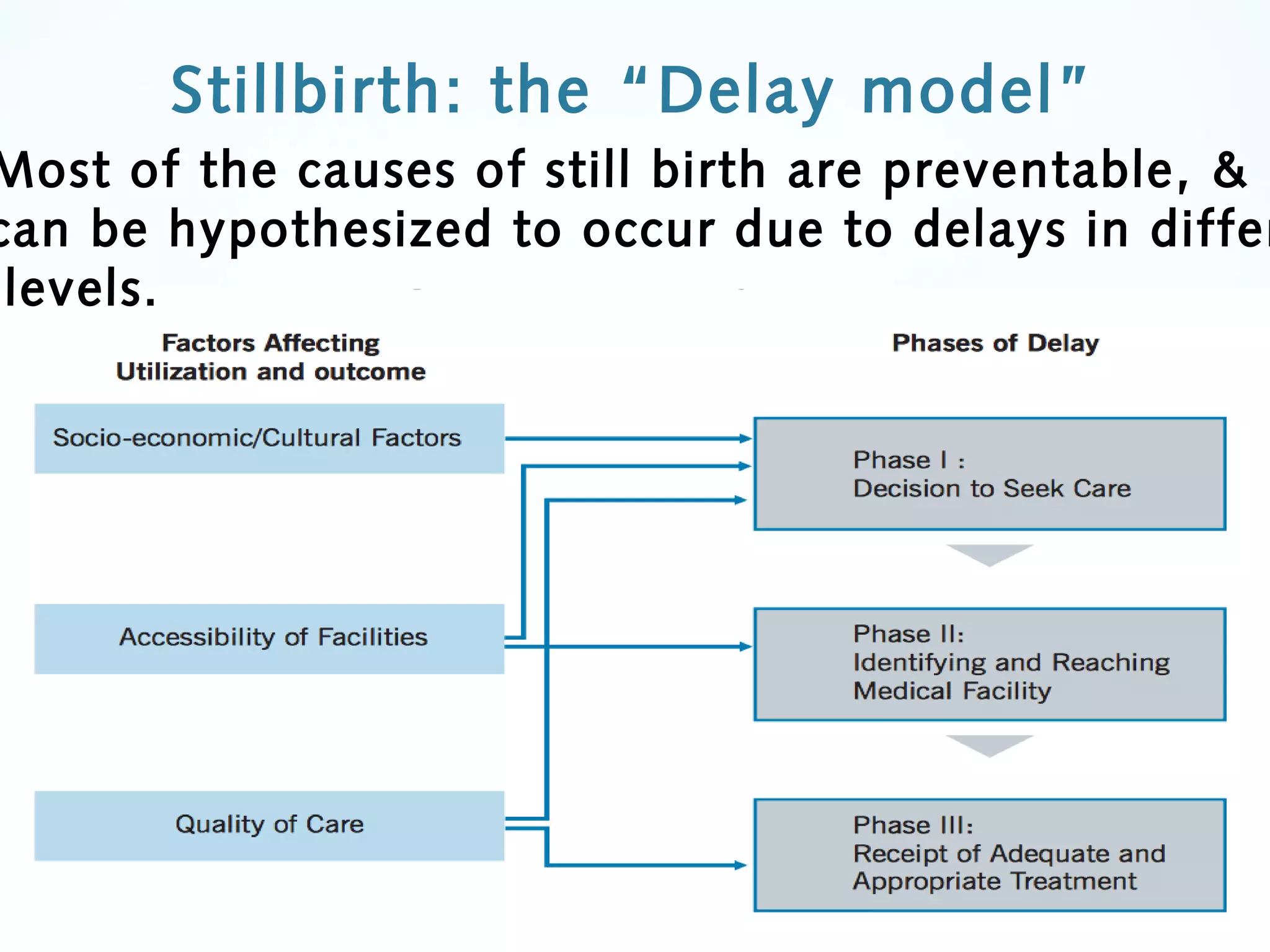
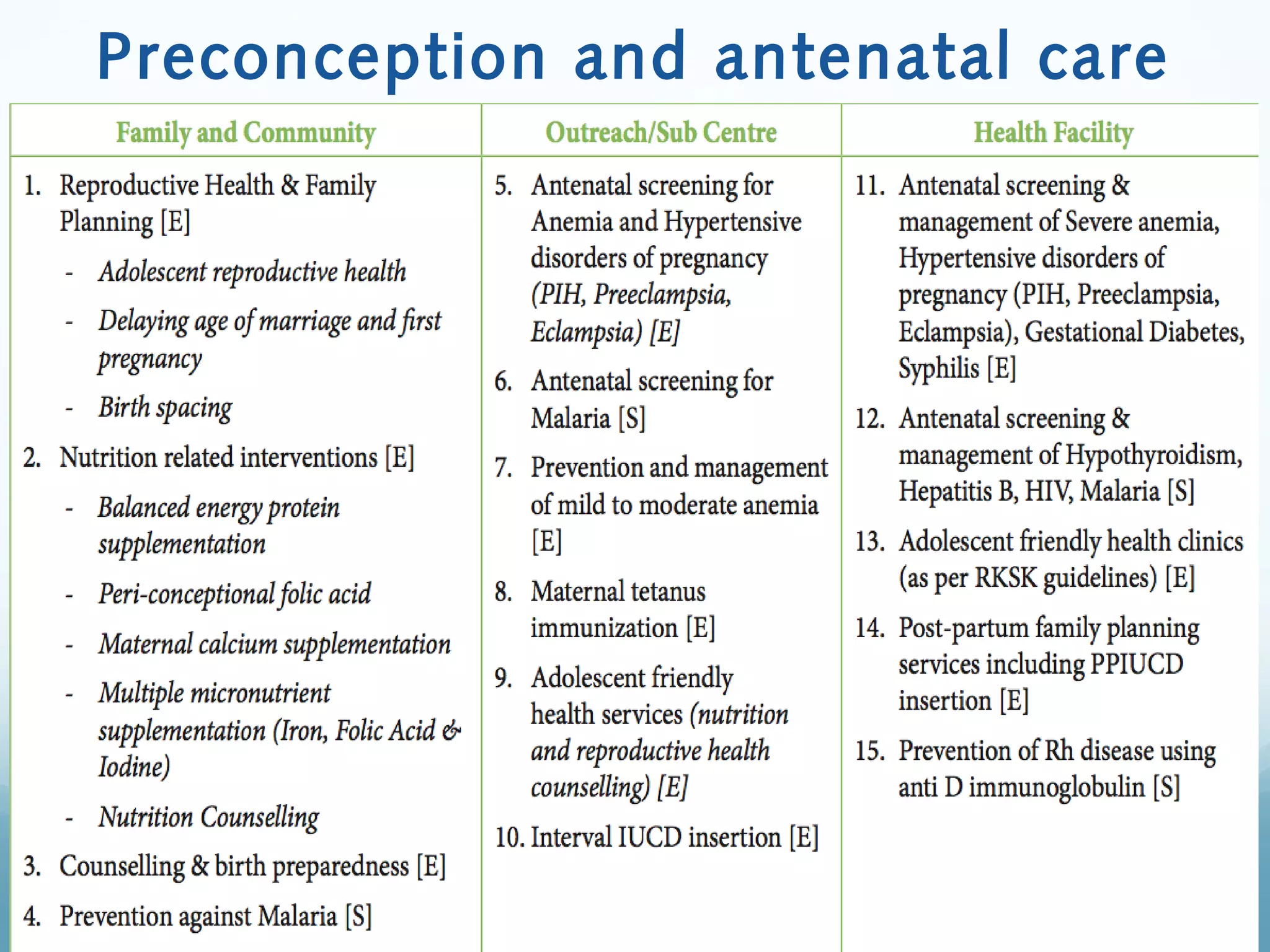
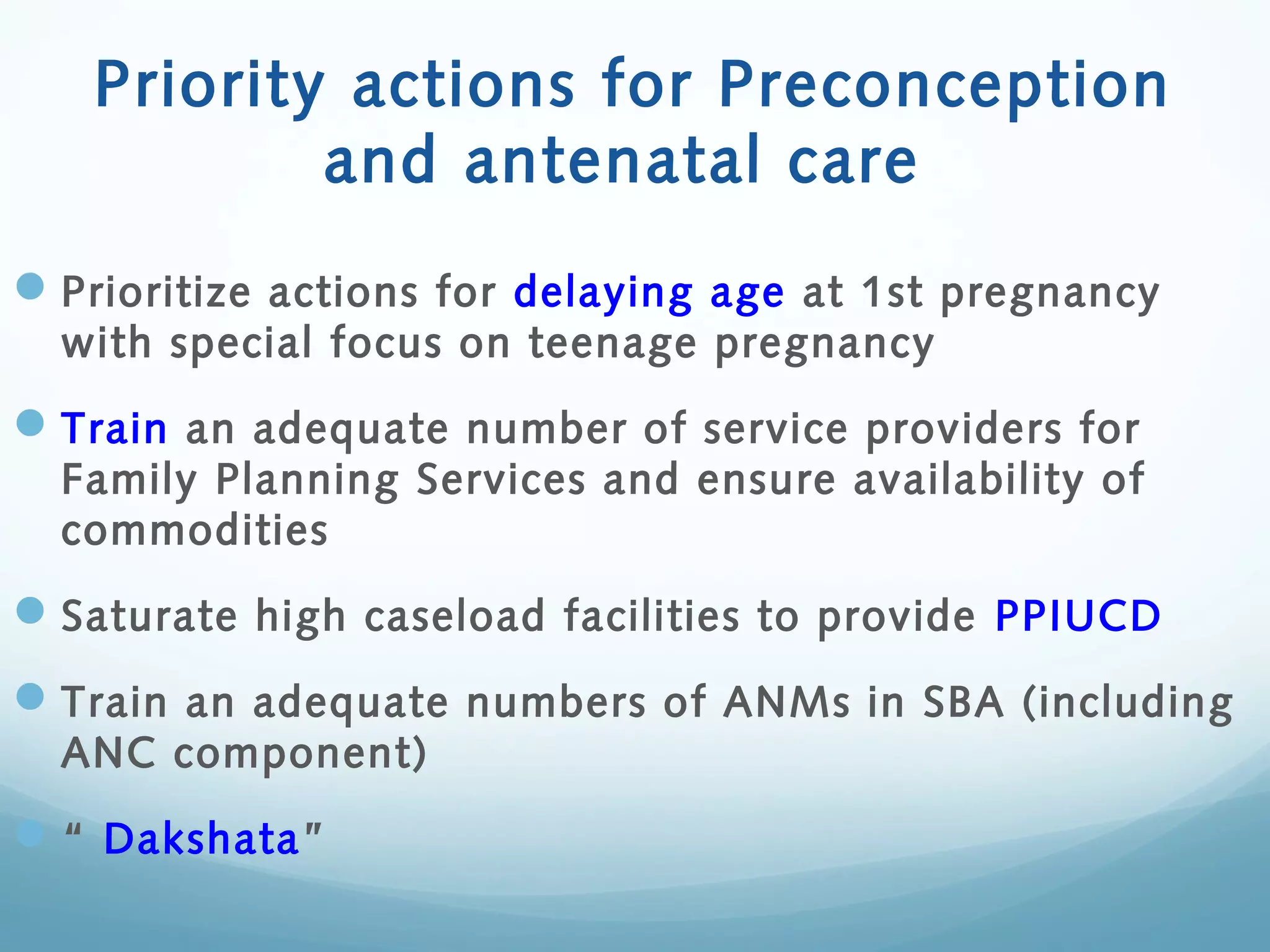
The document provides a comprehensive overview of the epidemiology of stillbirth in India, detailing its prevalence, causes, and classifications. It emphasizes the importance of addressing stillbirths as a key indicator of maternal and neonatal healthcare quality, with strategies for reducing stillbirth rates outlined in the India Newborn Action Plan. Additionally, it highlights the psycho-social and financial impacts of stillbirth on families and communities, calling for increased awareness and advocacy to address this significant public health issue.