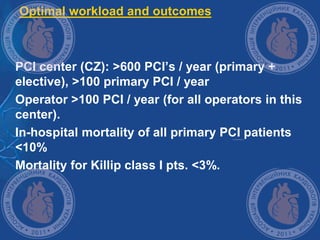
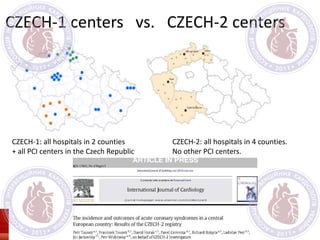
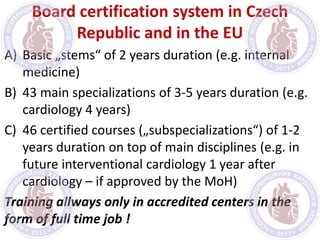
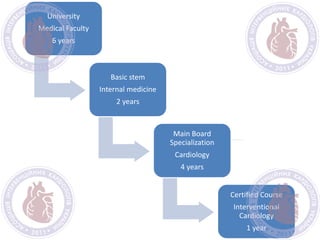
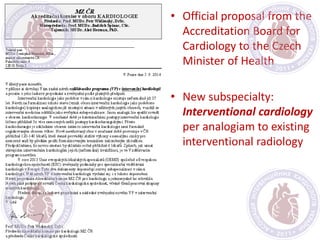
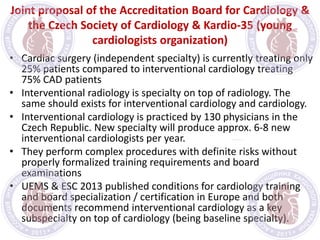
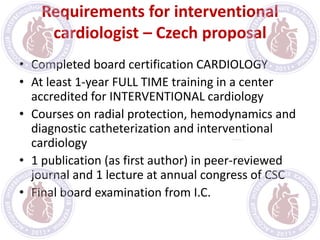
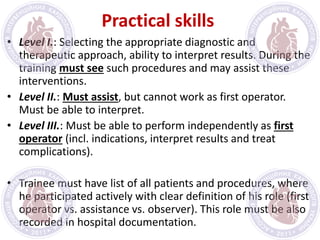
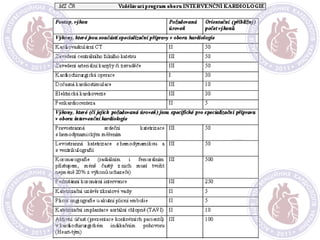
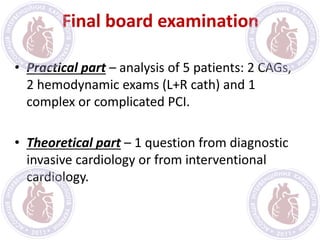
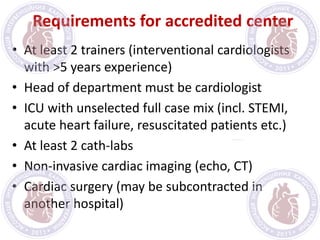
The document proposes new certification requirements for interventional cardiologists in the Czech Republic based on European models. It recommends interventional cardiology become a certified subspecialty after completing cardiology training. The proposed requirements include 1 year of full-time interventional cardiology training, courses, publications, and a final board exam. Accredited centers must have experienced trainers, cath labs, ICU, and imaging. Up to 100 experienced interventional cardiologists could be initially certified without the exam to start the program.