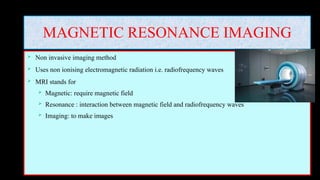
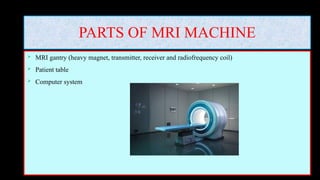
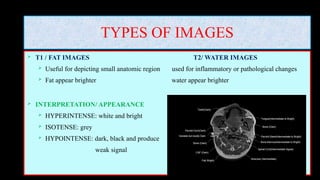
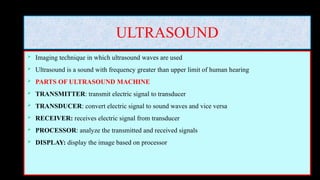
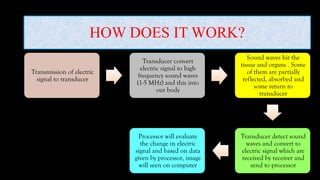
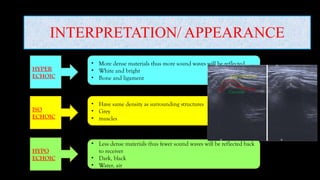
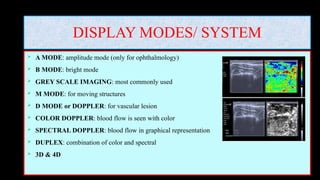
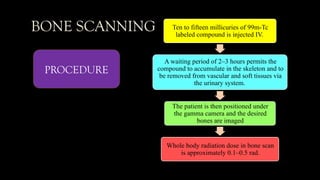
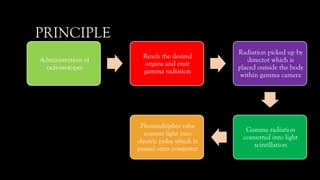
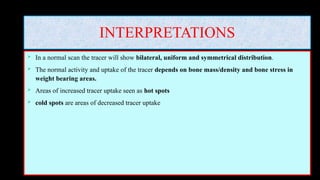
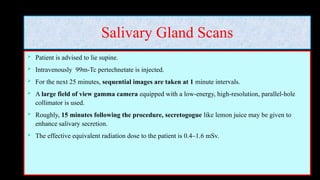
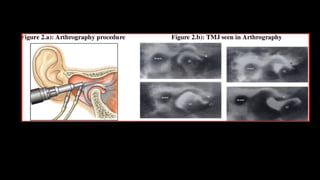
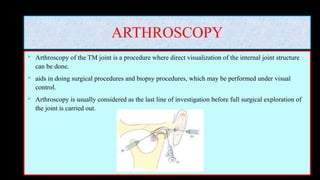
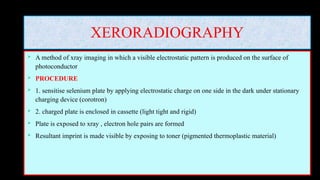
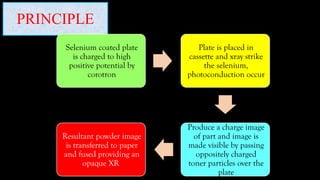
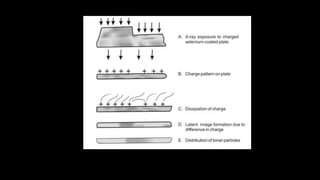
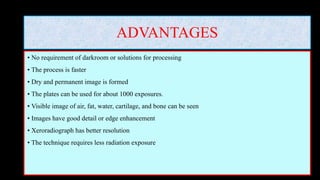
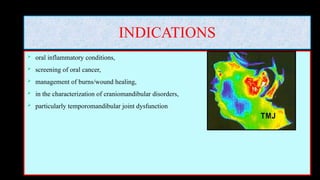
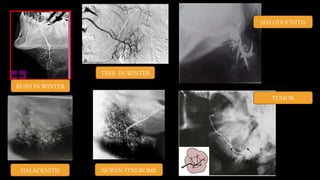
The document discusses various specialized imaging modalities in oral medicine and radiology, including MRI, ultrasound, nuclear medicine, arthrography, and more. It outlines the principles, procedures, advantages, disadvantages, and clinical applications of each technique, emphasizing their non-invasive nature and detailed imaging capabilities. The document serves as a comprehensive guide for understanding these imaging methods in diagnosing and managing oral and maxillofacial conditions.