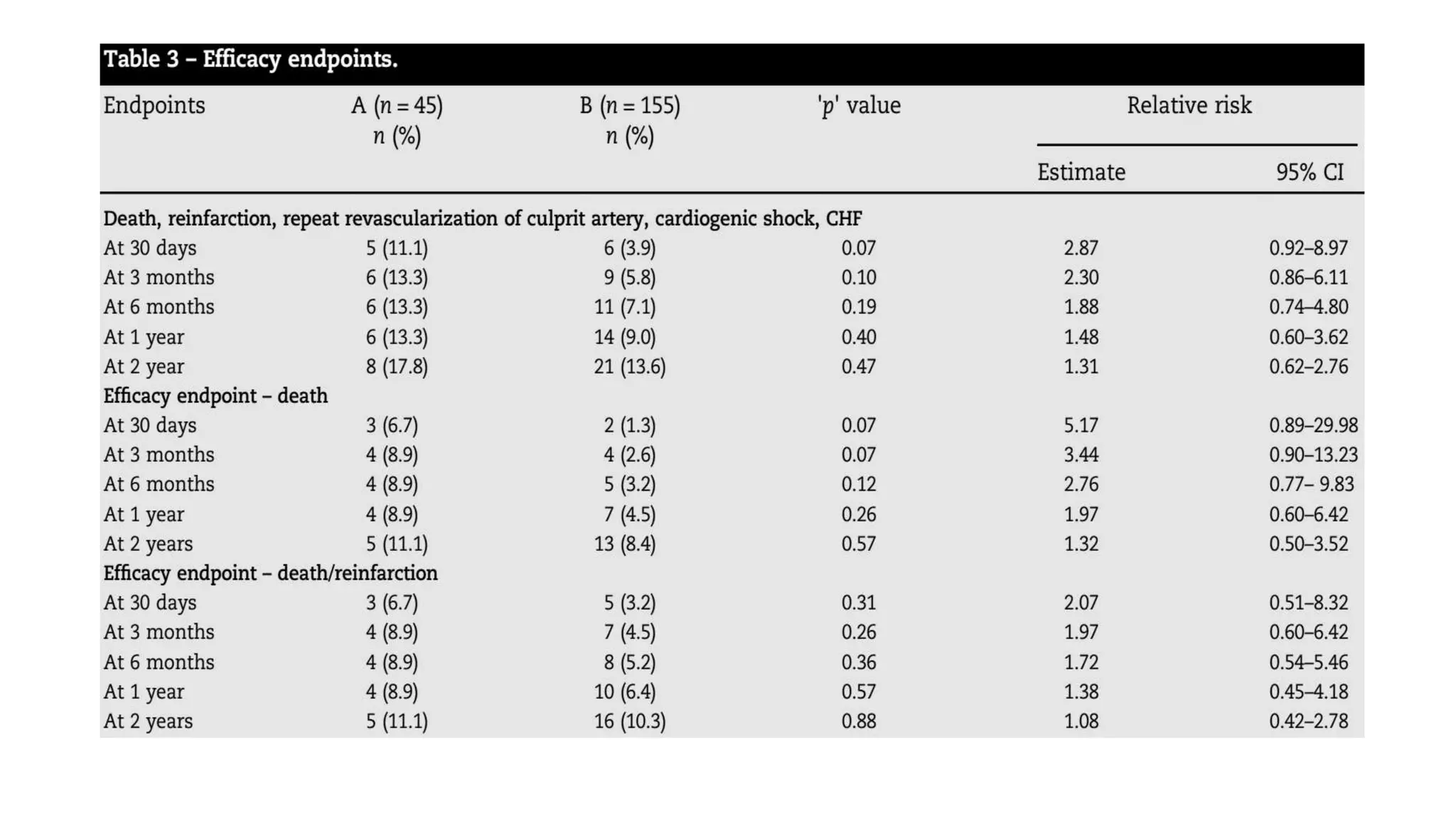
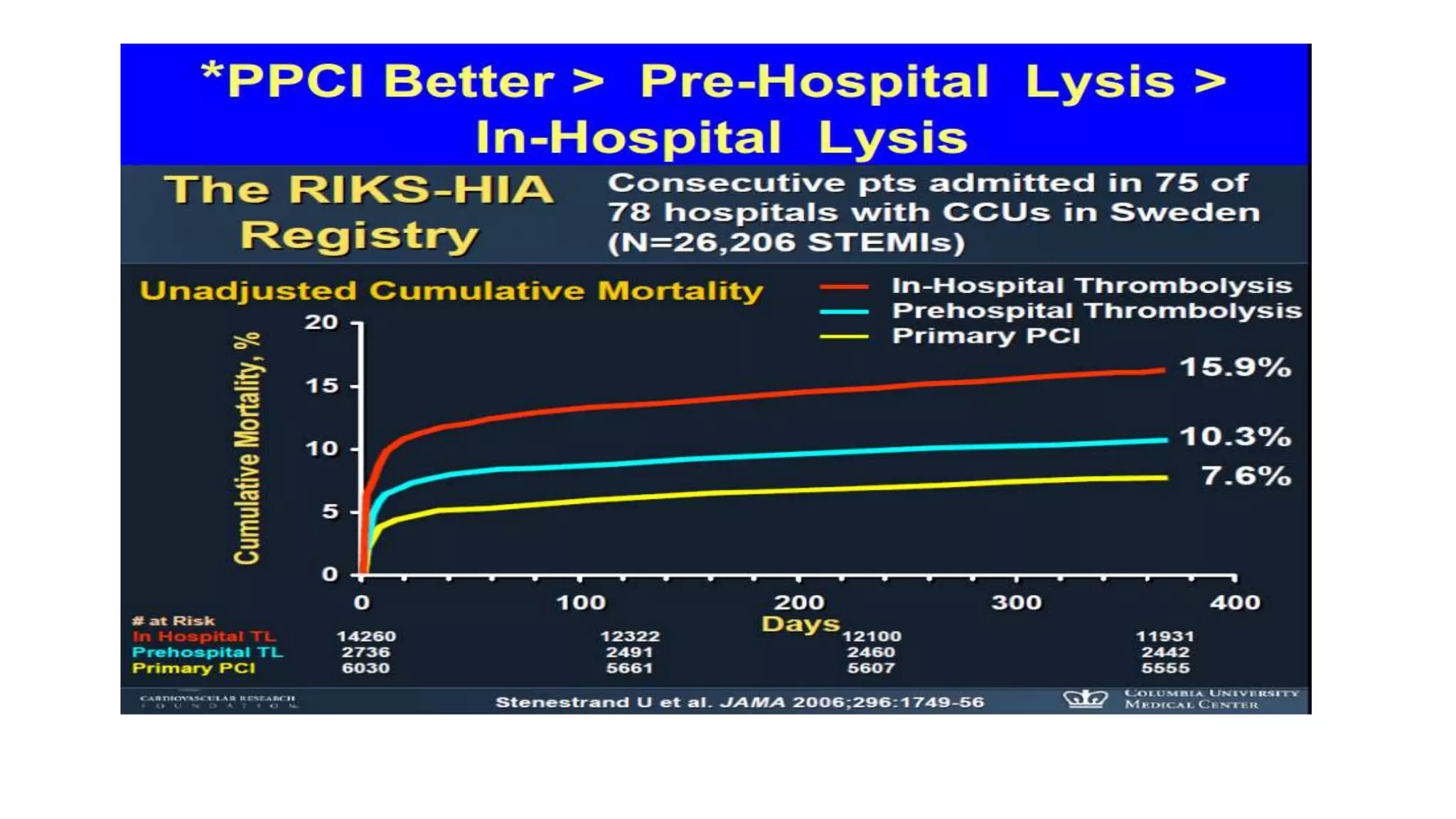
This study compared outcomes of a pharmacoinvasive strategy (tenecteplase fibrinolysis followed by early angiogram and PCI if needed) versus primary PCI in Indian patients with STEMI over 2 years. The pharmacoinvasive strategy resulted in similar outcomes to primary PCI at 2-year follow-up, with no differences in the composite primary endpoint of death, shock, reinfarction, revascularization or heart failure. Initially, primary PCI seemed more beneficial but by 2 years the groups were similar, suggesting fibrinolysis followed by angiogram is a reasonable alternative when PCI is not immediately available. The pharmacoinvasive strategy had benefits like less thrombus burden and higher rates of open arteries. This supports adopting such a strategy where delays
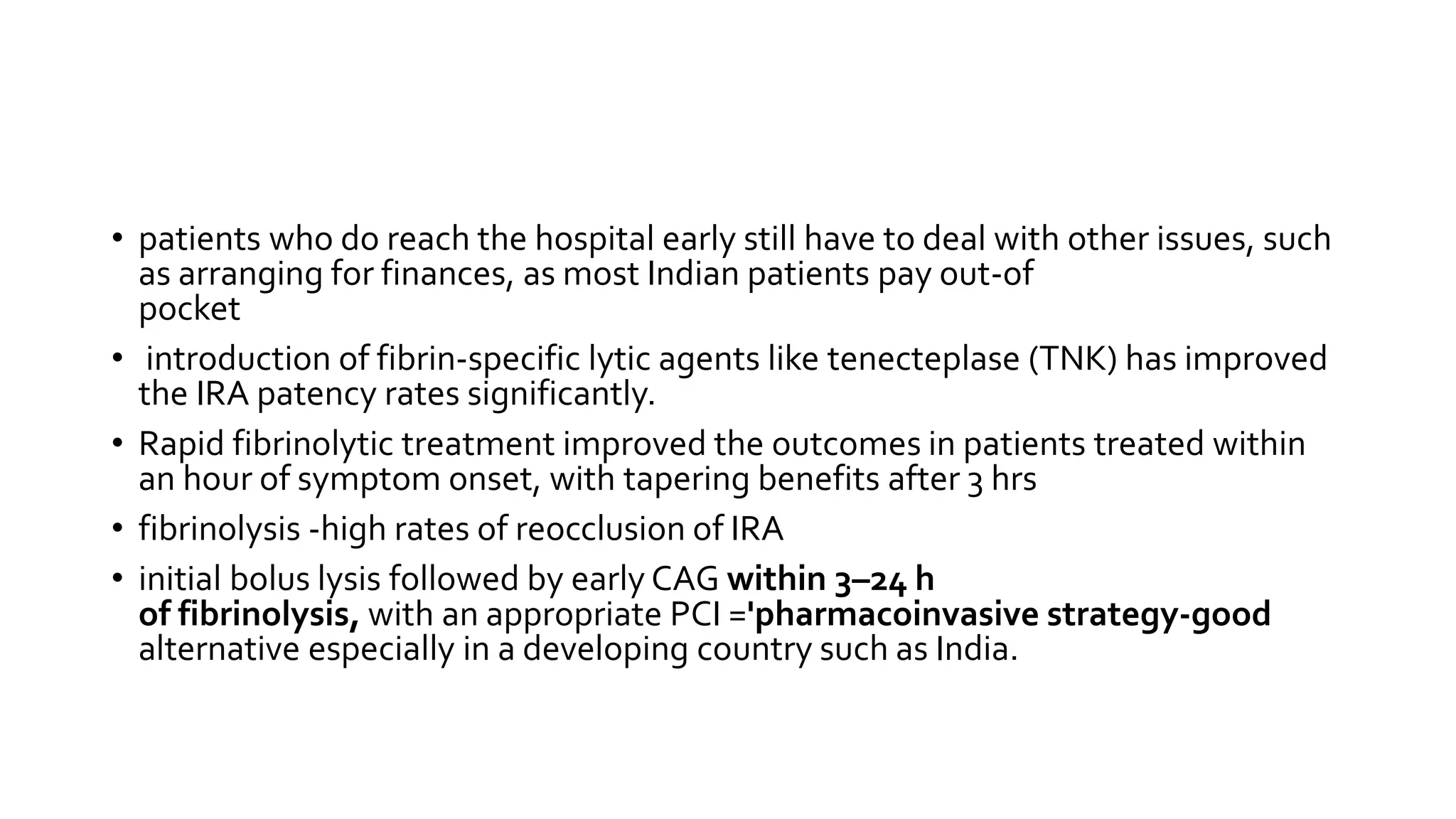




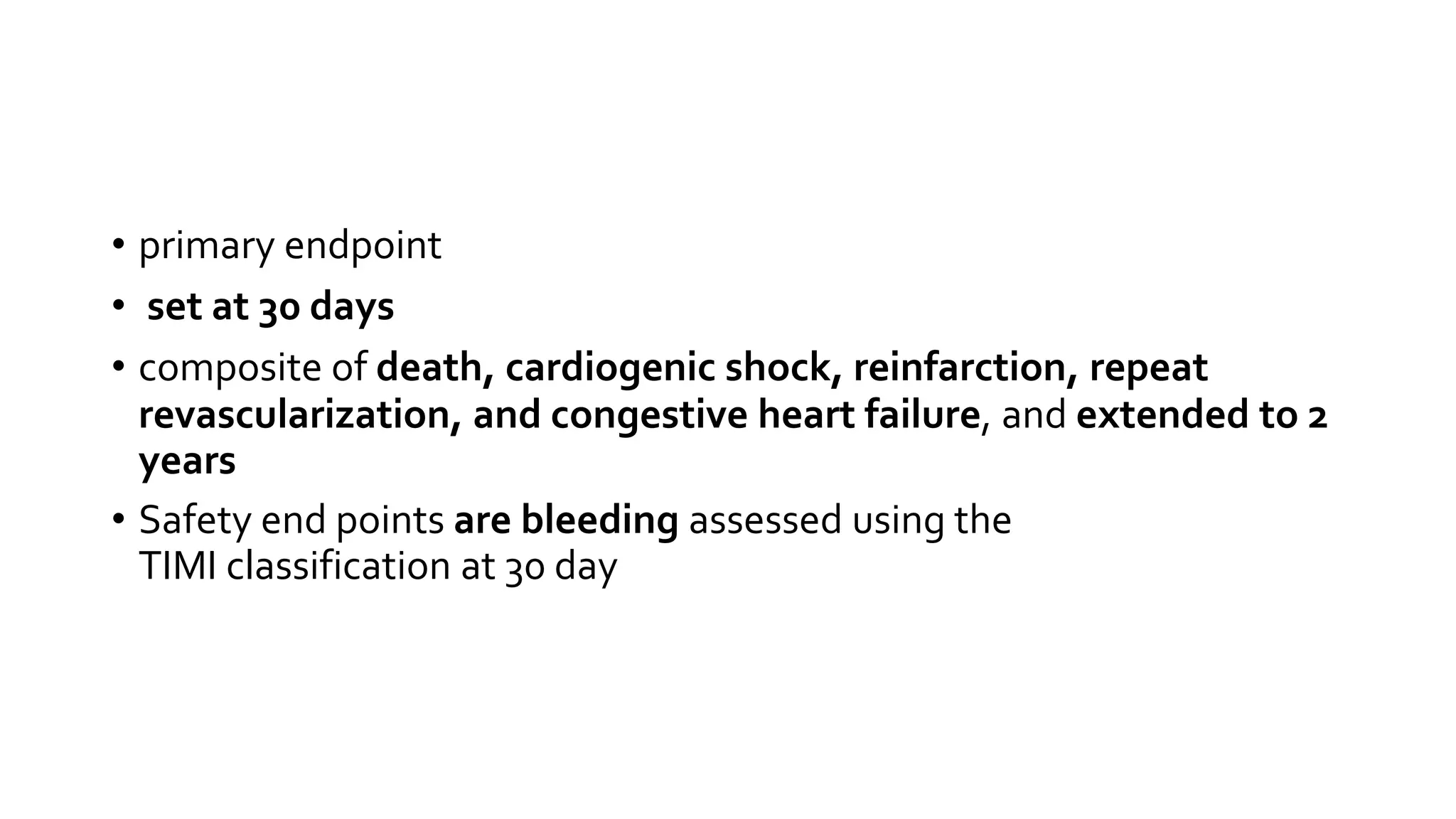
![Comparison of primary angioplasty and pre-
hospital fibrinolysis in acute myocardial
infarction (CAPTIM) trial: a 5-year follow-up
• primary angioplasty (n = 421)VS pre-hospital fibrinolysis (rt-PA) with
immediate transfer to a centre with interventional facilities (n = 419)
all-cause mortality at 5 years
• 9.7% in the pre-hospital fibrinolysis group
• 12.6% in PPCI [ P = 0.18].
patients included within 2 h, 5 year mortality
• 5.8% in the pre-hospital fibrinolysis group
• 11.1% in PPCI [HR 0.50 ( P = 0.04],
Patients included after 2 h, 5 year mortality
• 14.5 vs 14.4% [ P = 0.92].](https://image.slidesharecdn.com/pcivstlt2-160717071911/75/Pci-vs-tlt-2-17-2048.jpg)