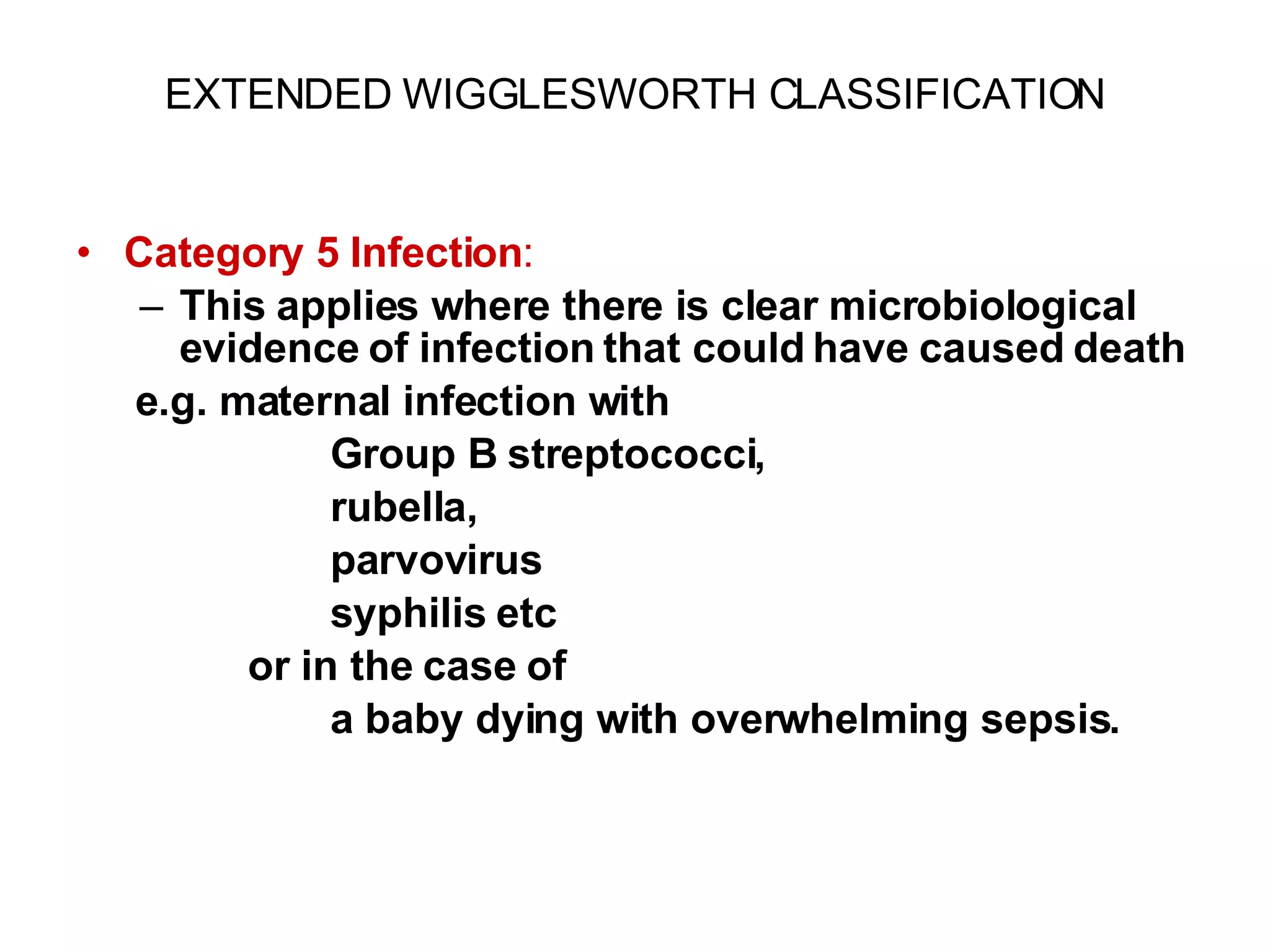
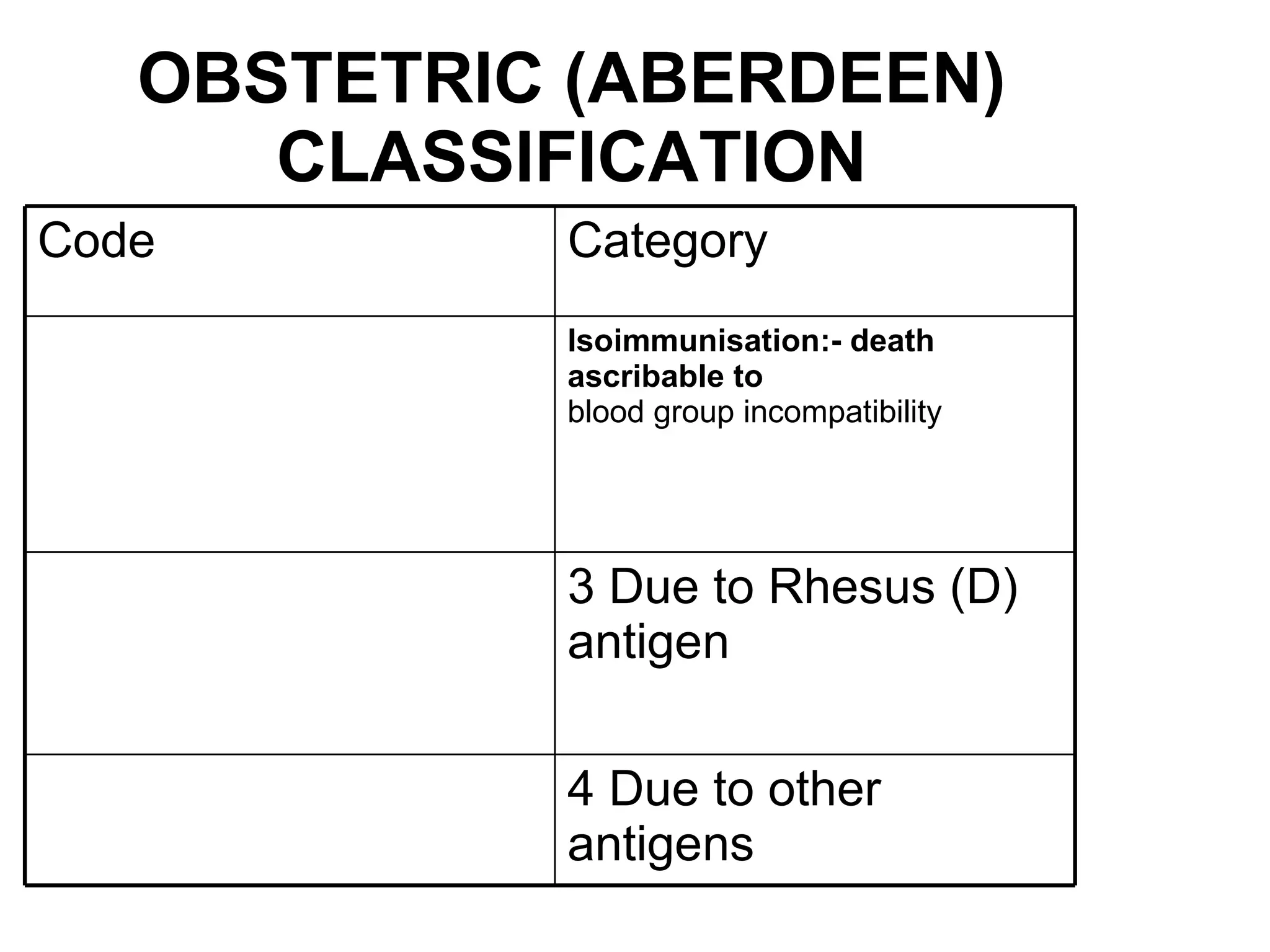
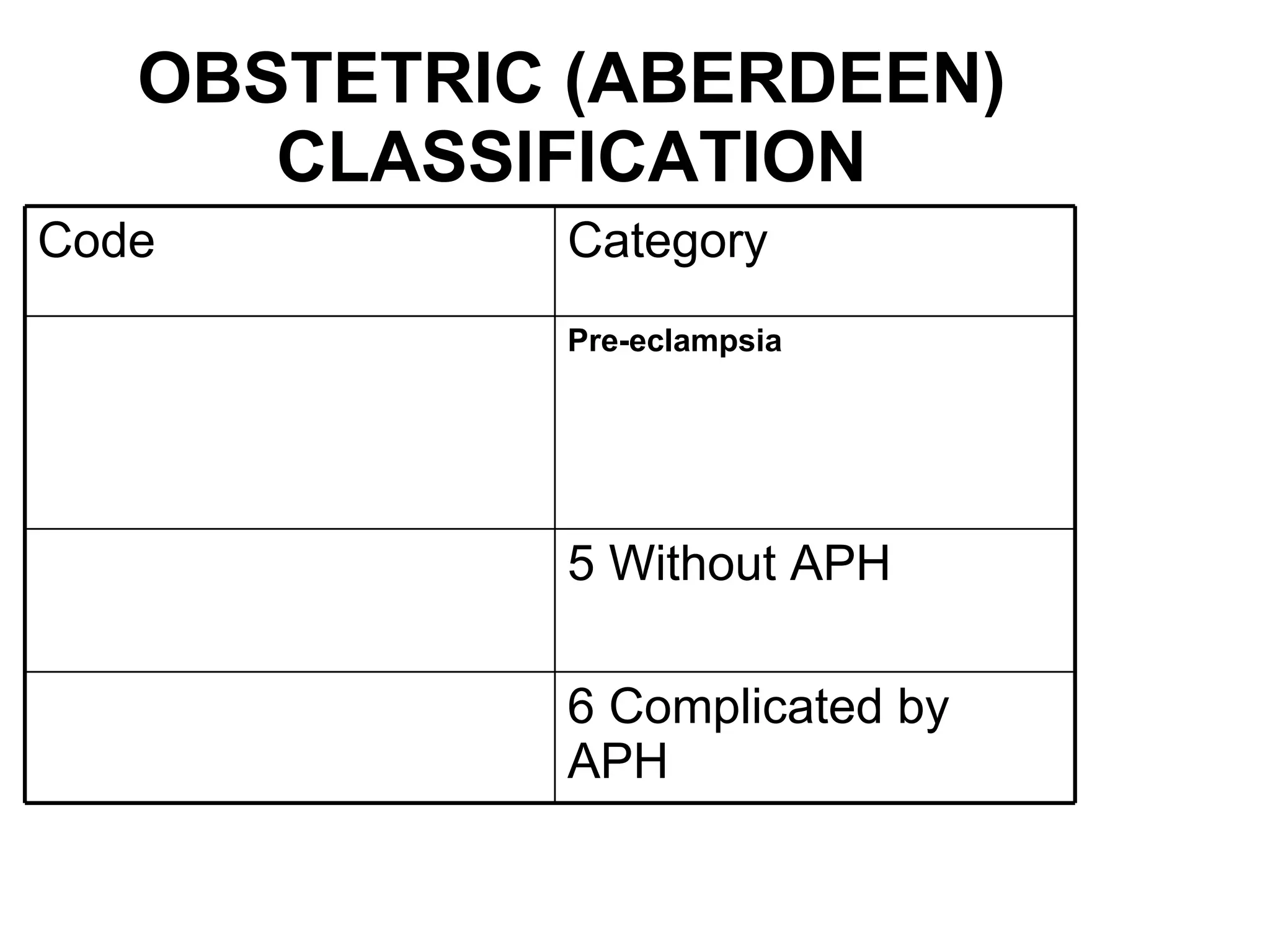
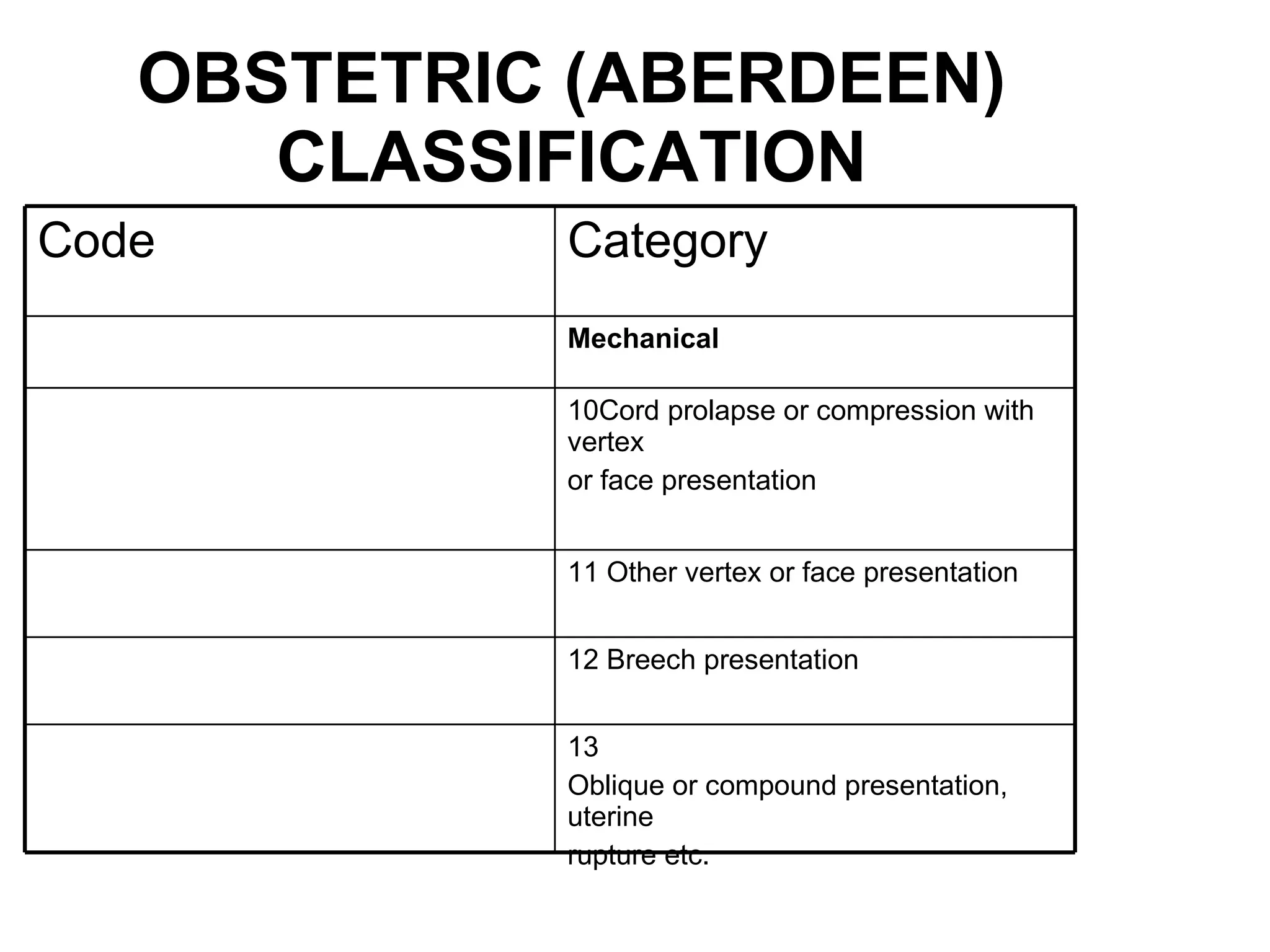
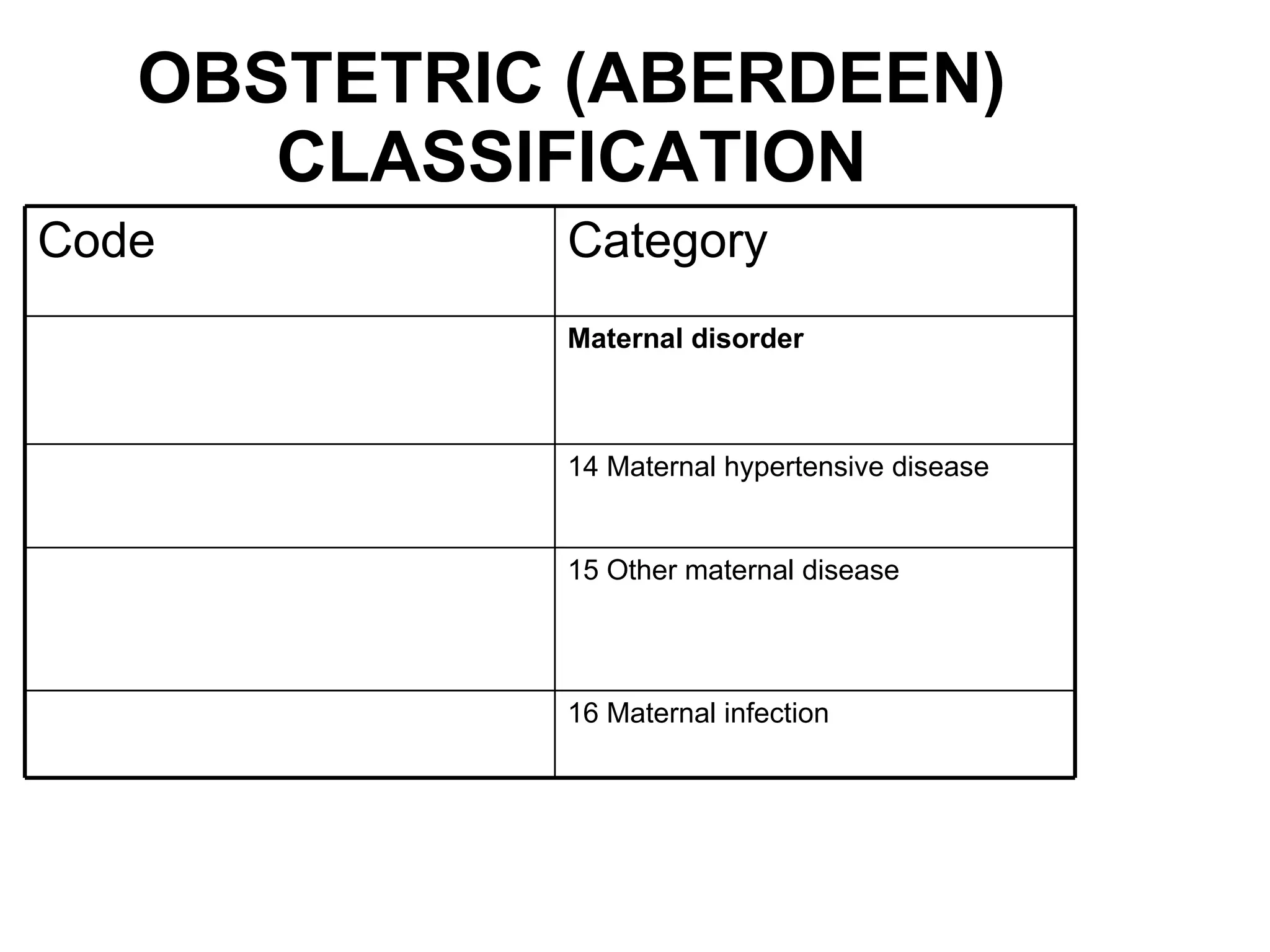
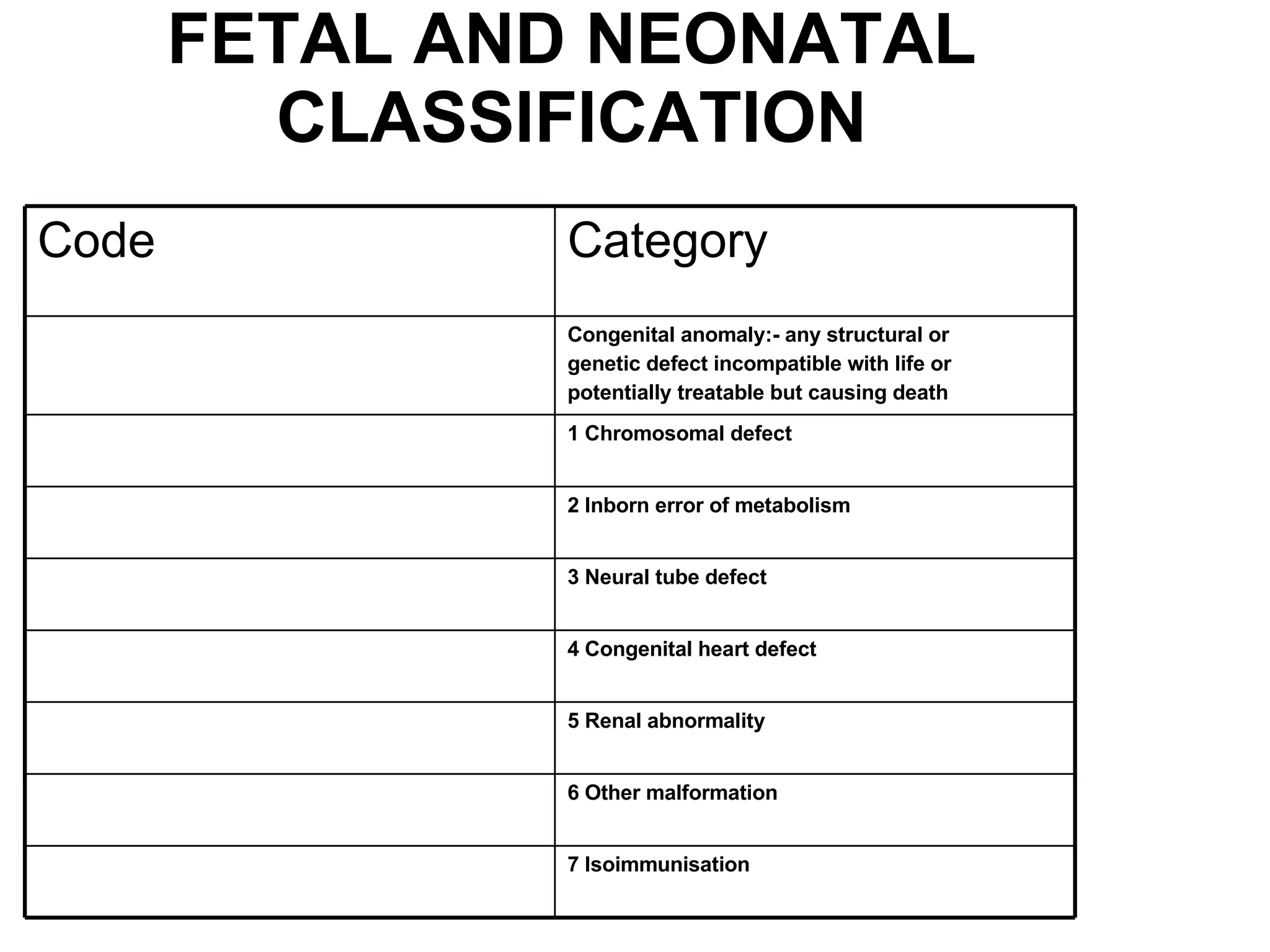
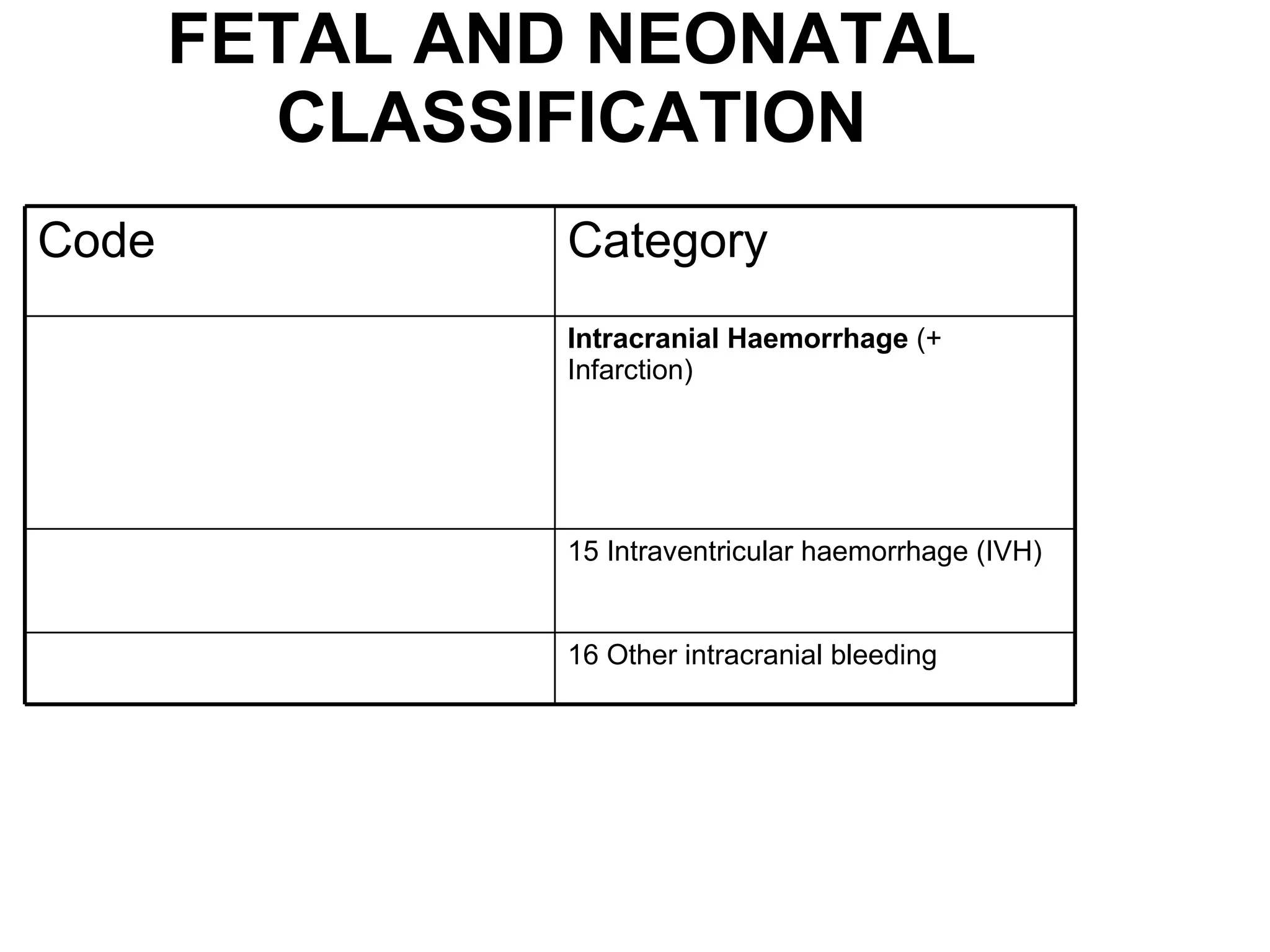
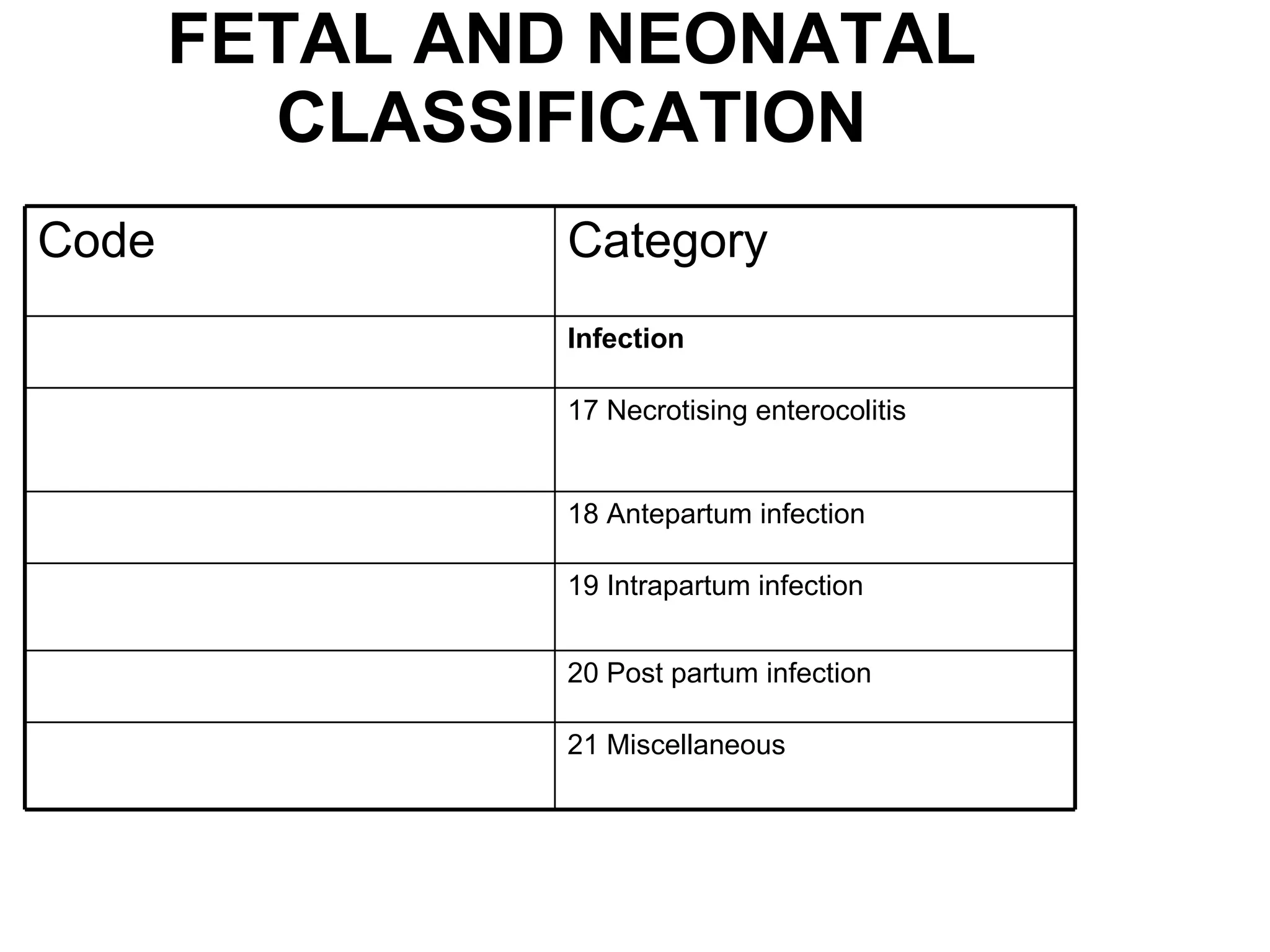
The document discusses various classification systems for stillbirths and neonatal deaths. It describes the ReCoDe classification system which categorizes stillbirths into 9 groups based on the relevant condition at death, including groups for fetal conditions, umbilical cord issues, placental problems, amniotic fluid abnormalities, uterine factors, maternal health conditions, intrapartum complications, trauma, and unclassified cases. It then outlines several other classification approaches including the Wigglesworth, Nordic-Baltic, and Aberdeen systems which categorize stillbirths and neonatal deaths based on factors like congenital anomalies, gestational age, infection, maternal conditions, and unexplained cases.