This review examined the evidence for using virtual reality (VR) as a therapeutic modality for children with cerebral palsy (CP). A search of 13 databases identified 19 relevant articles, of which 13 studies from 11 articles were included. The studies documented outcomes in domains like brain plasticity, motor capacity, visual-perceptual skills, social participation, and personal factors. Two randomized controlled trials reported conflicting results for motor outcomes. However, 12 of the 13 studies found positive outcomes in at least one domain. The review concluded that VR has potential benefits for children with CP, but the current evidence is poor in methodological quality and empirical data is lacking. More rigorous randomized controlled trials are needed.
![Developmental Neurorehabilitation, April 2010; 13(2): 120–128
SUBJECT REVIEW
Virtual reality as a therapeutic modality for children with
cerebral palsy
LAURIE SNIDER, ANNETTE MAJNEMER, & VASILIKI DARSAKLIS
McGill University, School of Physical & Occupational Therapy, Montreal, Canada
(Received 1 September 2009; accepted 22 September 2009)
Abstract
Objective: The evidence for using virtual reality (VR) with children with cerebral palsy (CP) was examined.
Methods: A search of 13 electronic databases identified all types of studies examining VR as an intervention for children
with CP. The most recent article included was published in October 2008. For each study, the quality of the methods was
assessed using the appropriate scale. A total of 19 articles were retrieved. Thirteen studies from 11 articles were included
in the final analysis.
Results: Outcomes documented brain reorganization/plasticity, motor capacity, visual-perceptual skills, social participation
and personal factors. Two studies were randomized controlled trials. These reported conflicting results regarding motor
outcomes. Twelve of the 13 studies presented positive outcomes in at least one domain.
Conclusions: VR has potential benefits for children with CP. However, the current level of evidence is poor and empirical
data is lacking. Future methodologically rigorous studies are required.
Keywords: virtual reality, cerebral palsy, children
Resumen
Objetivo: Se reviso´ la evidencia sobre el uso de realidad virtual (VR) en nin˜os con para´lisis cerebral.
Me´todos: Una bu´squeda en 13 bases de datos electro´nicas identifico´ todos aquellos estudios respecto al uso de VR como una
intervencio´n para nin˜os por CP: El artı´culo ma´s reciente fue publicado en Octubre de 2008. Para cada estudio, se determino´
la calidad de los me´todos utilizando las escalas adecuadas. Un total de 19 artı´culos fueron recabados. Trece de los 11
artı´culos fueron incluidos en el ana´lisis final.
Resultados: Los resultados documentados fueron reorganizacio´n/plasticidad cerebral, capacidad motriz, habilidad
visuoespaciales, participacio´n social y factores personales. Dos estudios eran ensayos clı´nicos aleatorizados. Estos estudios
arrojaron resultados conflictivos respecto a los resultados motrices. Doce de los trece estudios presentaron resultados
positivos por lo menos en una de las a´reas.
Conclusiones: La realidad virtual tiene efectos potencialmente bene´ficos en nin˜os con para´lisis cerebral. Sin embargo, el
actual nivel de evidencia es pobre y falta informacio´n empı´rica. Se ameritan nuevos estudios metodolo´gicamente estrictos.
Palabras clave: realidad virtual, para´lisis cerebral
Introduction
Virtual reality (VR) is a virtual environment (VE)
system that uses a range of computer technologies to
present virtual or artificially generated sensory infor-
mation in a format that enables the user to perceive
experiences that are similar to real-life events and
activities [1]. Considering that computer technology
is enticing and intrinsically motivating for children
and adolescents, VR has sparked recent interest as
a new treatment modality for children and youth
with cerebral palsy (CP). CP is a non-progressive
disorder which affects the brain in the early stages
of development, primarily damaging the areas
responsible for the control of movement and pos-
ture [2]. Although no cure is available, therapies,
assistive devices and education are beneficial
in increasing functional independence and partici-
pation [3].
Currently, the popularity of computer technology
among children and adolescents, with or without
Correspondence: Dr Laurie Snider, OT, PhD, McGill University, School of Physical & Occupational Therapy, 3654 Sir-William-Osler Drive, Montreal, H3G
1Y5 Canada. E-mail: laurie.snider@mcgill.ca
ISSN 1751–8423 print/ISSN 1751–8431 online/10/020120–9 ß 2010 Informa UK Ltd.
DOI: 10.3109/17518420903357753](https://image.slidesharecdn.com/virtualrealityasatherapeuticmodalityforchildrenwith-170619015915/75/slide-1-2048.jpg)
![disabilities, is on the rise, as testified by the docu-
mented increase in use of consumer electronics by
this sub-set of the population [4]. In fact, approx-
imately one in four children own a video game
console, such as the Nintendo Wii or Sony
PlayStation, at home [4]. Consequently, it can be
assumed that children and the youth today are
familiar with this type of technology as it may be
used for leisure and as a method of socialization.
Current VR systems, such as the IREX, are expen-
sive and inaccessible to most of the population [5].
However, interest in commercially available gaming
consoles as a therapeutic medium has been gaining
popularity [6, 7]. Some benefits of technology use
identified by individuals with disabilities are com-
munication with others, the development of social
relationships, as well as the promotion of control,
skill competencies and independence [8].
In rehabilitation, VR is used to create interactive
play environments in order to achieve specific
treatment goals. The primary purpose of VR as a
treatment modality is to improve competence and
confidence in motor-based activities and to engage
in play-based activities that are otherwise inaccessi-
ble in the real world [9, 10]. Virtual environments
can be sub-divided into two types: (1) immersion
VR, which consists of viewing the environment via
screens in a head-mounted display and (2) desktop
VE, which projects the desired image onto a com-
puter or TV screen with sound provided by external
speakers [1]. Tactile feedback (e.g. through a glove)
and force feedback (e.g. resistance in a joystick or
steering wheel) can also be provided in VE [1].
Motor learning theory places great emphasis on the
role of practice and feedback on the development
of proper motor performance as the motor patterns
learned are reinforced through these techniques [9,
11, 12]. VR therapy incorporates fundamental
principles of motor learning theory by allowing the
users to continuously monitor their performance
via a spatial representation of their movements on
the computer screen. With the goal of increasing
functional independence in everyday tasks, VR
provides opportunities for repeated practice and
positive feedback [13]. Users are also informed of
the results of their motor performance (e.g. their
score) through virtual games [9, 12]. Further
advantages include the possibility for the treating
therapist to grade the activities to meet the abilities
of the user as well as to facilitate the exploration of
complex environments that would otherwise be
inaccessible to children with CP due to mobility
restrictions. Early research studies demonstrate that
this modality is feasible, highly enjoyable and
non-threatening [10]. Furthermore there is recent
evidence demonstrating the effectiveness of VR as a
therapeutic intervention for upper limb motor
recovery in adult stroke rehabilitation [14].
Therefore, it can be hypothesized that these results
may be extrapolated to other brain-injured popula-
tions, such as children with CP. This systematic
review seeks to synthesize the available evidence on
this population of interest.
Purpose
To guide future research and clinical intervention,
this study conducted a structured review of the
existing evidence on the therapeutic use of VR with
children with CP. The outcomes investigated in this
review were categorized according to the dimensions
of the International Classification of Functioning,
Disability and Health (ICF): body functions
(e.g. physiological, psychological); structures (e.g.
anatomical); activities (tasks); and participation
(life roles) [15].
Methods
Primary research question
An a priori PICO question was developed to aid
in the search for articles that would comprise this
review [16]: Does training using a play-based VR
intervention improve outcomes (brain reorganiza-
tion/motor skills/spatial skills/motivation and play-
fulness/functional everyday self-care and leisure
activities) in children with cerebral palsy? PICO is
defined as:
. Population: Children with CP;
. Intervention: Virtual games;
. Comparison: Compared to baseline or to a control
group; and
. Outcome: Measures of body structure (fMRI),
body function (motor skills, quality of move-
ments, visual-spatial skills), activity and participa-
tion (self-care and leisure activity performance,
playfulness), personal factors (motivation,
self-perception, self-efficacy).
Systematic review of the literature
The electronic databases MEDLINE: 1950 to week
2, June 2009, PsychINFO: 1806 to week 1, June
2009, CINAHL, ERIC, HealthSTAR: 1966 to May
2009, PEDro, Cochrane database of Systematic
Reviews, Cochrane Central Register of Controlled
Trials, CIRRIE, EMBASE: 1980 to week 25, 2009,
Health and Psychosocial Instruments: 1985 to April
2009, OTSeeker and RehabData were searched
using the key words: tetraplegi*, spastic*, quad-
riplegi*, quadrapare*, pes equinus*, monoplegi*,
little* disease, hypotoni*, hemiplegi*, hemipare*,
dystoni*, diplegi*, dyskine*, choreoathe*, atheto*,
Virtual reality as a therapeutic modality 121](https://image.slidesharecdn.com/virtualrealityasatherapeuticmodalityforchildrenwith-170619015915/75/slide-2-2048.jpg)
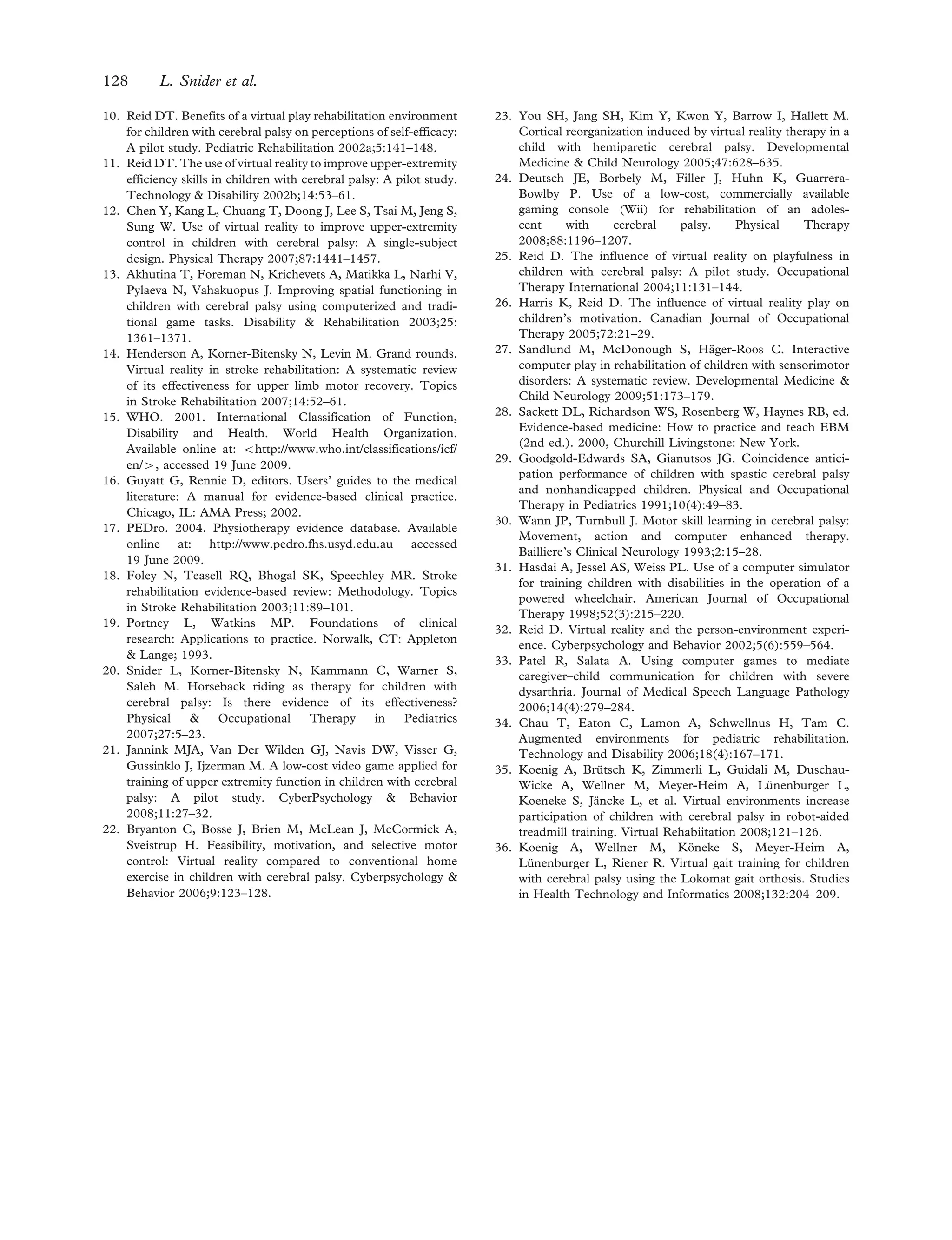
![ataxi*, cerebral palsy, VR, virtual environment,
computer* game* and computer* simulation*.
Only English or French manuscripts were included.
Studies including individuals 18 years of age and
younger as well as all study designs (e.g. randomized
controlled trials (RCTs), quasi-experimental, case
series, case studies) were considered. Articles that
were excluded focused predominantly on individuals
with stroke, traumatic brain injuries, physical dis-
abilities or adults. A total of 13 studies from 11
articles were retrieved for final analysis. A detailed
flowchart of the search strategy and exclusion
process can be found in Figure 1.
Quality assessment
The following information was extracted from each
study: author/date, design, participants, exposure/
intensity, outcomes and significance and ICF com-
ponent assessed. Studies were classified as either
observational or experimental. Experimental studies,
which are higher quality than observational studies,
use comparable control groups, random assignment,
blinding (of assessors, therapists and subjects) and/
or report on subject attrition. The two RCTs
retrieved were rated for methodological quality
using the Physiotherapy Evidence Database
(PEDro) rating scale [17]. According to Foley
Run searches on all relevant
databases and sources
June 2009
Articles
excluded
(n= 521)
Exclusion
criteria
(by title
/abstract)
– Not CP
– Not children
– Not VR
– Duplicates
Total Articles
included
(n= 19)
(Full text
obtained)
Reference
lists
reviewed
and articles
added (n=0)
Articles excluded*: Format (n=4)
Total articles
obtained for
second
screen
(n= 19)
Total articles
considered
eligible after
full-text review
(n= 11)
13 studies from 11 articles included in
the final analysis
Cochrane (SR)
Included: 0
Excluded: 5
PsychInfo
Included: 14
Excluded: 37
Medline
Included: 11
Excluded: 183
OT Seeker
Included: 2
Excluded: 0
RehabData
Included: 2
Excluded: 0
Cochrane (CT)
Included: 1
Excluded: 10
HAPI
Included: 1
Excluded: 0
CINHAL
Included: 11
Excluded: 40
PeDRO
Included: 0
Excluded: 0
ERIC
Included: 1
Excluded: 11
HealthStar
Included: 12
Excluded: 126
Articles excluded*: Population (n=3)
Articles excluded*: Outcomes (n=1)
*see Table III
EMBASE
Included: 12
Excluded:
CIRRIE
Included: 0
Excluded: 0
Figure 1. Flowchart of search strategy and selection process.
122 L. Snider et al.](https://image.slidesharecdn.com/virtualrealityasatherapeuticmodalityforchildrenwith-170619015915/75/slide-3-2048.jpg)
![et al.’s [18] quality assessment, studies scoring 9–10
on the PEDro scale are considered to be method-
ologically ‘Excellent’, 6–8 ‘Good’, 4–5 ‘Fair’ and
below 4 ‘Poor’. Observational study designs
included in this review consist of quasi-experimental
or descriptive pre–post designs [19]. These designs
do not include randomization and, in some cases,
subjects act as their own controls. Level of evidence
ratings are based upon a modified Sackett score
adapted to include PEDro ratings (see Table I) [28].
These levels have been described in greater detail
in other work by Snider et al. [20].
Results
Study characteristics
The data extracted from the 13 eligible studies is
summarized in Table II. A summary of excluded
articles is found in Table III.
Categorization according to ICF components
In children with CP, is VR therapy more effective than
no intervention, placebo intervention, or an alternative
intervention for body functions and body structure
outcomes?
One ‘good’ pilot RCT involving 31 children with CP
investigated this question; however, no significant
results were yielded [9]. One ‘fair’ exploratory RCT
with a sample size of 10 children revealed that scores
on the Melbourne Assessment of Unilateral Upper
Limb Function either improved or stayed the same
in the experimental group. The highest percentage
change between pre- and post-test coincided with
the results of two children from the experimental
group [21].
One quasi-experimental study consisting of 45
children found that visual-spatial abilities in the
treatment group improved more compared to the
control group [13]. In another quasi-experimental
study of 21 children conducted by the same authors,
no difference in the spatial functioning between
the control and experimental groups was found [13].
In an observational study investigating the kinemat-
ics of ankle dorsiflexion during VR therapy as
compared to conventional exercises, it was found
that more repetitions were completed when follow-
ing a conventional exercise programme. Children
also required more time to complete one set of VR
exercises. However, on average, a longer hold time
for VR exercises as well as a greater mean for ankle
dorsiflexion ankle range of motion was noted during
VR exercises [22]. A single-subject design study
investigated the reaching kinematics and fine motor
abilities of four children between the ages of 4–8
years with CP. Descriptive analysis of the results
revealed that 75% of the children showed qualitative
improvement in the reaching kinematics, which
was partially maintained 4 weeks post-treatment.
Fine motor scores improved for all children and 75%
of the children showed increased scores on the
visual-motor integration sub-test of the Peabody
Developmental Motor Scales–2nd edition [12].
Three case studies have also been published
addressing this question. One revealed improved
scores on the Bruininks-Oseretsky Test of Motor
Proficiency accuracy score; however, no consistent
effect in the quality of upper extremity movements
was detected [11]. Another study indicated
improved quality of movement of the affected
upper limb as well as a greater activation of the
contralateral sensorimotor cortex [23]. In the last
case study, it was found that following VR therapy,
visual-perceptual processing improved, as well as
postural control, weight distribution and functional
mobility [24]. In summary, there is conflicting
evidence (primarily Level 4) that VR therapy is
effective in enhancing body structures or functions
when compared to traditional or no intervention.
However, the results from both RCTs are prelimi-
nary and the remaining evidence originates from
Table I. Levels of evidence (adapted from Sackett).
Level Description
1a (Strong) Well designed Meta-Analysis or two or more ‘high’ quality RCT’s (PEDro ! 6) showing similar findings
1b (Moderate) 1 RCT of ‘high’ quality (PEDro ! 6)
2a (Limited) At least 1 ‘fair’ quality RCT (PEDro ¼ 4–5)
2b (Limited) At least one ‘poor’ quality RCT (PEDro 5 4) or well-designed non-experimental study (non-randomized
controlled trial, quasi-experimental studies, cohort studies with multiple baselines, single subject series with
multiple baselines, etc.)
3 (Consensus) Agreement by an expert panel or a group of professionals in the field or a number of pre–post studies all with
similar results
4 (Conflict) Conflicting evidence of two or more equally well designed studies
5 (No evidence) No well-designed studies—only case studies/case descriptions or cohort studies/single subject series with no
multiple baselines)
Virtual reality as a therapeutic modality 123](https://image.slidesharecdn.com/virtualrealityasatherapeuticmodalityforchildrenwith-170619015915/75/slide-4-2048.jpg)
![TableII.Summaryofstudiesonvirtualreality.
Reference
Subjects;samplesize;
agerangeMethodologyOutcomemeasures/Variables*Mainfindings
[10]Spasticquadriplegiaor
diplegia;n¼3;8–12
years
Casestudy,pre/posttest
design,two90minute
sessionsperweek,
4weeks
CanadianOccupationalPerformance
Measure(COPM)—mainlyself-care
andleisureactivitieswereidentified
Performanceandsatisfactionscoreswereratedhigheratpost-test
forallparticipants(clinicallysignificant).
Suggestsbeneficialeffectswithrespecttoself-efficacy.Descriptive
analysis&graphicpresentation.
[11]Spasticquadriplegiaor
diplegia;n¼4;8–12
years
Casestudy,pre/posttest
design;1.5hours/week,
8weeks
QualityofUpperExtremitySkillsTest
(QUEST),BOTMP(item6of
sub-test5—motoraccuracy)
ScoresimprovedontheBOTMPaccuracyscore.
Changeinqualityofupperextremitymovementswasvariable
(noconsistenteffect).
Descriptiveanalysis.
[13]Cerebralpalsy;n¼21;
7–14years;
12experimental,9control
Experimentaldesign;
30–60min/session,
6–8Âovera1month
period
Computer-based:KoosBlockDesignTest,
ClownAssemblyTestOthertests:
DecentrationofViewpointTest,
DirectionalPointingtoHiddenObject
Test,RavenProgressiveMatrices,
BentonJudgmentofLineOrientation
Test,Arrowssub-testofthe
NeuropsychologicalTestBatteryfor
Children,RoadsTest
Nosignificantchangeswereobserved(mostchildreninexperimental
groupwerenon-ambulatorywhereasmostcontrolswereambula-
tory).Descriptive&comparativestatistics(t-test;Chi-square).
Cerebralpalsy(mostdiple-
gia);n¼45;agenotspeci-
fied;23experimental,
22control
Experimentaldesign;
30–60min/session,
6–8Âovera1month
period
Visual-spatialabilitiesofthechildreninthetreatmentgroup
improvedmorecomparedtothecontrolgroup.
Descriptive&comparativestatistics(t-test,chi-square,ANOVA).
[25]Cerebralpalsy;n¼13;
8–12years
Observationalstudy
(videotapeanalysis)
81-hoursessions
TestofPlayfulnessChildrenexhibitedallelementsofplayfulness(intrinsicmotivation,
internalcontrol,suspensionofrealityandframing)whileplaying
theVRgames.
Playfulnessvariedwiththetypeofvirtualenvironment,somebeing
moreengagingthanothers.Descriptive&qualitativeanalysis.
[26]Cerebralpalsy;n¼16;
8–12years
Observationalstudy
(videotapeanalysis)
1hour/week,8weeks
PediatricVolitionalQuestionnaire
(measuresmotivation,levelof
engagement)
VRplayisamotivatingactivity,thereforeofinterestasaninterven-
tiontool.
Levelofvolitionwasinfluencedbythetypeofvirtualenvironment
(e.g.degreeofvariationinthegame,degreeofchallenge,
competition).Descriptive&qualitativeanalysis.
[23]Hemiplegia;n¼1;8yearsCasestudy;
60min/day,5Â/week
for4weeks
fMRI,BOTMP,modifiedPediatric
MotorActivityLogQuestionnaire,
UpperLimbsub-testofthe
Fugl-Meyerassessment
Improvedfunctionalmotorskills(use)andbetterqualityofmove-
ment(control,coordination)inaffectedupperlimb.
Post-intervention,spontaneousreaching,self-feedinganddressing
werenoted(notpossiblepriortoVR).
Concurrently,therewasgreateractivationofthecontralateral
sensorimotorcortex(asopposedtoipsilateralorbilateral).
Descriptivestatistics.
[9]Cerebralpalsy;n¼31;
8–12years;
19experimental,12control
(standardcare)
Randomizedcontrolled
trial;1.5hours/week,
8weeks
CanadianOccupationalPerformance
Measure(COPM),QualityofUpper
ExtremitySkillsTest(QUEST),
HarterSelf-PerceptionProfilefor
Children(SPPC)
Significantlyincreasedscoresforthesocialacceptancesub-scale
favouringtheexperimentalgroup.
VRappearstoincreasemotivationinexperimentalgroup.
Manychildreninthecontrolgroupwerelosttofollow-up.
Descriptive&comparativestatistics(t-test).
124 L. Snider et al.](https://image.slidesharecdn.com/virtualrealityasatherapeuticmodalityforchildrenwith-170619015915/75/slide-5-2048.jpg)
![[22]Cerebralpalsyandother;
n¼10withcerebral
palsy,n¼6without
cerebralpalsy
Observationalstudy;
One90minsession
Ankledorsiflexionexercises
alternatedbetweenVR
andconventionalexer-
cises(AB-BAdesignfor
intervention
administration)
VisualAnalogueScaleregardinginterest/
perceptionoffun(parentsand
children)
Movementkinematicsvia
electrogoniometer
Childrenandparentsreportedhigherlevelsoffunandinterest
withVR.
Morerepetitionscompletedwithconventionalexercises.
LongeraveragetimetocompleteonsetofVRexercise.
LongerholdtimesforVRexercises.
GreatermeanankledorsiflexionanklerangeofmotioninVR
exercises.
VRexercisesgoal-oriented.Descriptiveanalysis&graphic
representation.
[12]Spasticcerebralpalsy;
n¼4;4–8years
Single-subjectdesign,AB
with2-4weekfollow-up;
2hours/week,4weeks
Reachingkinematics,FineMotor
DomainofPDMS-2(sub-tests:
grasping,visual-motorintegration)
3/4childrenshowedimprovementinsomeaspectsofqualityof
reachingwhichwaspartiallymaintained4weeksaftertreatment.
ScoresonthePDMS-2increased(1–11points)forallchildren;
scoresonthevisual-motorintegrationsub-testimprovedfor3/4
subjects.Descriptiveanalysis;Statisticalanalysisofsinglesubject
designs(Cstatistic).
[24]Spasticdiplegia;n¼1;
13years
Casereport;
11sessions60–90minutes
(twogroupsessions)
4weeks
Inadditiontoregular
therapies
QUEST,GMFM,TVPS-3,Posture
ScaleAnalysr,Retrospectivedata
fromchartreview
Visualperceptualprocessing:Improvementinalldomainssequential
memory.Gainsmaderangefrom4–70percentilechanges.
Posturalcontrol:greaterloadingonLE;decreasedposturalsway
by60%;moresymmetricaldistributionofmedial-lateralweight.
Functionalmobility:increasedby235ft.Descriptiveanalysis.
[21]Spasticcerebralpalsy;
n¼12;7–16years
Casereport;treatment
duration&intensitynot
specified
QuestionnairedevelopedIntuitivetouse.
ChildrenweremotivatedtotrainusingtheEyeToy.
Descriptiveanalysis.
Spasticcerebralpalsy;
n¼10;7–16years
Randomizedtrial;
30minutes2Â/week6
weeks
MelbourneAssessmentofUnilateral
UpperLimbFunction
Increaseinscorefor6/10subjects;2nochange,2loss.Highest%
changein2childrenfromexperimentalgroup(9%and13%).
Descriptiveanalysis.
ANOVA:AnalysisofVariance;BOTMP:Bruininsks-OseretskyTestofMotorProficiency;fMRI:functionalMagneticResonanceImaging;PDMS-2:PeabodyDevelopmentalMotorScales-2;
GMFM:GrossMotorFunctionalMeasure;TVPS-3:TestofVisualPerception-3;LE:LowerExtremity.
Virtual reality as a therapeutic modality 125](https://image.slidesharecdn.com/virtualrealityasatherapeuticmodalityforchildrenwith-170619015915/75/slide-6-2048.jpg)
![lower quality studies. Further research of higher
methodological rigour is required.
In children with CP, is VR therapy more effective than
no intervention, placebo intervention or an alternative
intervention for activity and participation outcomes?
One ‘good’ pilot RCT revealed no significant
differences in the Canadian Occupational
Performance Measure performance and satisfaction
scores [9]. One observational study of 13 children
with CP indicated the all the children exhibited the
elements of playfulness while engaged in VR games.
The degree of playfulness fluctuated with the type of
virtual environment that was provided [25]. A case
study reporting on this question revealed that chil-
dren participated in self-feeding and dressing
post-intervention, activities that had not been pos-
sible or observed prior to VR therapy [23]. In
summary, there was a moderate level of evidence
(Level 1b) to suggest that VR therapy does not have
a positive impact on activity and participation
outcomes when compared to no intervention or
traditional therapy. Nevertheless, two other studies
of lower level of evidence indicate results to the
contrary. As the results generated by all the studies
with respect to this question are preliminary and
originate from small sample sizes, more research in
this area is warranted.
In children with CP, is VR therapy more effective than no
intervention, placebo intervention or an alternative
intervention for personal factor outcomes?
One ‘good’ pilot RCT revealed a significant increase
in scores for the social acceptance sub-scale of the
Harter Self-Perception Profile for Children in the
group receiving VR therapy. It was also found to
have a positive impact on the children’s motivation
[9]. Two observational studies reported on higher
levels of enjoyment and interest in participants
following VR therapy [22]. The type of VE that the
children are exposed to influenced their level of
volition [26]. Two case studies have reported higher
performance and satisfaction scores [10] as well as
greater levels of motivation to train with VE [21].
In summary, there is a moderate level (1b) of evi-
dence to suggest that VR therapy has a positive effect
on personal factors such as motivation, volition and
perceptions of self-efficacy as compared to no inter-
vention or alternative treatment methods. The
results of the RCT are supported by the outcomes
measured from several lower quality studies.
Discussion
VR therapy still remains a relatively new intervention
modality and the preliminary research in this
area is just emerging (publications since 2002).
Considering the novelty of this therapeutic modality,
the current evidence stems primarily from observa-
tional studies and case reports. Consequently, this
structured review included all types of research
design. Early evidence suggests that VR therapy
can be an effective and motivating therapeutic
modality for children with CP. In fact, of the nine
studies included in this review examining brain
reorganization, motor skills or visual-spatial out-
comes, seven indicated positive results in this area.
Of the three studies reporting on activity and
participation, two lower level studies indicated ben-
eficial effects in this domain. Finally, five studies
investigating the impact of VR on personal factors
were unanimous in determining that VR therapy had
a positive impact.
The potential uses of VR are vast, yet validation
of findings is necessary as the current body of
research is dominated by lower quality of evidence.
Table III. Summary of excluded articles.
Author(s) Title
Goodgold-Edwards SA, Gianutsos JG (1990) [29] Coincidence anticipation performance of children with spastic cerebral palsy and
non-handicapped children
Wann JP, Turnbull JD (1993) [30] Motor skill learning in cerebral palsy: movement, action and computer-enhanced
therapy
Hasdai A, Jessel AS, Weiss PL (1997) [31] Use of a computer simulator for training children with disabilities in the operation
of a powered wheelchair
Reid D (2002) [32] Virtual reality and the person-environment experience
Patel R, Salata A (2006) [33] Using computer games to mediate caregiver–child communication for children
with severe dysarthria
Chau T, Eaton C, Lamon A, Schwellnus H, Tam C (2006)
[34]
Augmented environments for paediatric rehabilitation
Koenig A, Bru¨tsch K, Zimmerli L, Guidali M, Duschau-
Wicke A, Wellner M, Meyer-Heim A, Lu¨nenburger L,
Koeneke S, Ja¨ncke L, et al. (2008) [35]
Virtual environments increase participation of children with cerebral palsy in
robot-aided treadmill training
Koenig A, Wellner M, Ko¨neke S, Meyer-Heim A,
Lu¨nenburger L, Riener R (2008) [36]
Virtual gait training for children with cerebral palsy using the Lokomat gait
orthosis
126 L. Snider et al.](https://image.slidesharecdn.com/virtualrealityasatherapeuticmodalityforchildrenwith-170619015915/75/slide-7-2048.jpg)
![Several threats to internal validity can explain the
findings of improvements in outcome measures
(e.g. practice effect and lack of blinded evaluators).
Duration of treatment in the studies included in this
structured review varied greatly, as did the choice
of outcome measures. All studies included in this
review had small sample sizes, which limited the
extent to which results could be generalized.
Furthermore, in the experimental studies, discre-
pancies at baseline between the control and inter-
vention groups were not always considered, which
can impact on the outcomes assessed. The great
variability in the assessments used to measure the
outcomes makes it difficult to synthesize results.
Use of more responsive measures will improve the
detection of changes in outcomes [27]. The majority
of studies investigating VR therapy utilized high cost
systems that many clinical facilities do not have the
means to purchase [5]. Considering that VR therapy
is motivating and engaging, it can be hypothesized
that compliance to treatment would be high. This is
further supported by promising positive results from
albeit low quality studies investigating commercially
available systems [21, 24]. These results demon-
strate the need for further research on readily
available gaming systems and their benefits for this
population.
Although outcomes were not specifically categor-
ized by authors according to the dimensions of the
ICF, the majority of outcomes measured were
related to body structures and function as well as
activity and participation. Specifically, there were far
fewer studies related to activity and participation.
Further investigations should be initiated in this
domain, particularly as VR may be useful to promote
social participation through virtual environments as
the barriers that are present in natural environments
can be eliminated.
Conclusion
Currently, there is a paucity of well designed studies
investigating the benefits of VR therapy in the
rehabilitation of children with CP. Overall, the
level of evidence is poor, as most of the studies are
experimental and observational studies with small
sample sizes. The results of this systematic review
reveal that there is conflicting evidence (Level 4) that
VR therapy has positive effects on body structures
and functions, a moderate level of evidence (Level
1b) that VR does not positively impact on activity
and participation and a moderate level of evidence
(Level 1b) that VR therapy positively impacts on
personal factors such as motivation, volition and
interest.
With the Wii and other games gaining popularity in
rehabilitation settings across North America,
research regarding commercially available gaming
systems is an emerging interest in this field, as the
potential benefits of this treatment modality seem
promising [6, 7]. As children with CP are a hetero-
geneous group, it would be necessary to clarify the
sub-groups of the population that would most benefit
(age, gender, type of CP, motor abilities, cognitive
function, etc.) and what treatment outcomes should
be targeted. The long-term benefits of VR therapy
are still unknown. More high quality randomized
controlled trials on large samples with follow-up are
needed to ascertain for which children with CP and
for what outcomes this approach may be better
than traditional rehabilitation interventions.
Acknowledgements
This review was conducted as part of a presentation
on occupational therapy intervention for cerebral
palsy consensus meeting, September 2008, Oxford,
United Kingdom. The authors are members of the
Research Institute of the McGill University Health
Centre, which is supported in part by the Fonds de
recherche´ en sante´ du Que´bec. This study was
initially funded by an operating grant from the
Reseau provincial de recherche en adaptation-
re´adaptation.
Declaration of interest: The author reports no
conflict of interest. The author alone is solely
responsible for the content and writing of this paper.
References
1. Wilson PN, Foreman N, Stanton D. Virtual reality, disability
and rehabilitation. Disability & Rehabilitation 1997;19:
213–220.
2. Bax M. Terminology and classification of cerebral palsy.
Developmental Medicine & Child Neurology 1964;6:
295–296.
3. Yamamoto MS. Cerebral palsy. In: Hansen RA, Atchison B,
editors. Conditions in occupational therapy: Effect on occu-
pational performance. 2nd ed. Baltimore, MD: Lippincott
Williams & Wilkins; 2000. p 8–15.
4. Riley DM. Kids’ use of consumer electronics devices such as
cell phones, personal computers and video game platforms
continue to rise. Port Washington, NY: NPD Group, Inc.;
2009.
5. Reid D. Virtual reality and the person-environment experi-
ence. Cyberpsychology & Behavior 2002;5:559–564.
6. Associated Press. La Wii comme the´rapie. La Presse;
17 February 2008, Associated Press: Montreal, QC.
7. Kutlu N. La ‘Wii the´rapie’ fait son chemin au Que´bec.
La Presse; 17 February 2008: Montreal, QC.
8. Lupton D, Seymour W. Technology, selfhood and physical
disability. Social Science & Medicine 2000;50:1851–1862.
9. Reid D, Campbell K. The use of virtual reality with children
with cerebral palsy: A pilot randomized trial. Therapeutic
Recreation Journal 2006;40:255–268.
Virtual reality as a therapeutic modality 127](https://image.slidesharecdn.com/virtualrealityasatherapeuticmodalityforchildrenwith-170619015915/75/slide-8-2048.jpg)