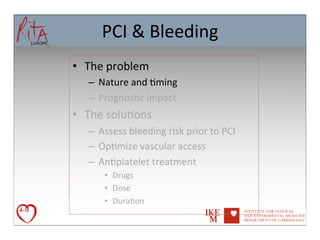
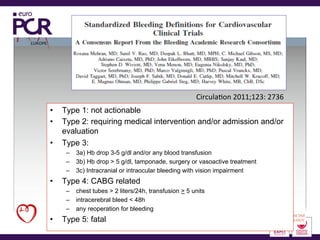
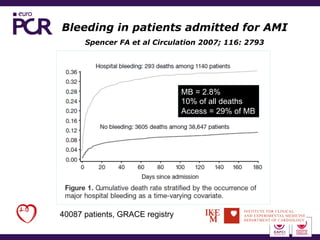
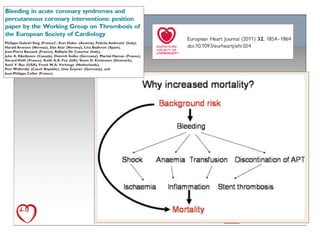
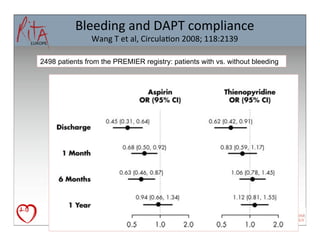
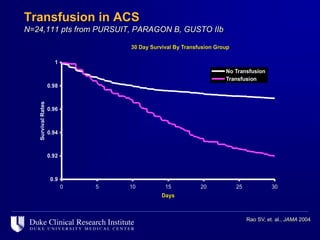
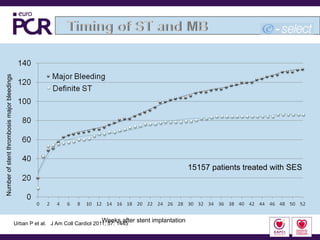
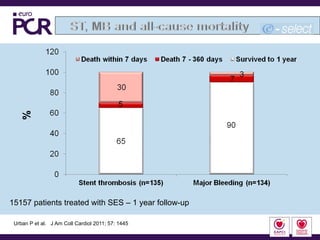
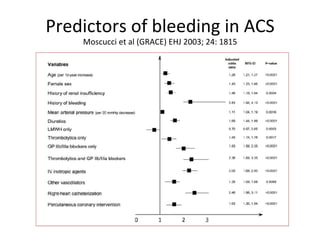
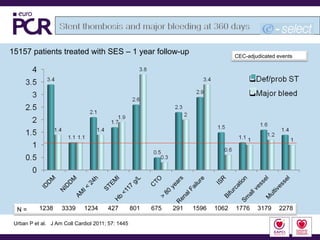
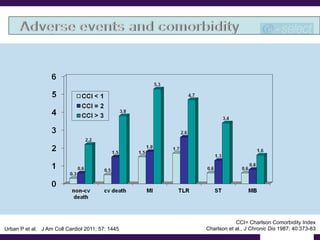
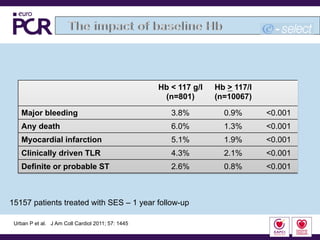
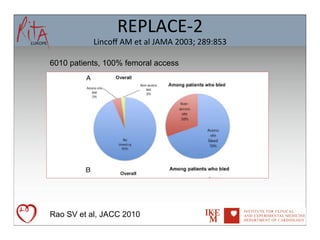
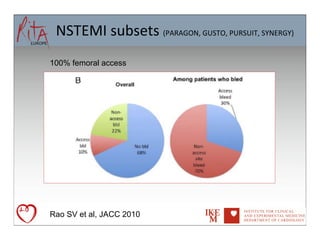
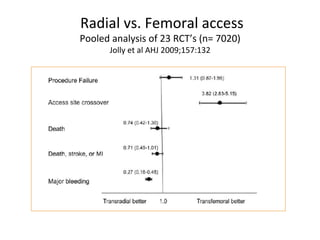
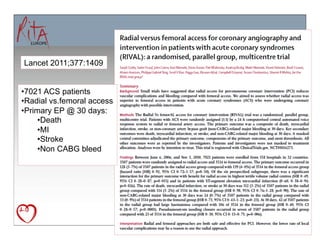
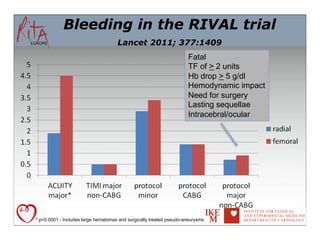
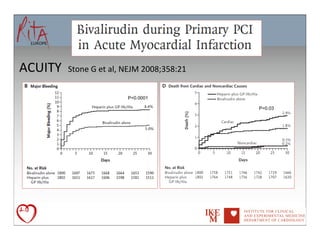
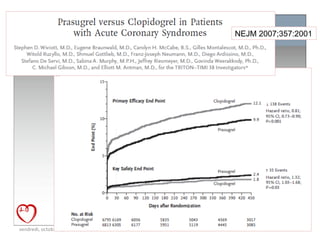
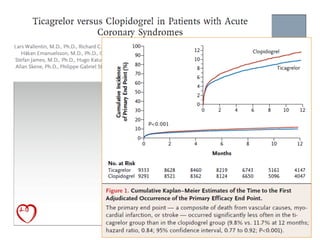
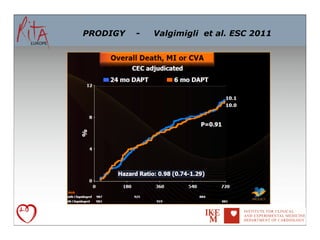
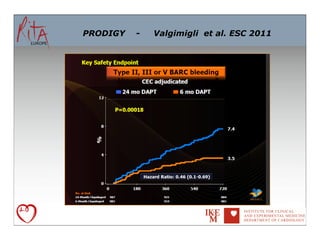
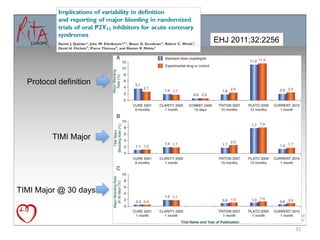
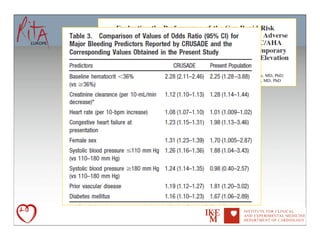
The document discusses bleeding as a complication of percutaneous coronary intervention (PCI) and antiplatelet therapy, noting that bleeding is associated with significantly increased mortality and morbidity, and that assessing bleeding risk, optimizing vascular access through the radial approach, and tailoring antiplatelet treatment can help address this problem. Major causes of bleeding include access site complications and prolonged dual antiplatelet therapy beyond 6 months without clear benefits.