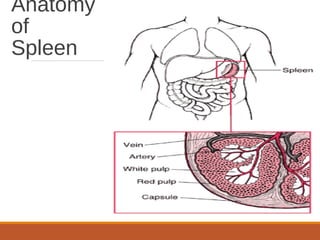
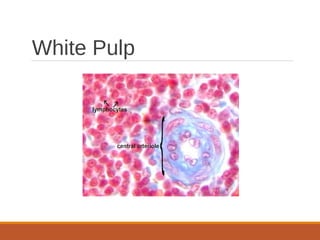
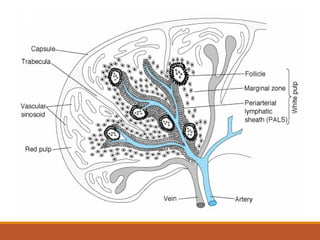
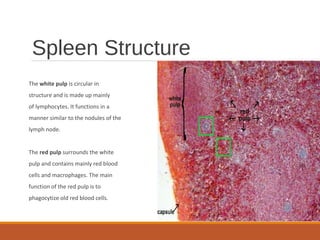
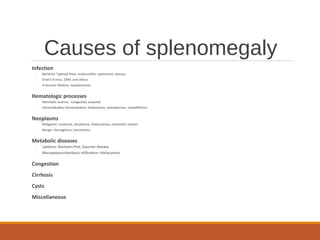
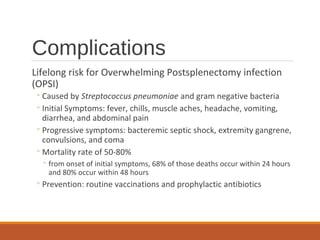
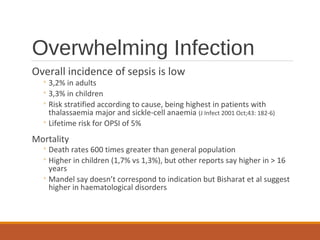
The spleen filters blood and mounts immune responses. It produces blood cells before birth but later filters out old red blood cells and mounts immune responses via white pulp and macrophages in red pulp. Congenital asplenia or splenectomy reduce immunity. Hyposplenism results in slower adaptive immunity and increased infection risk like overwhelming sepsis from pneumococcus. Diagnosis examines anatomy and function via imaging and blood smears. Complications include lifelong risk of sepsis.