This document discusses spinal tumors, including:
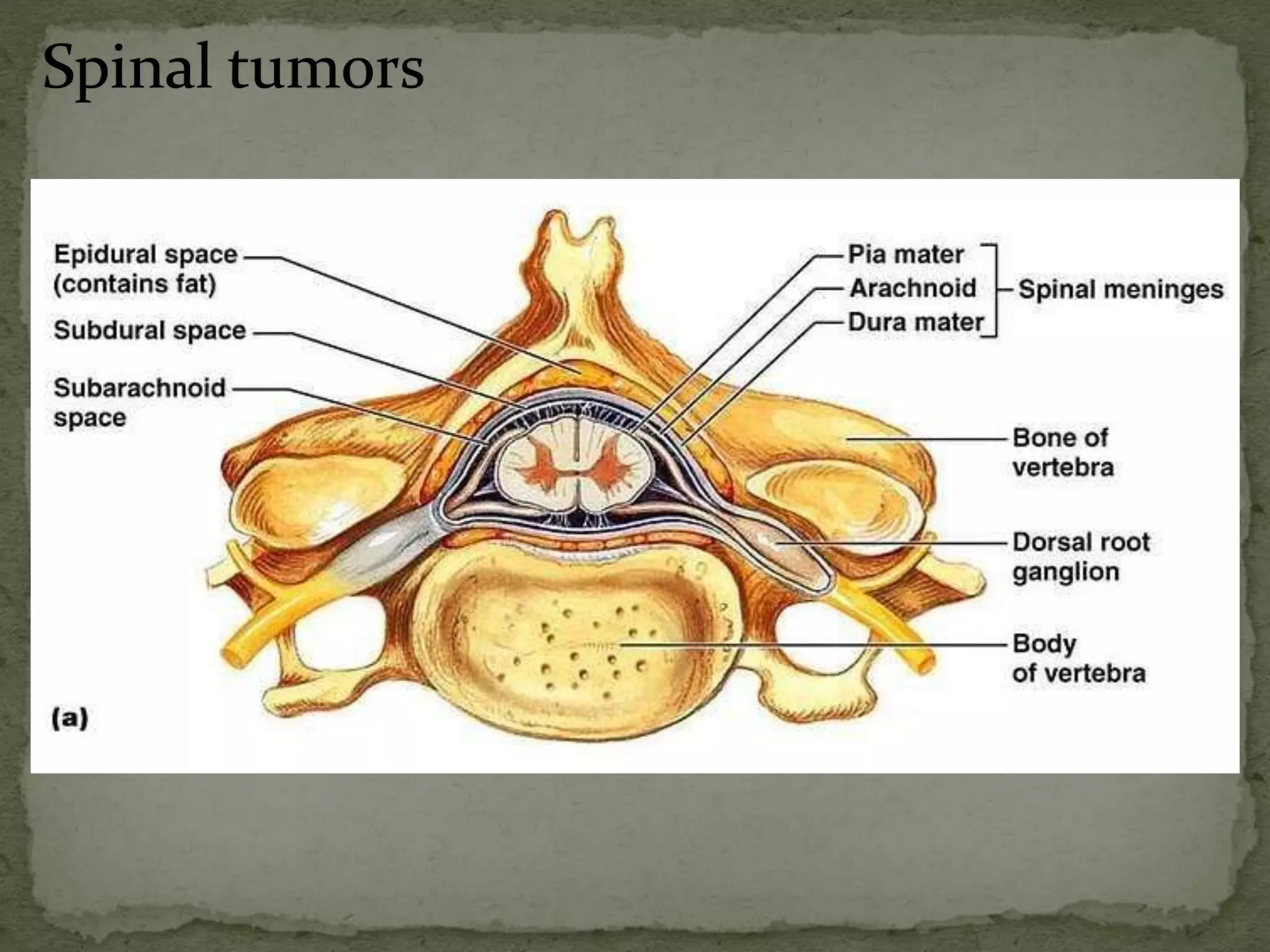
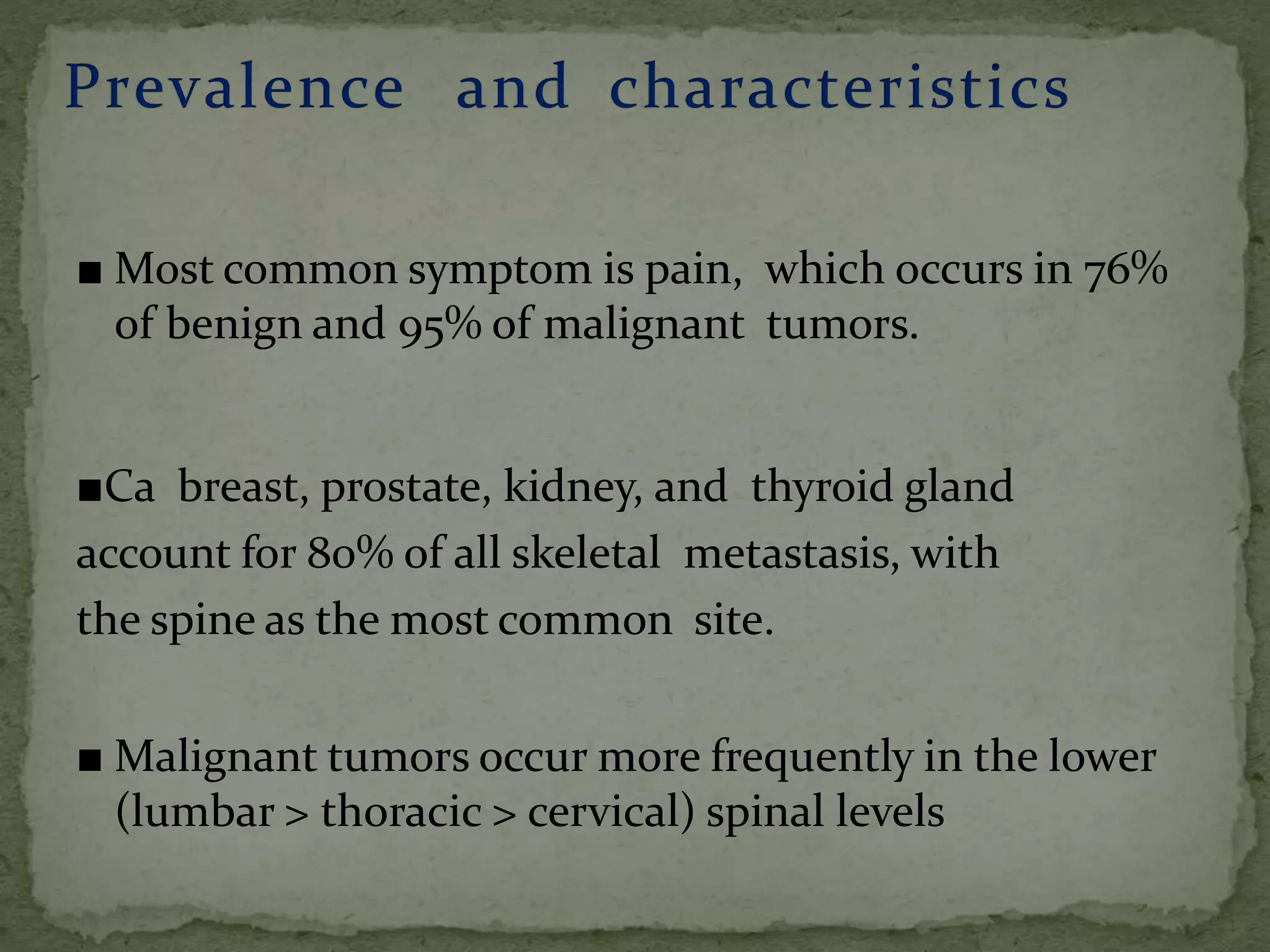
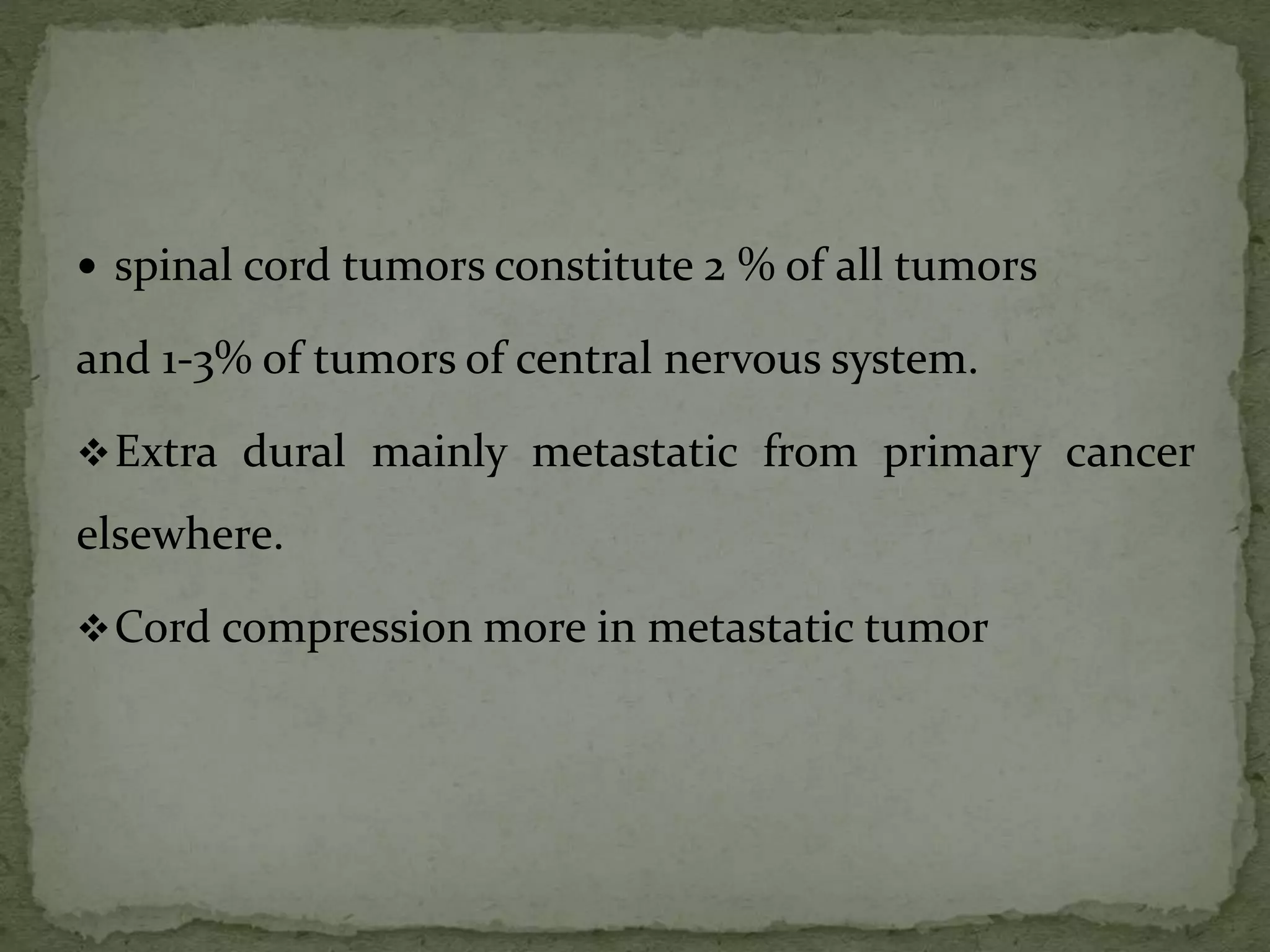
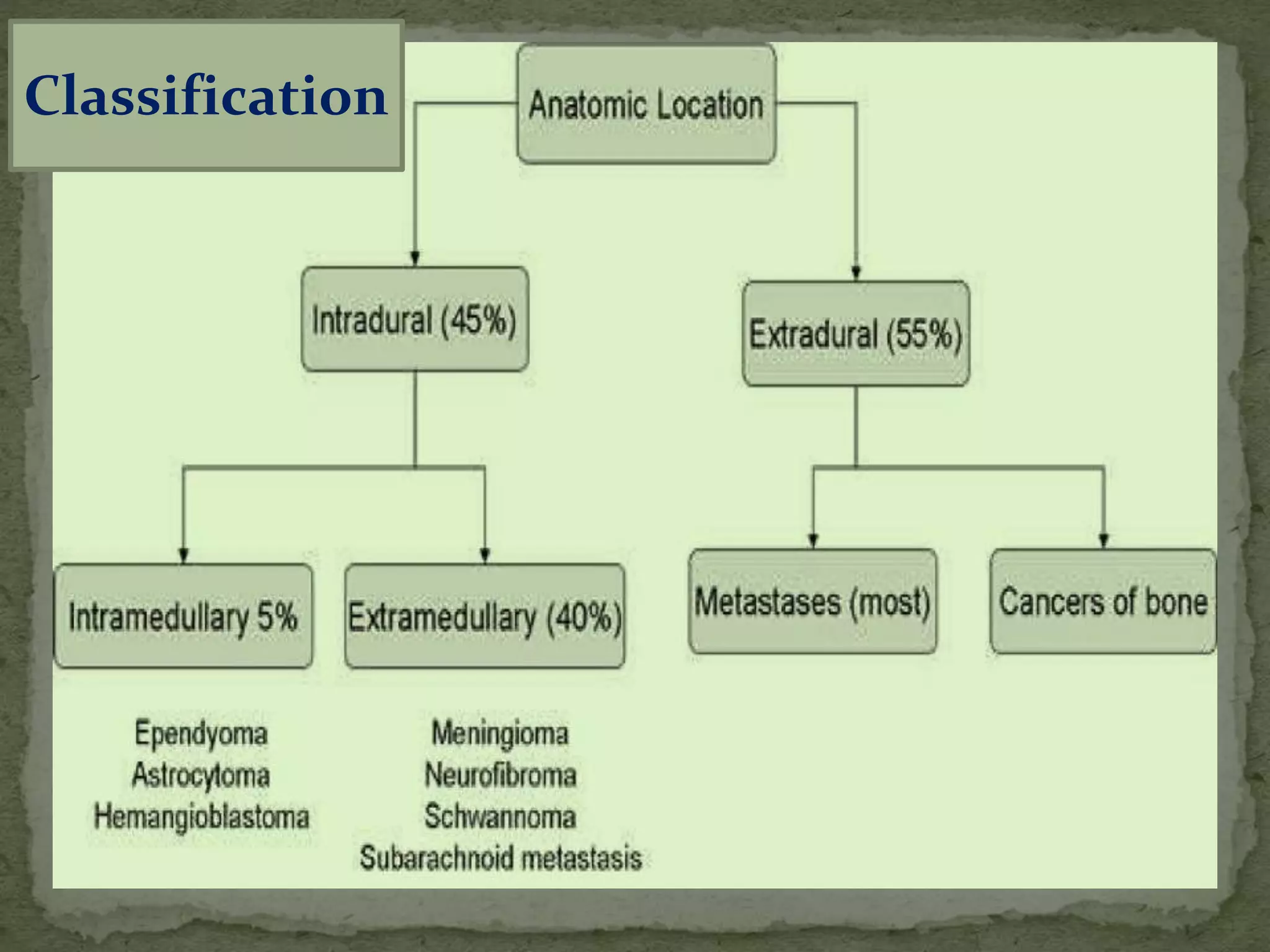
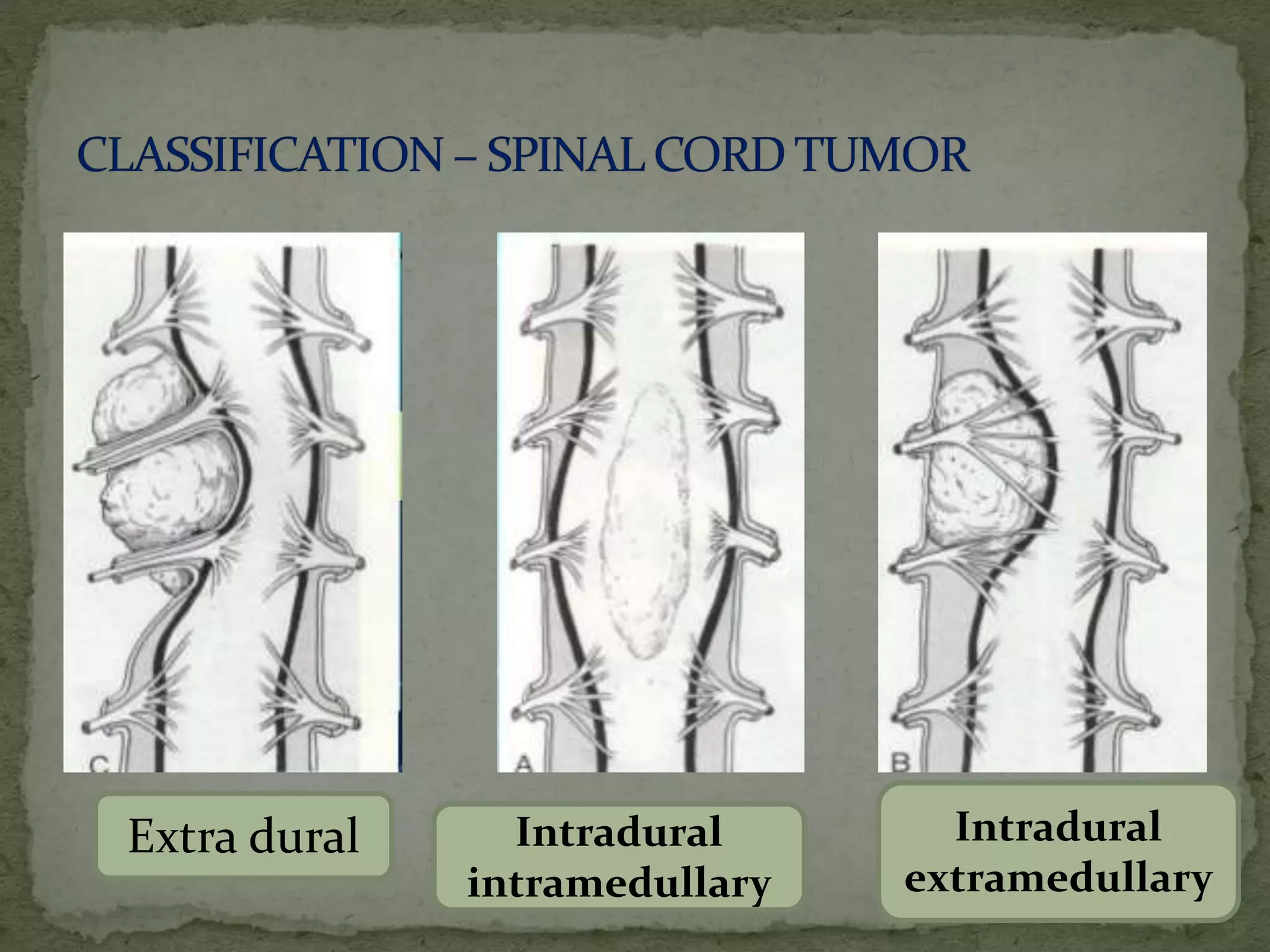
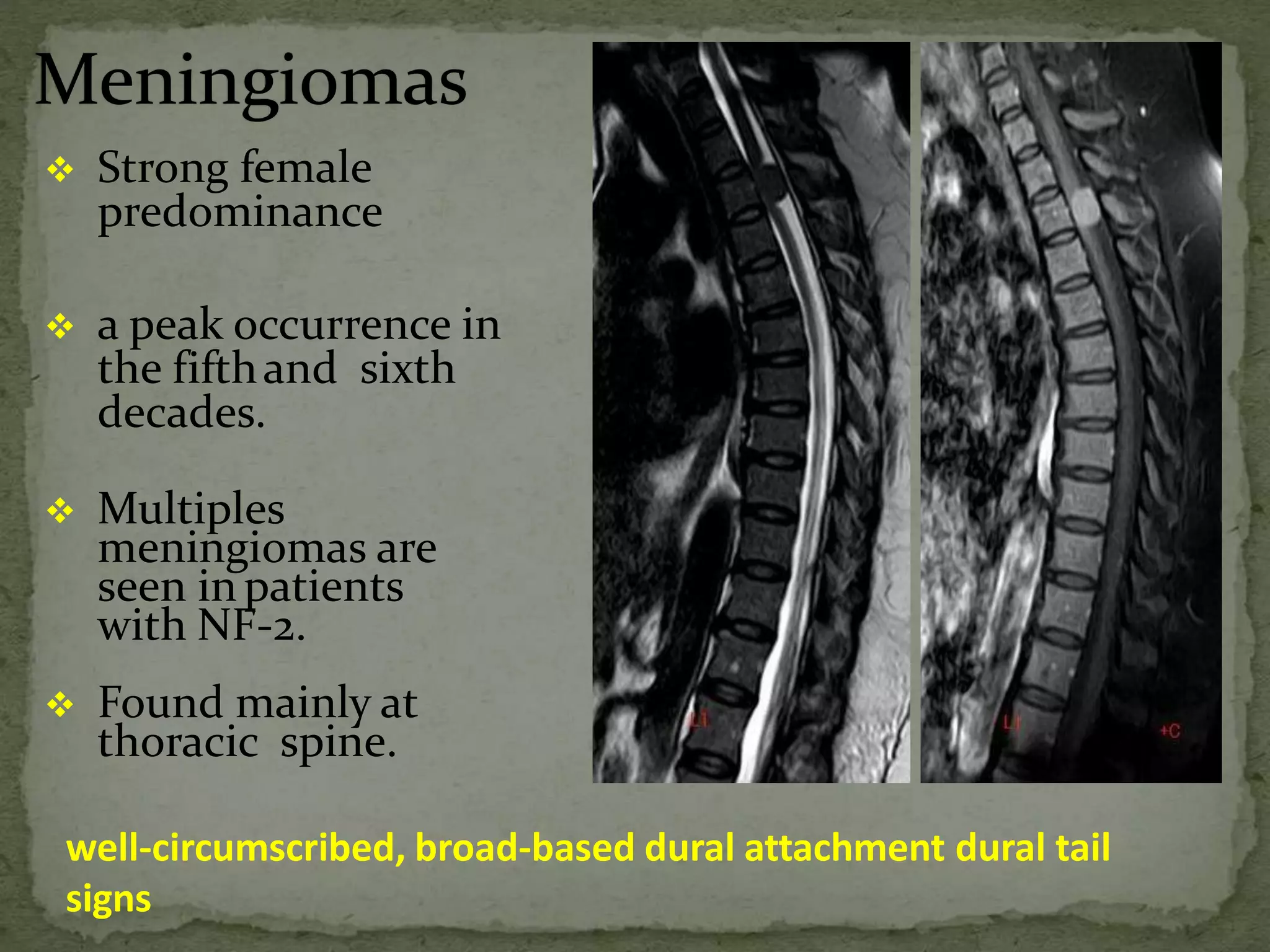
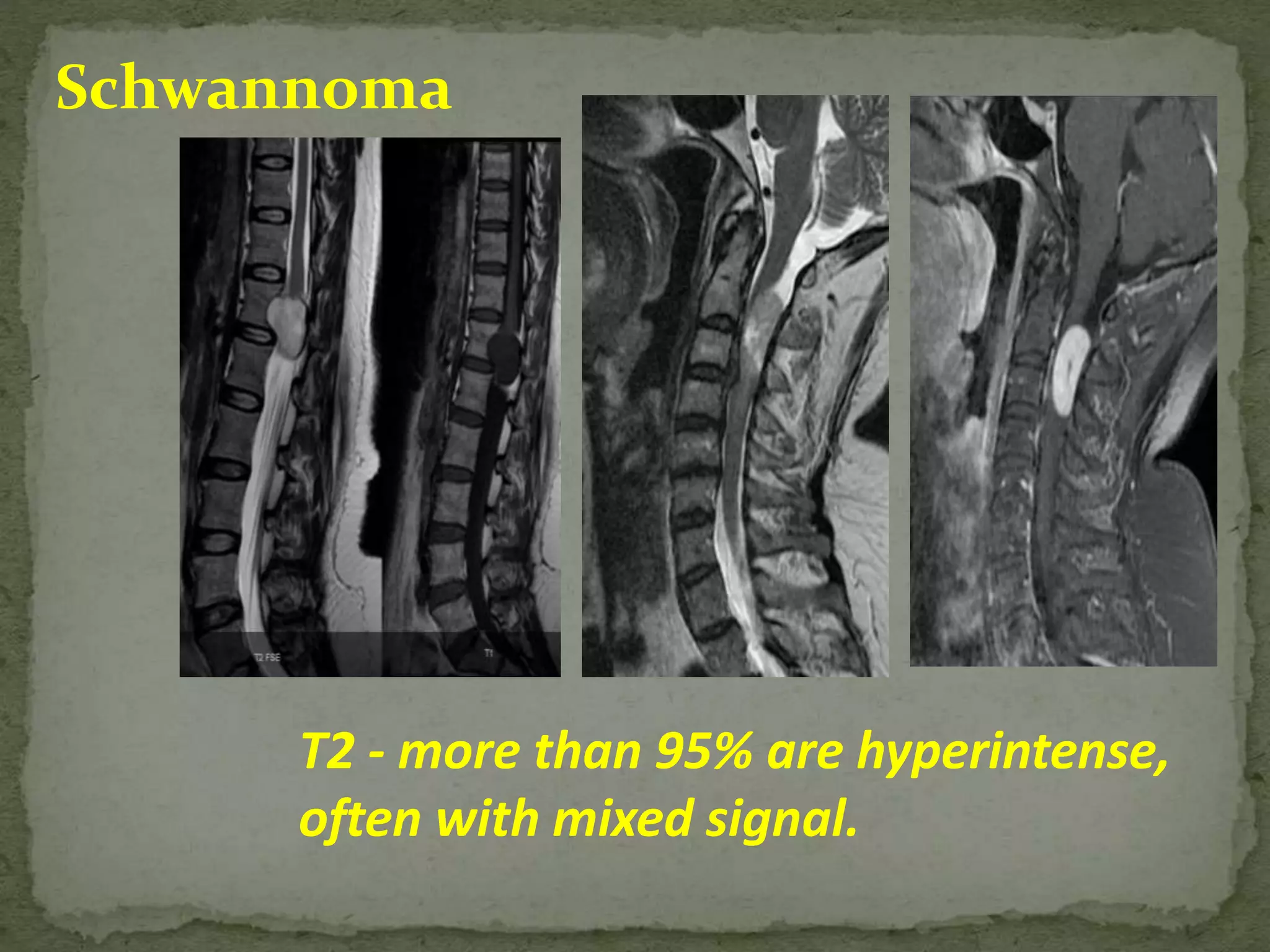
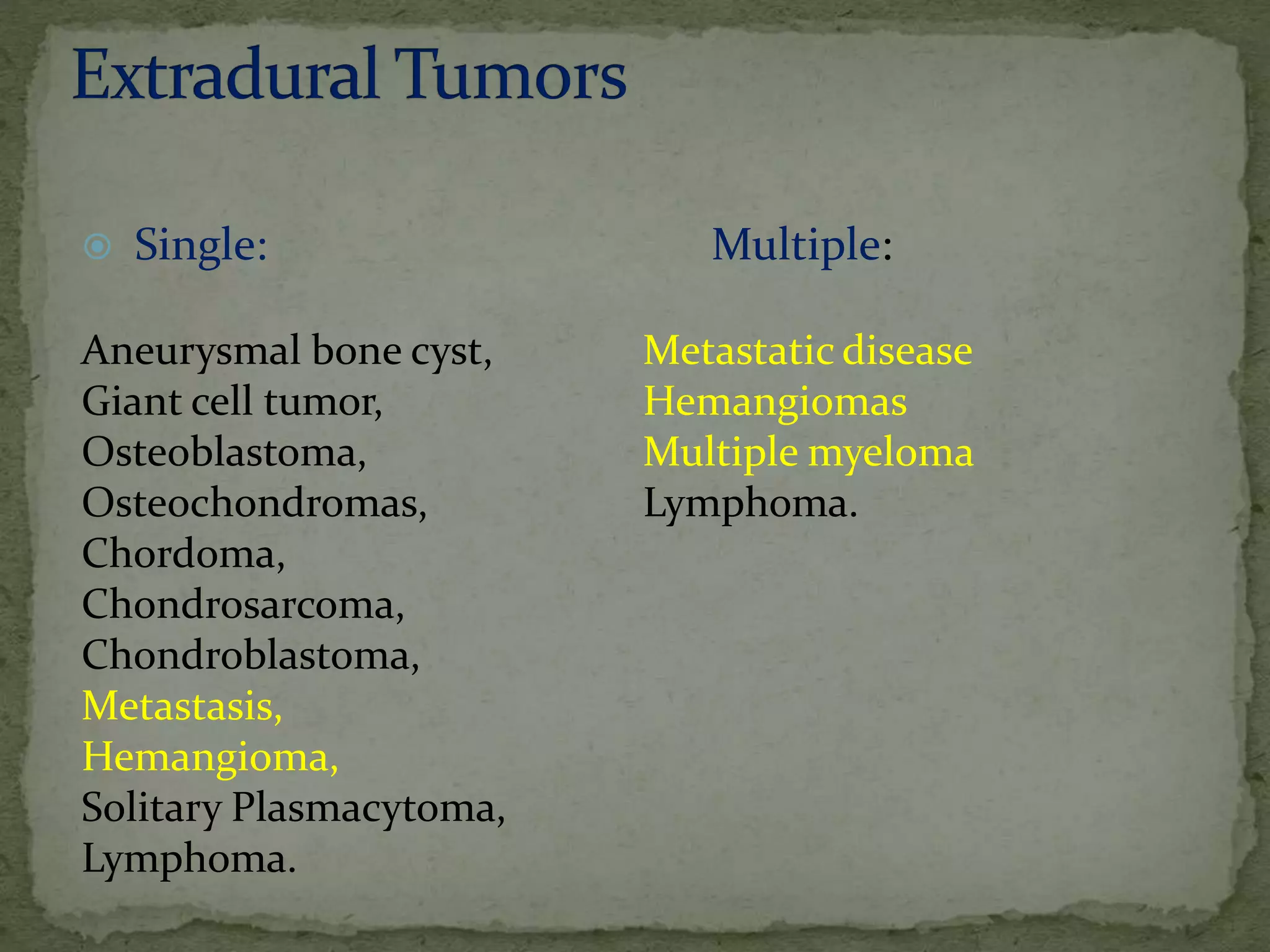
1. Spinal tumors can be primary or secondary, extradural or intradural. The most common symptoms are pain and neurological deficits.
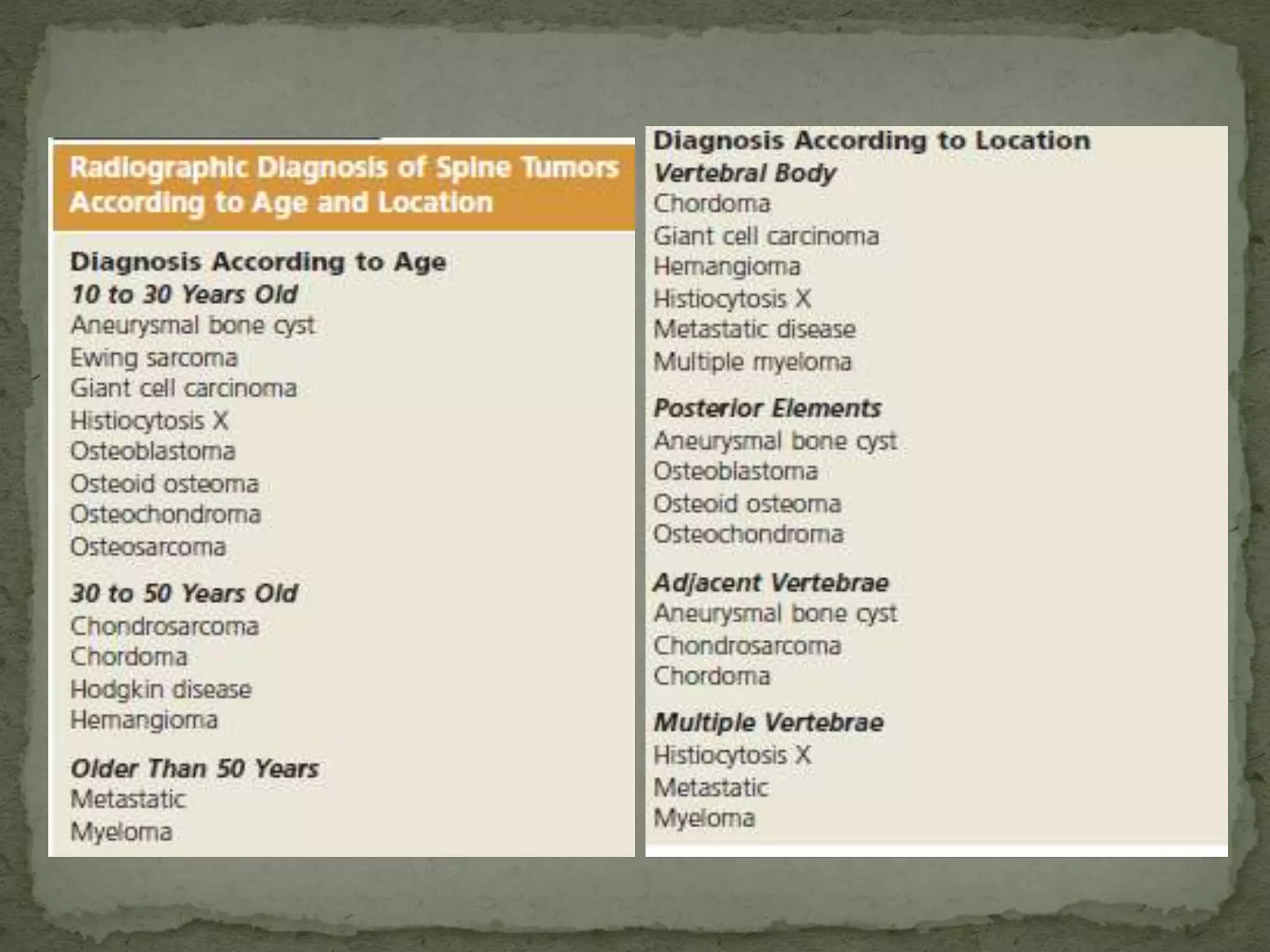
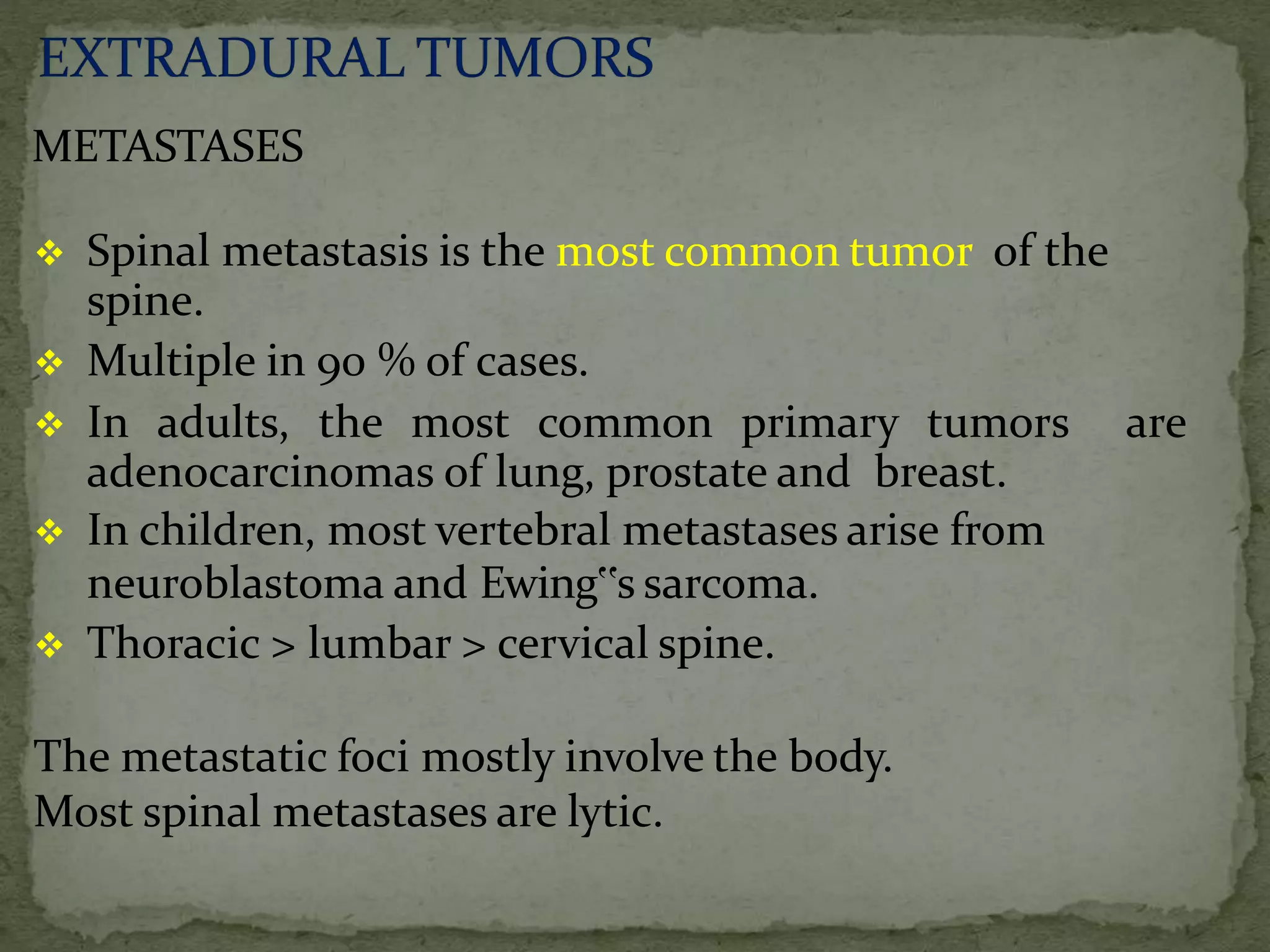
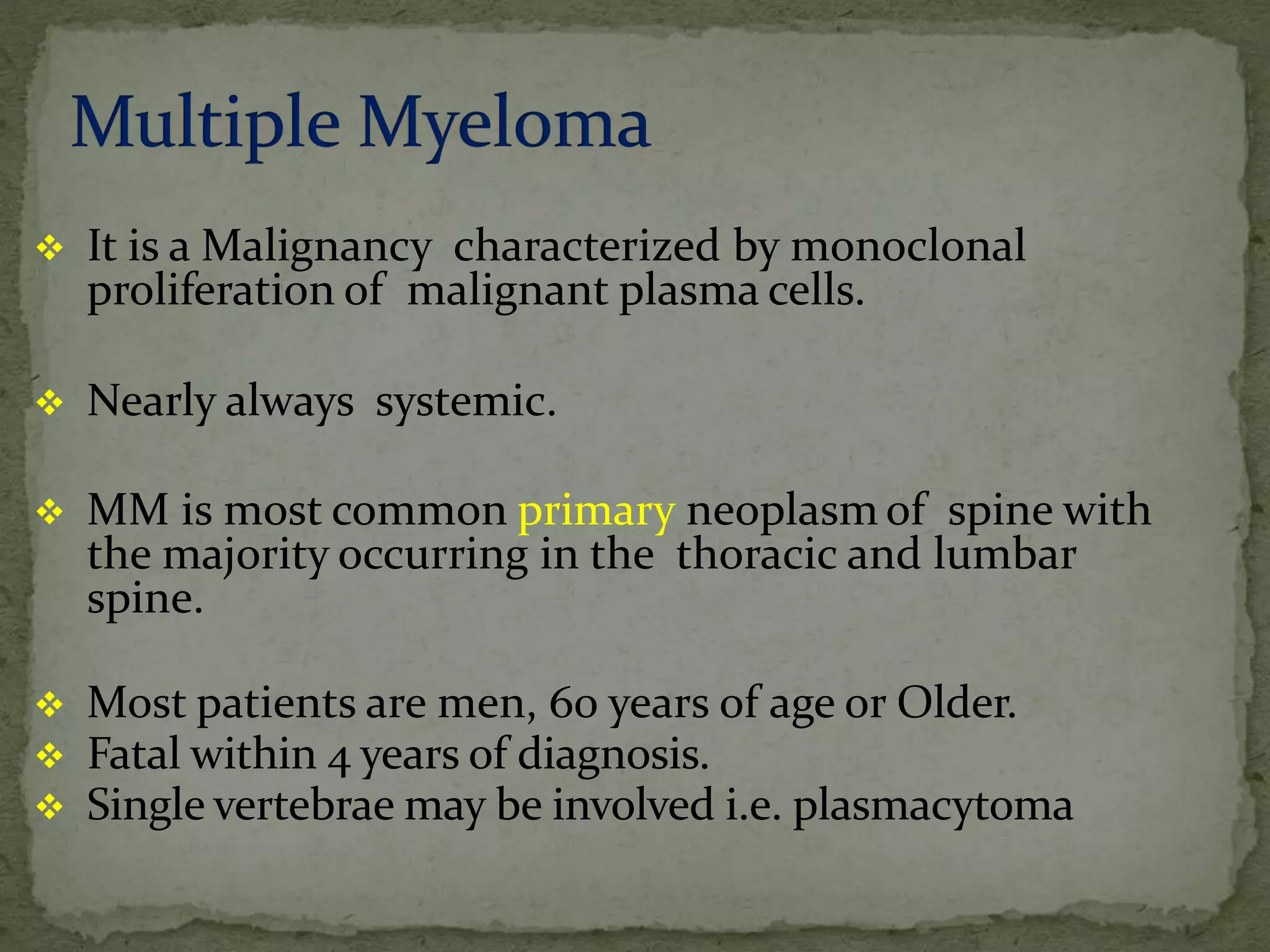
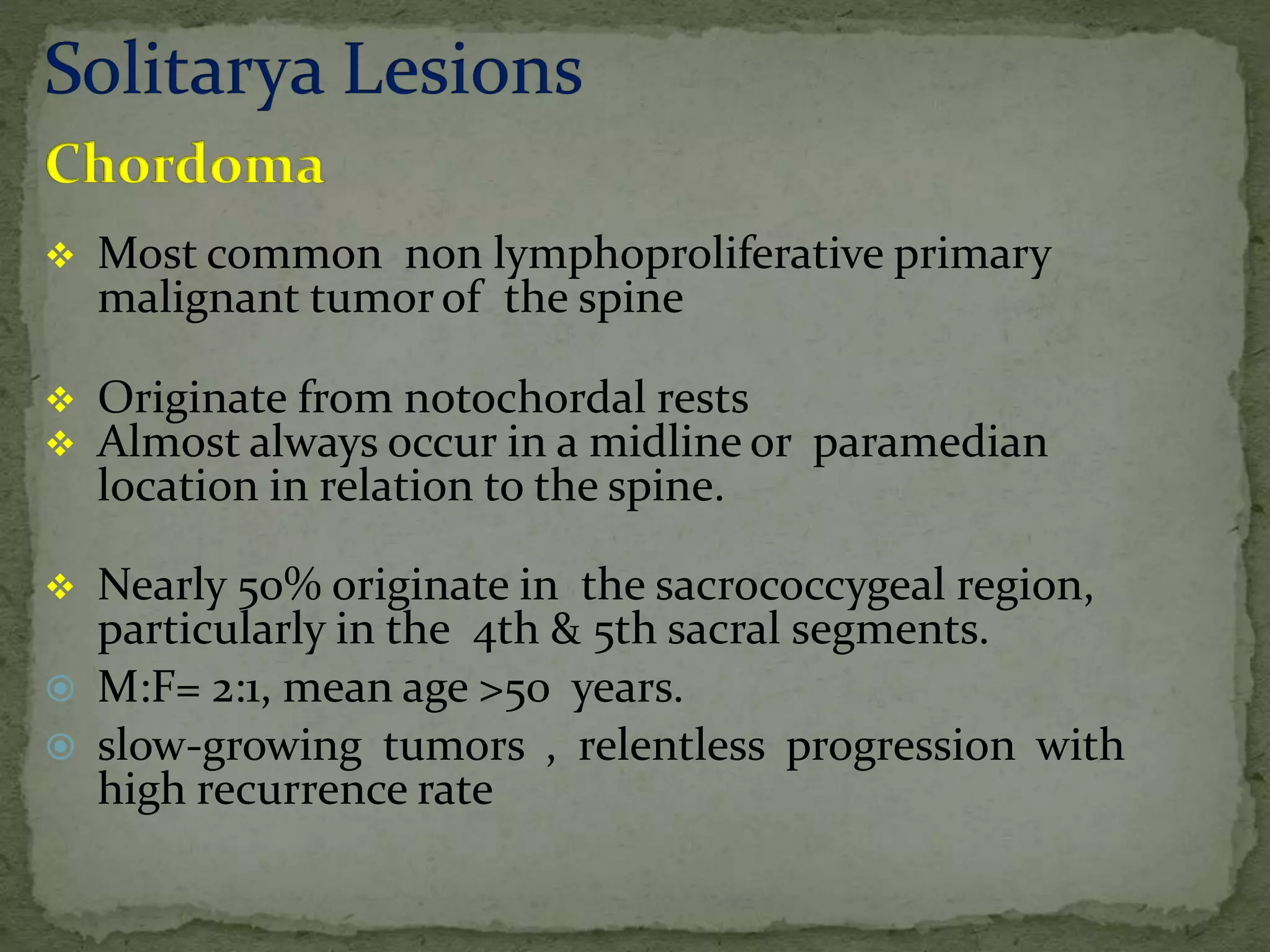
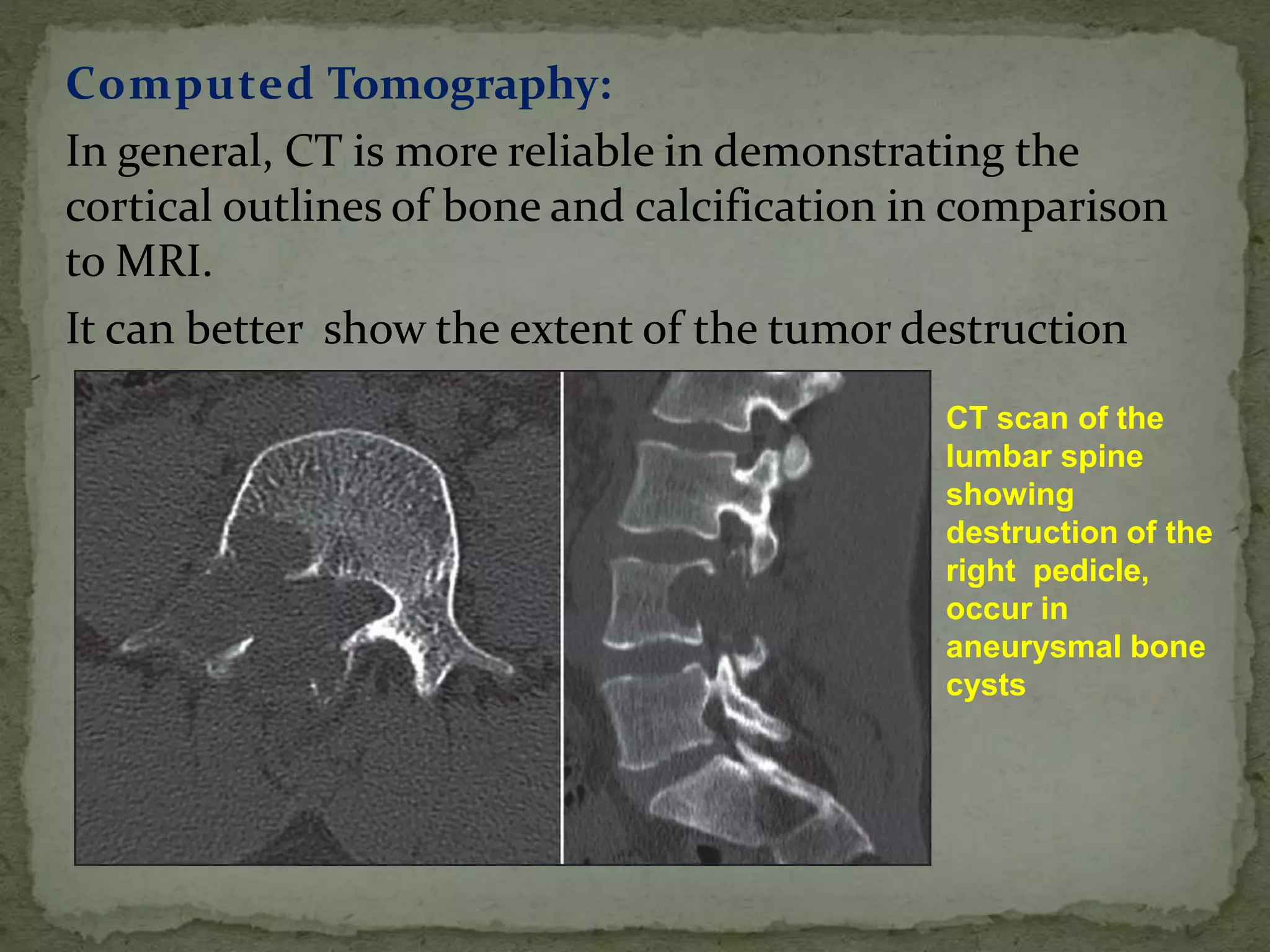
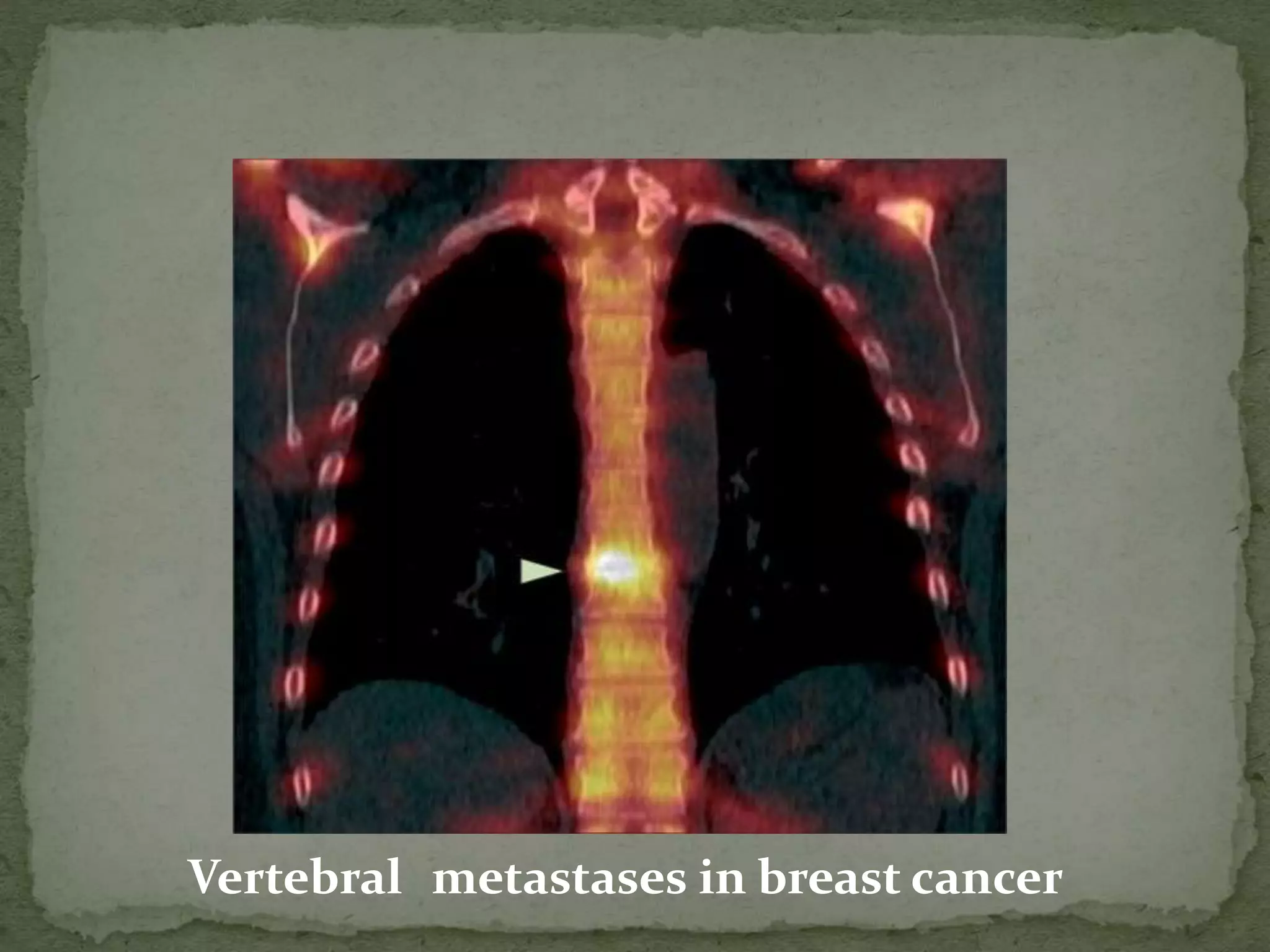
2. Common primary tumors include hemangiomas, aneurysmal bone cysts, and chordomas. Metastatic tumors are most frequently from breast, prostate and lung cancers.
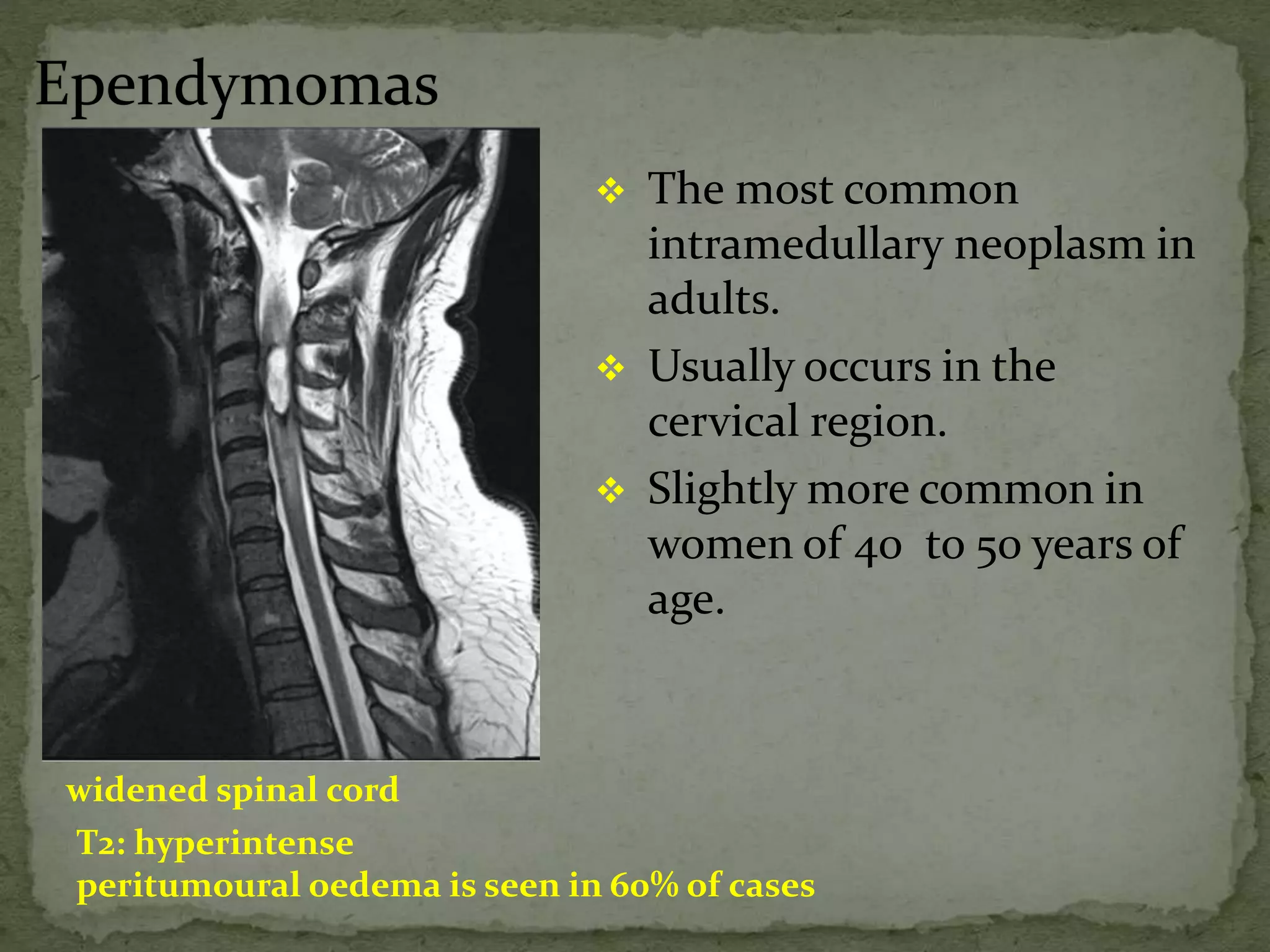
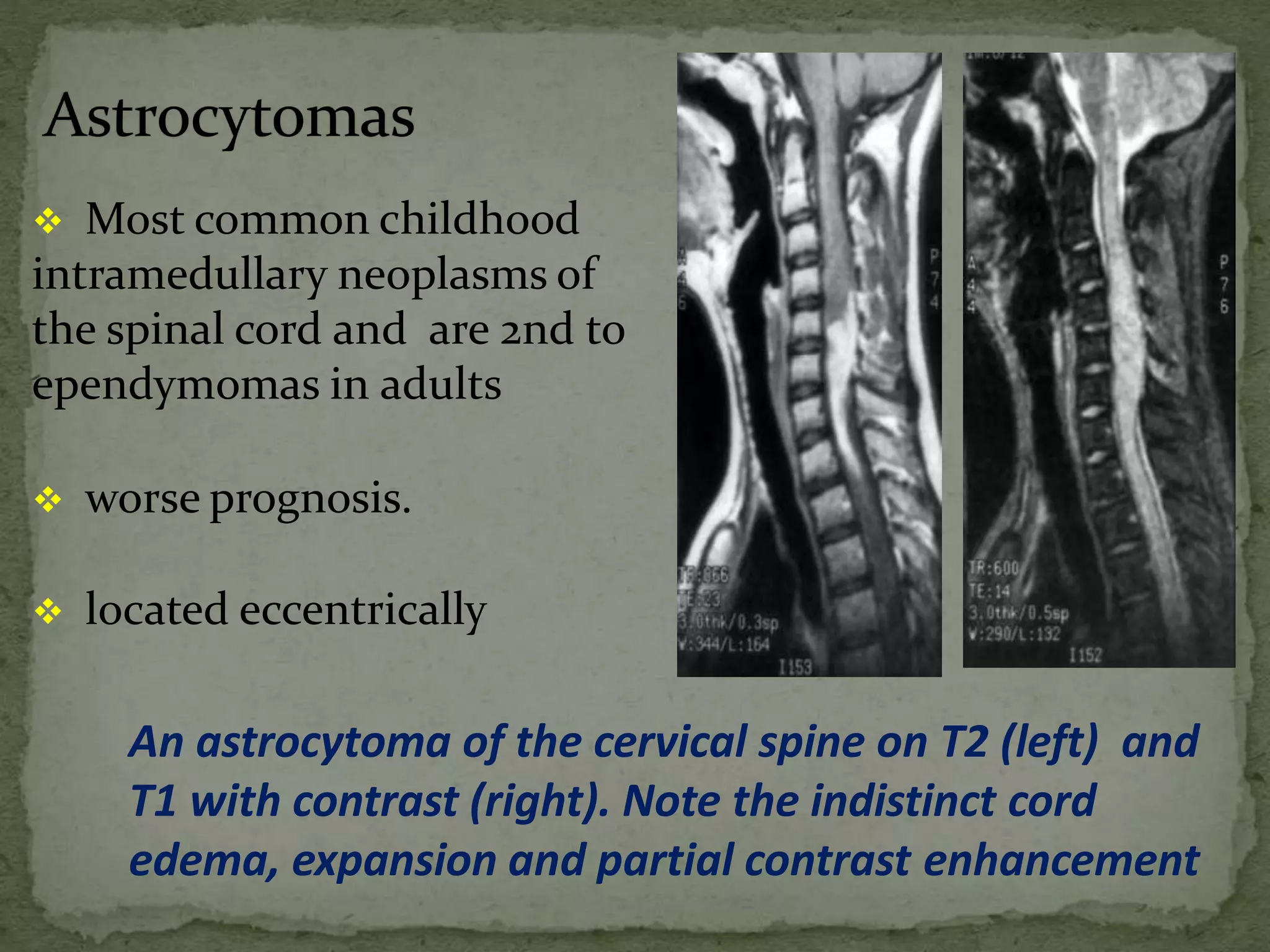
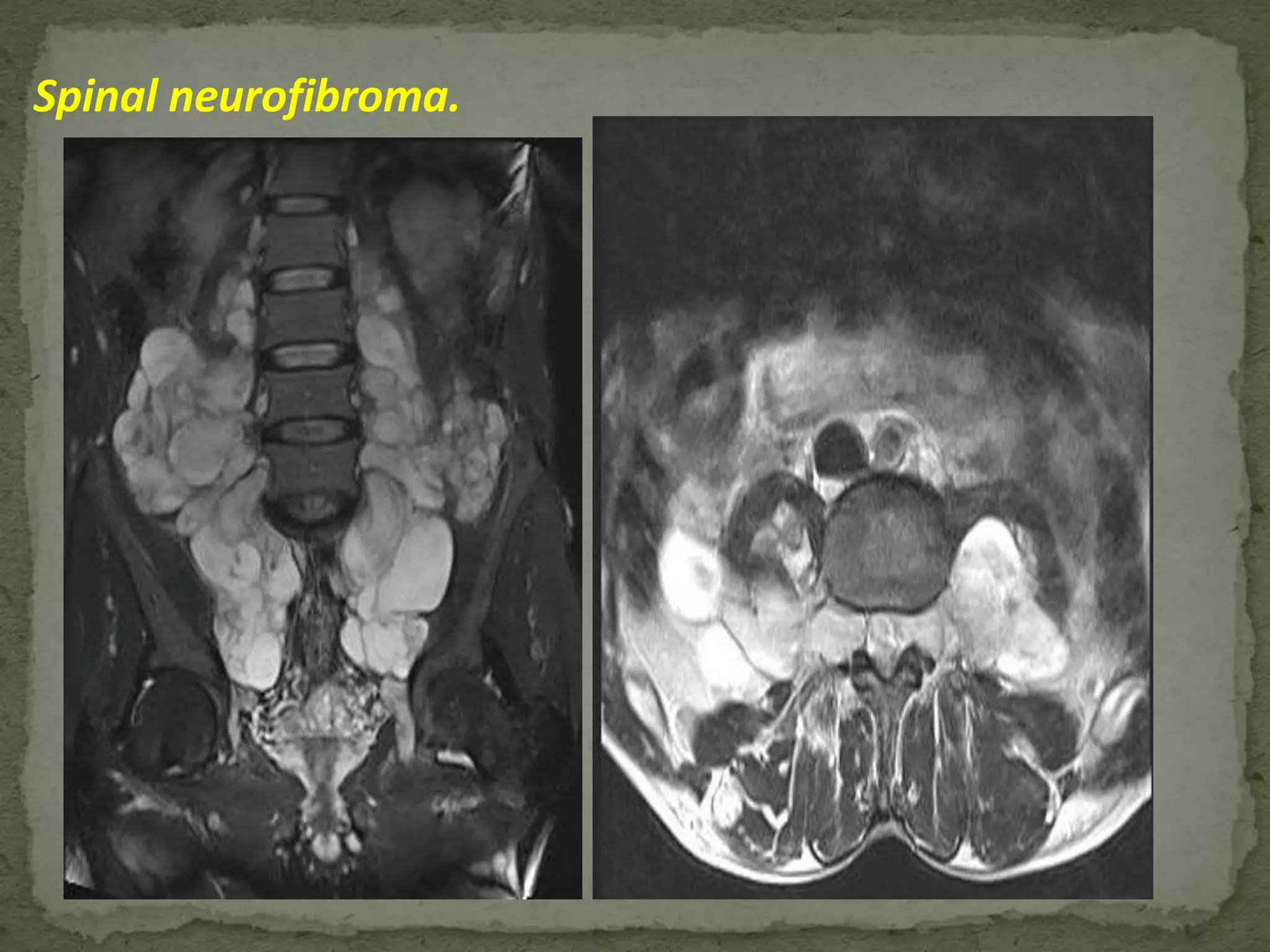
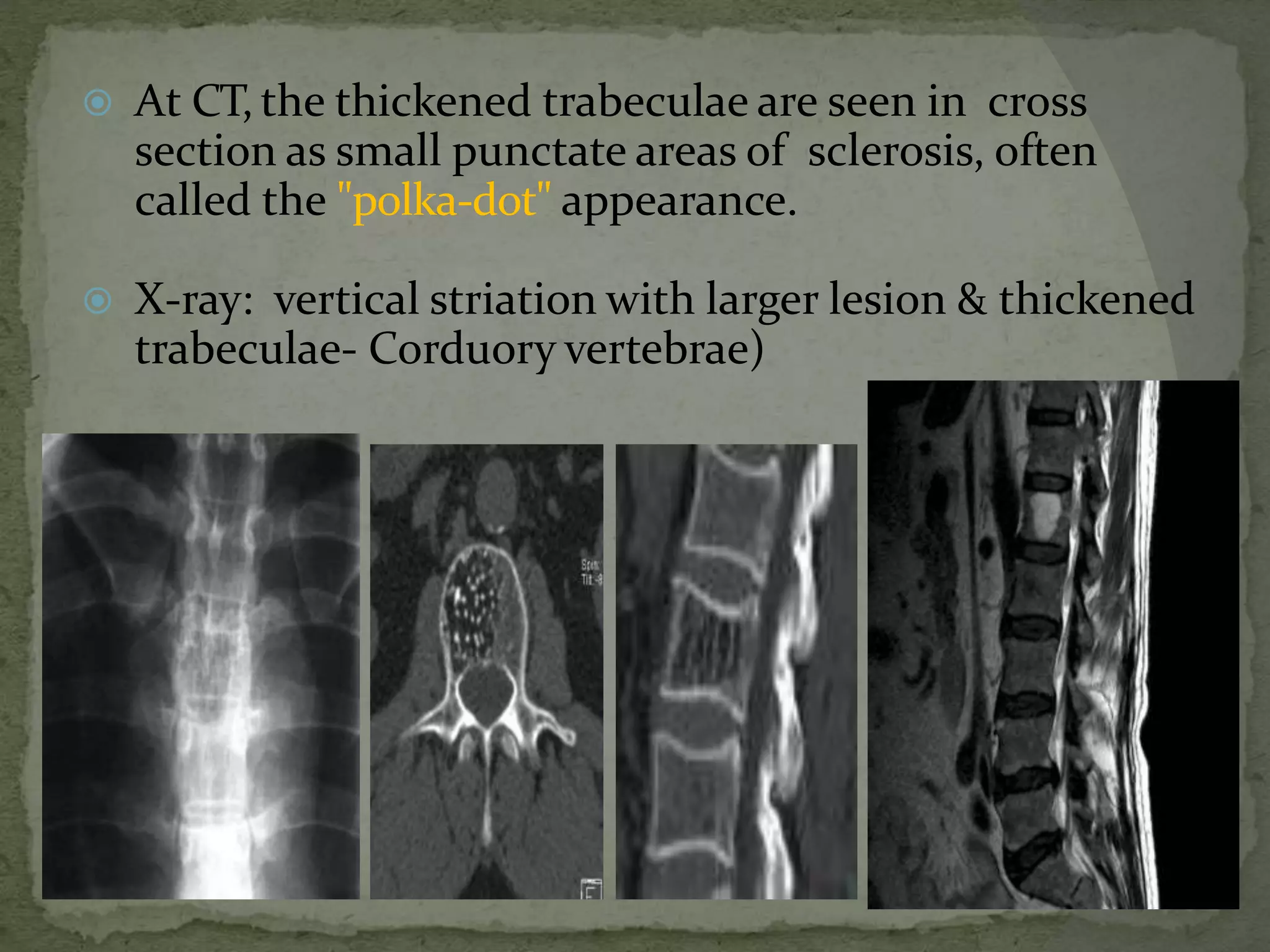
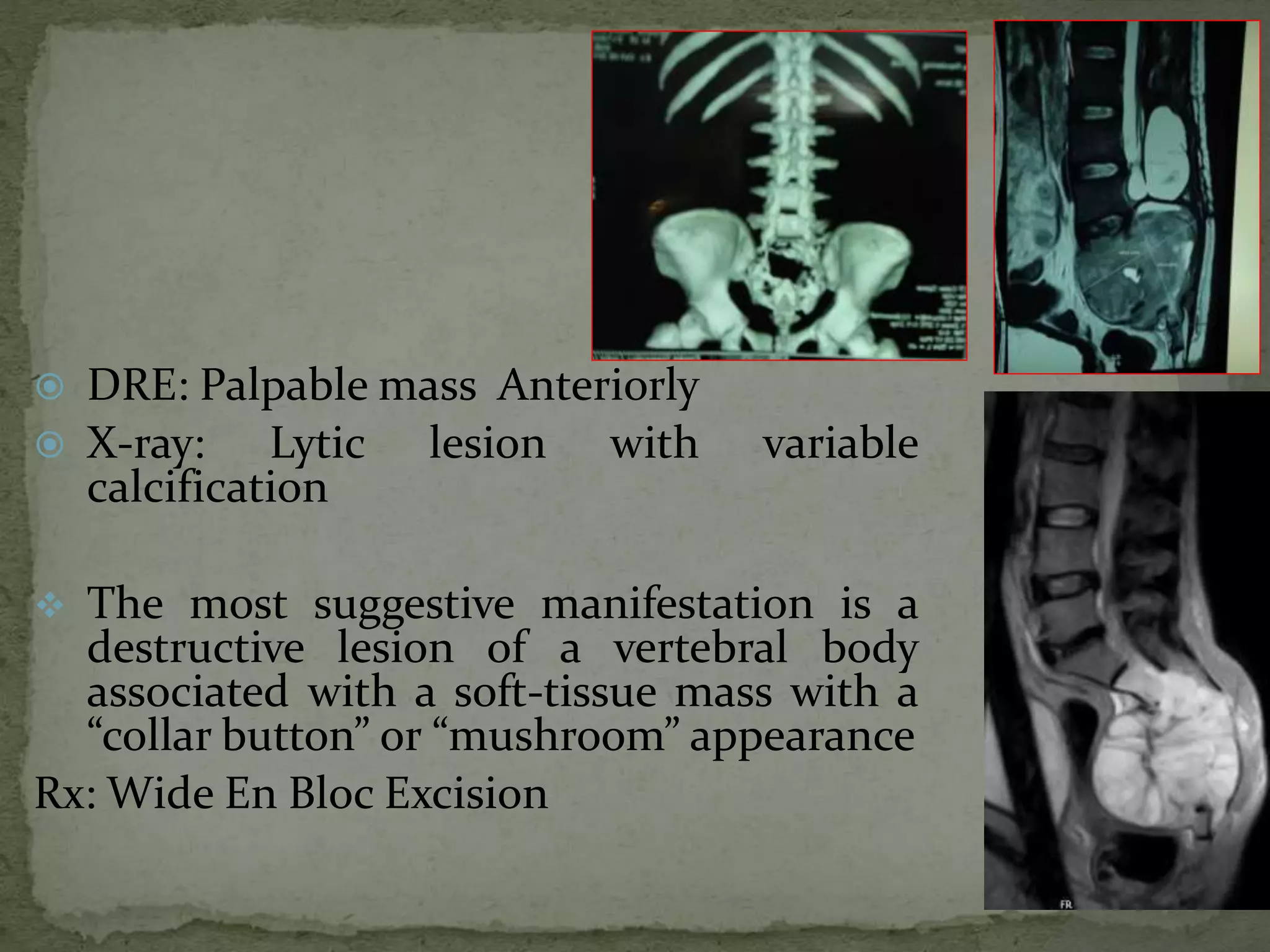
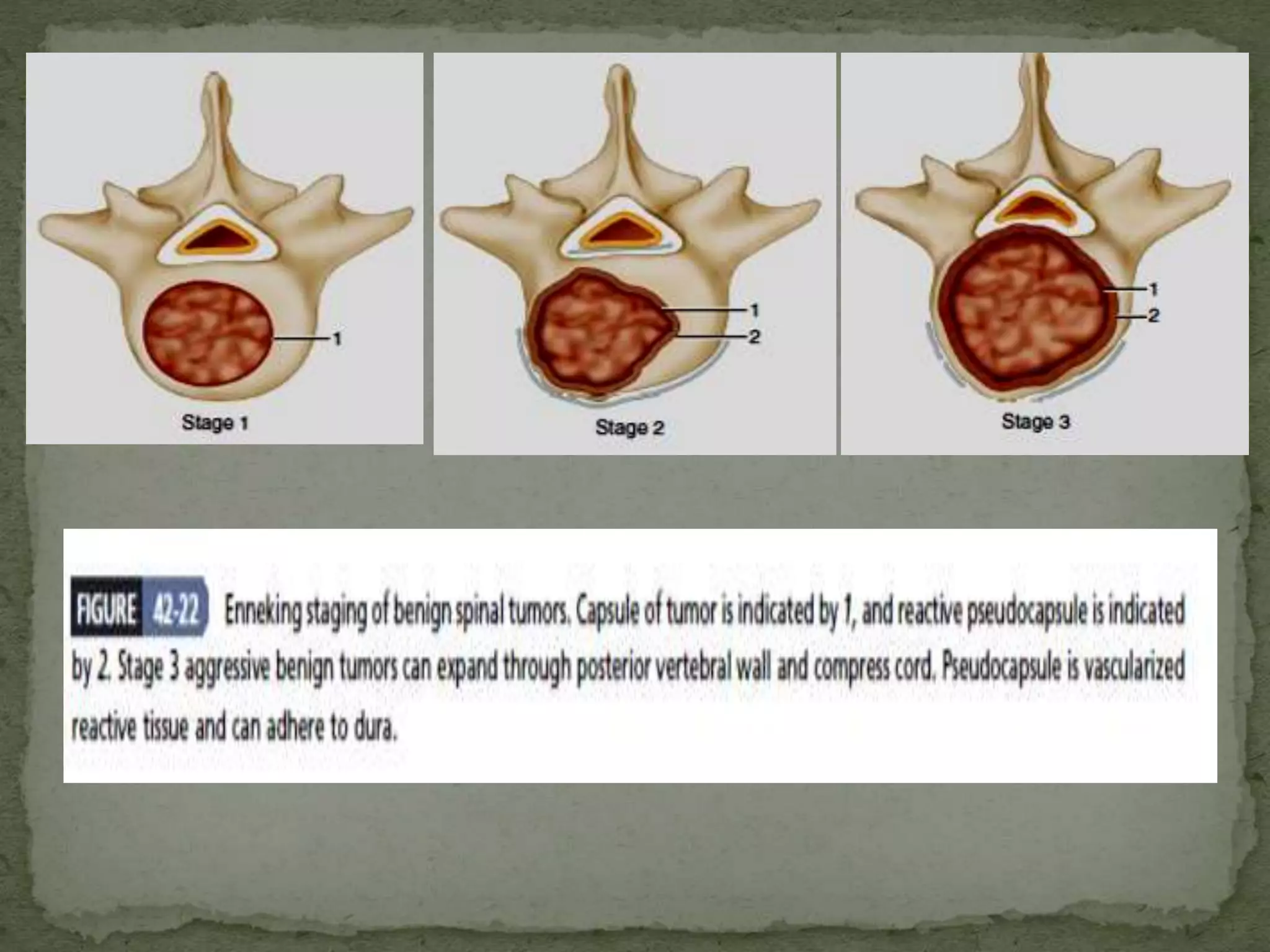
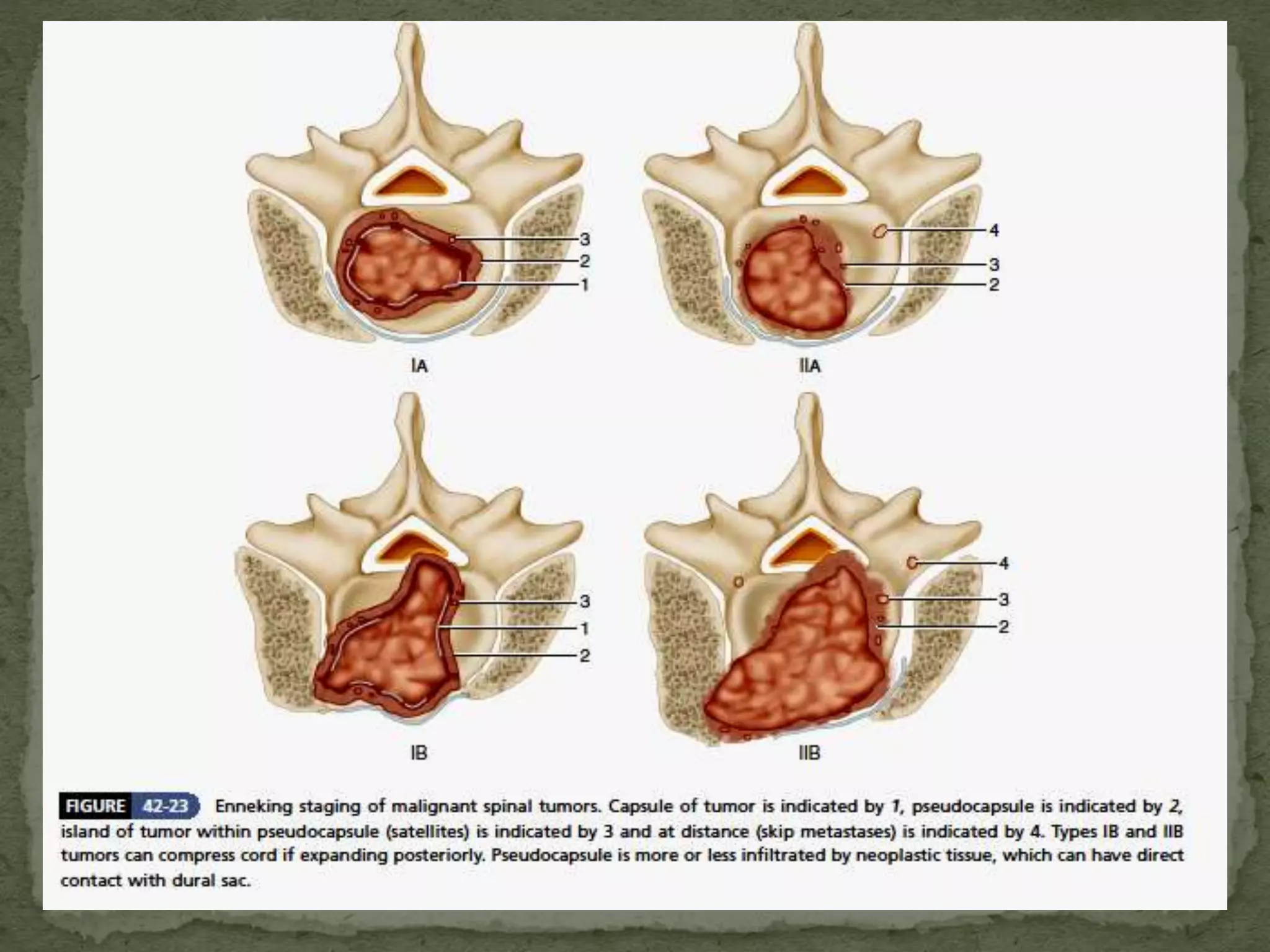
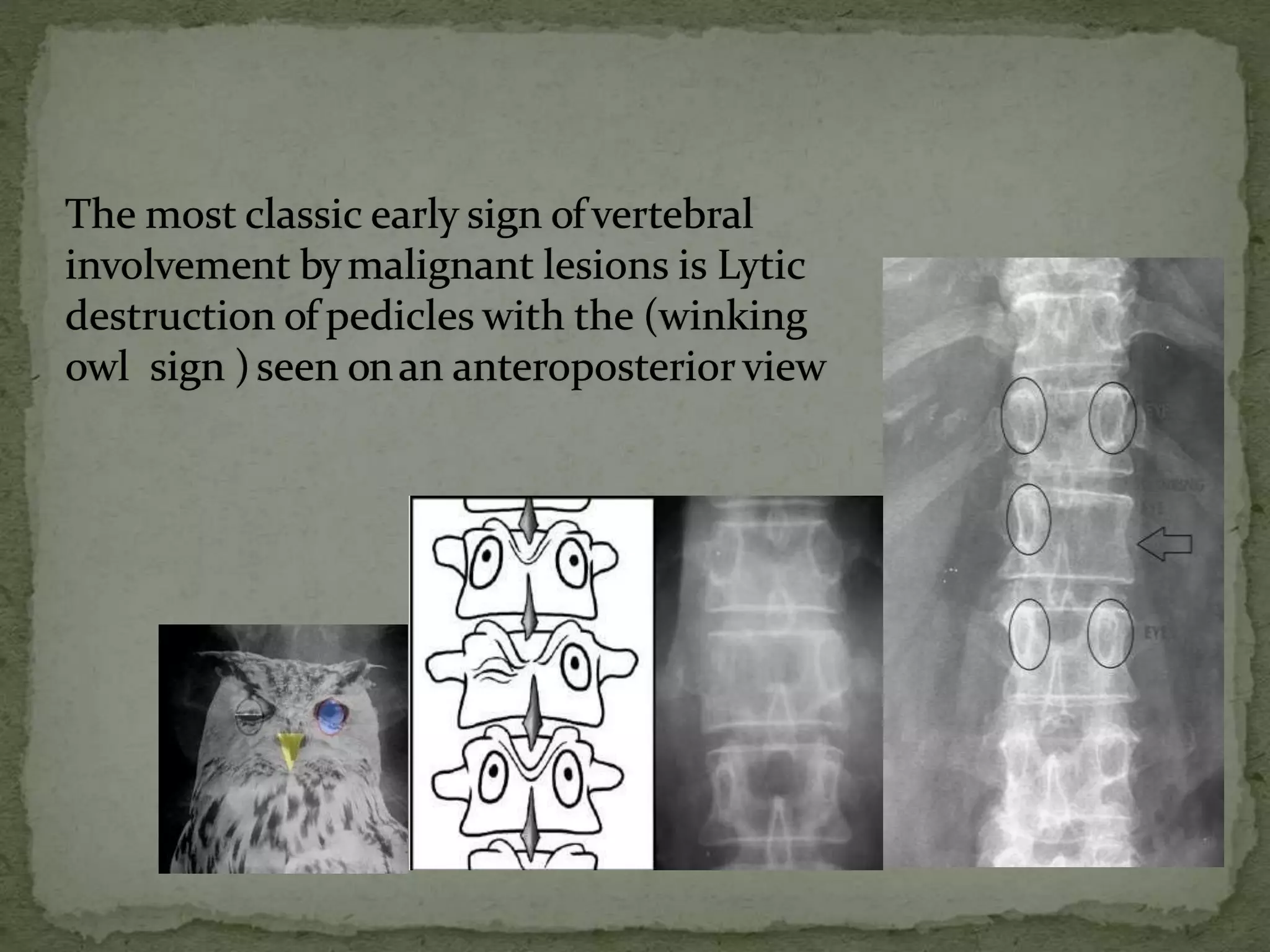
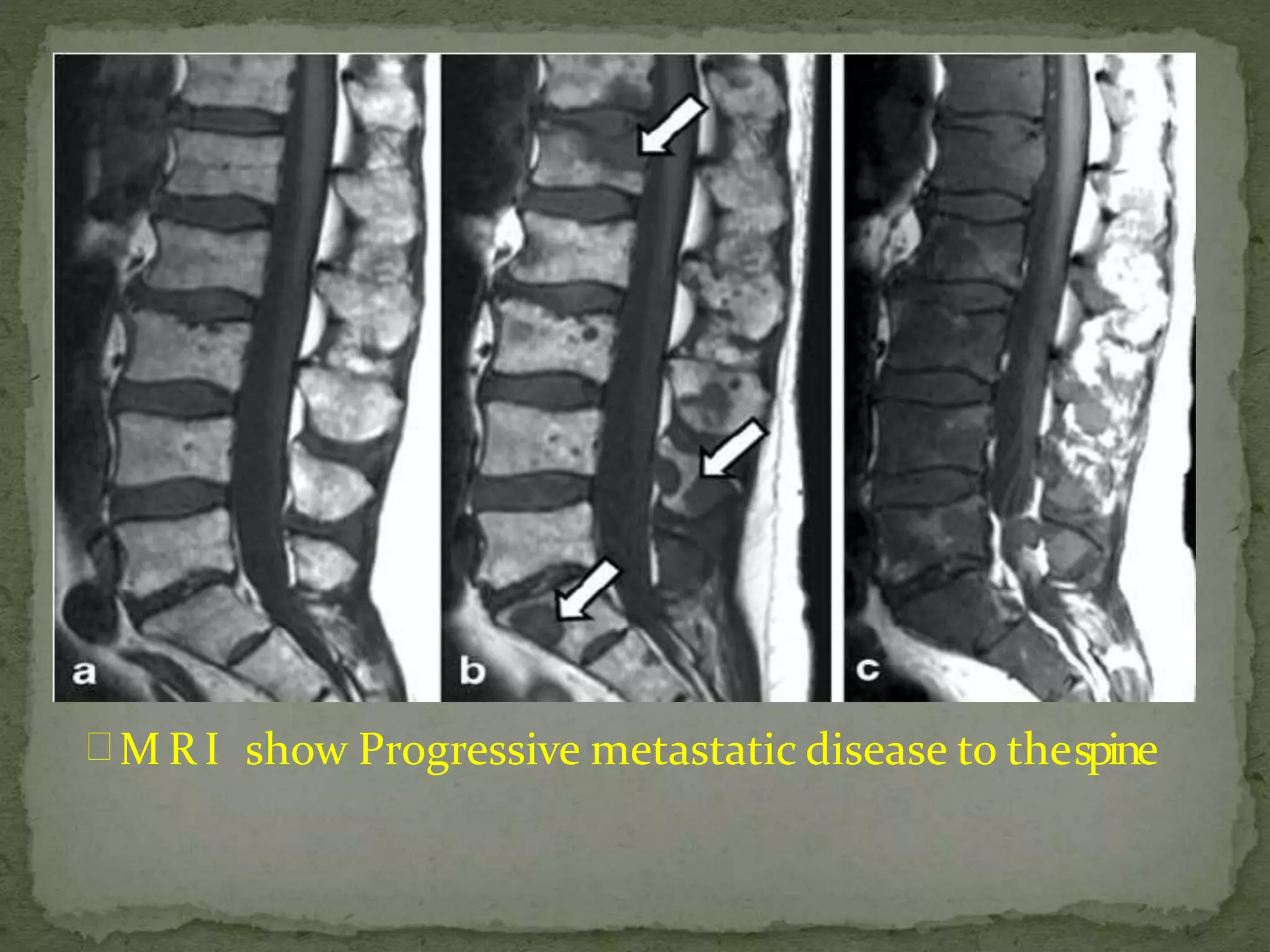
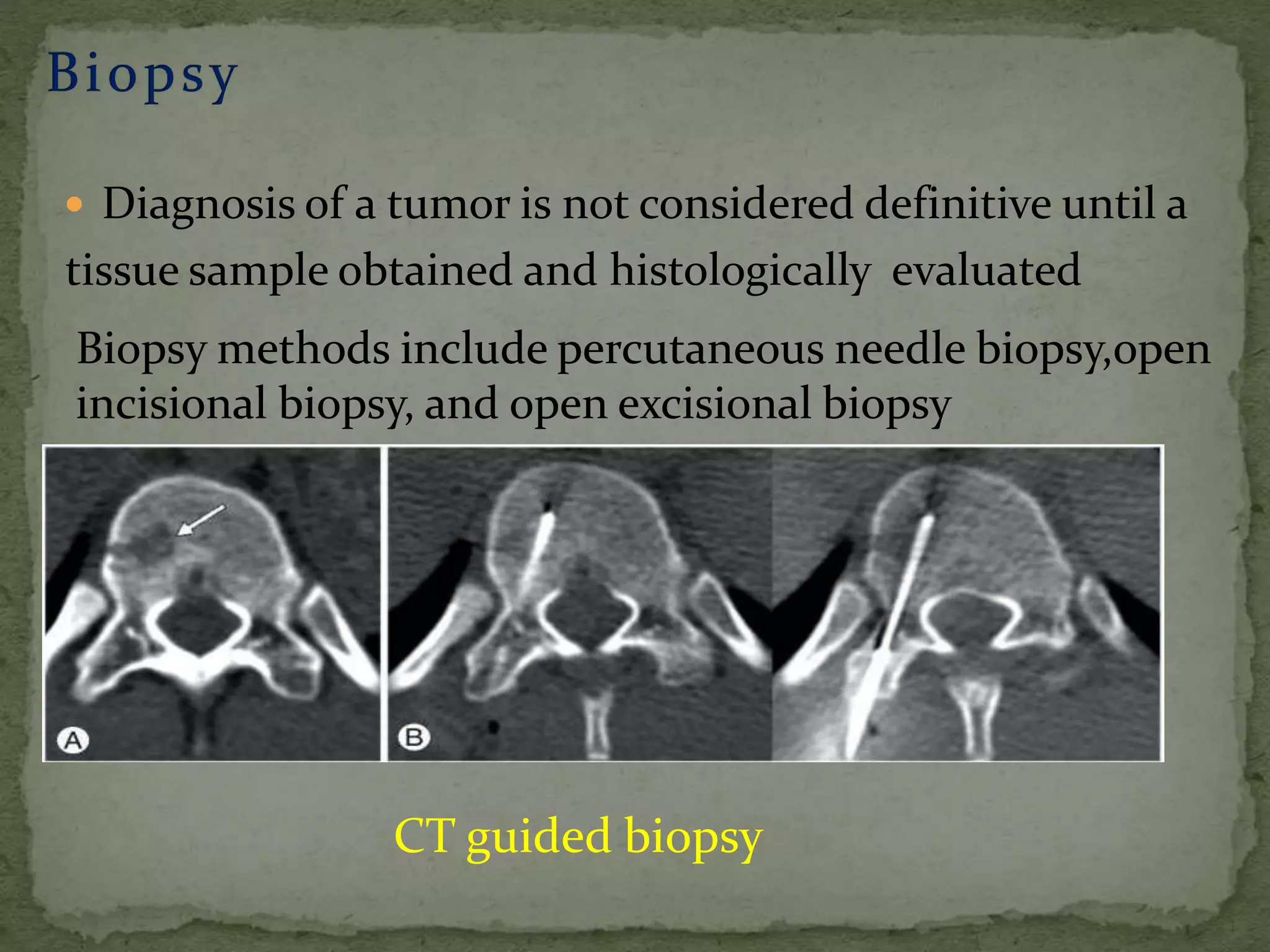
3. Imaging like CT, MRI and bone scans are used to identify the location and extent of tumors. Tissue biopsy is needed to confirm diagnosis.
4. Treatment involves a multidisciplinary approach with surgery, radiation, chemotherapy and steroid/medical management. The goal of surgery is wide or en bloc resection with spinal reconstruction and stabilization