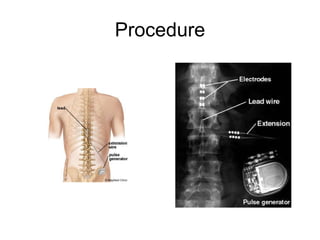
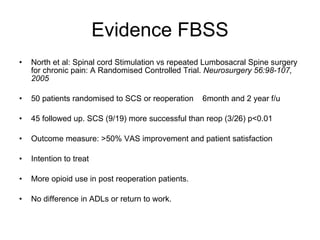
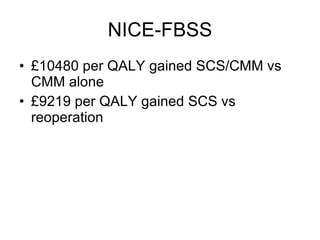
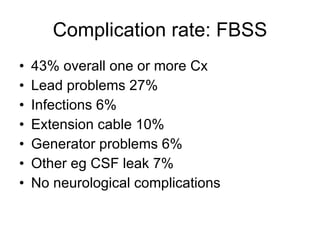
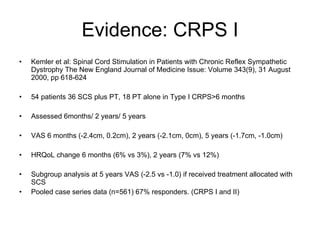
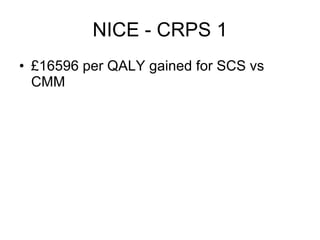
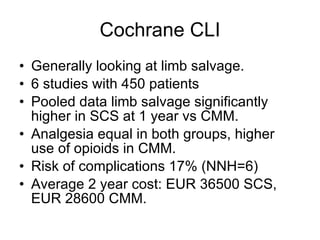
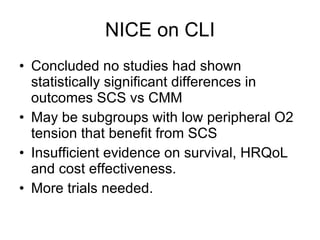
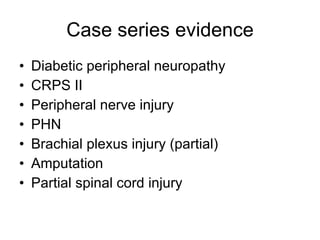
1. The document discusses spinal cord stimulation service, including its history, components, mechanisms of action, indications, procedures, evidence from studies, outcomes, complications, and guidelines.
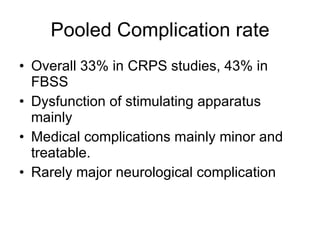
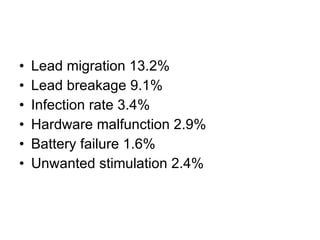
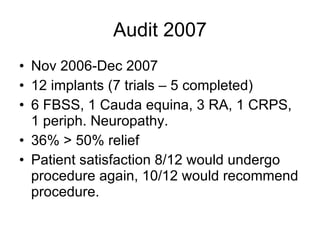
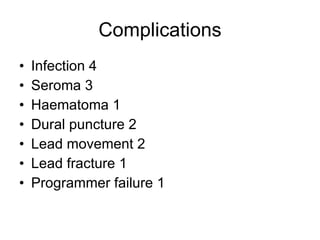
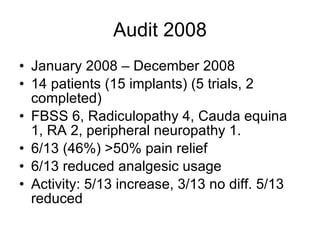
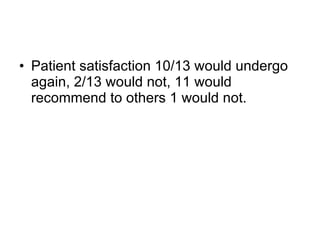
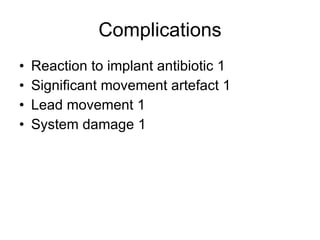
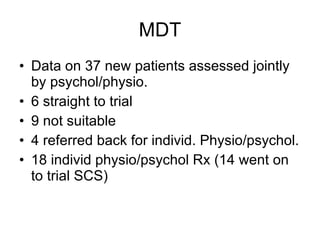
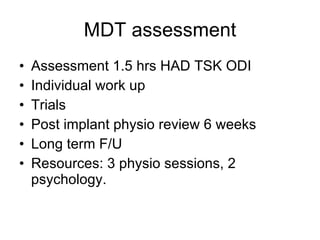
2. It provides details on the multidisciplinary team approach used, case studies, audits of outcomes that found over 50% pain relief in many patients, and complications rates of around 30-40%.
3. The document reflects on the author's experience with the multidisciplinary team approach and how working with complex patients has been an enjoyable learning experience.