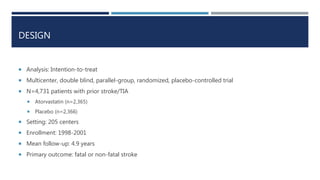
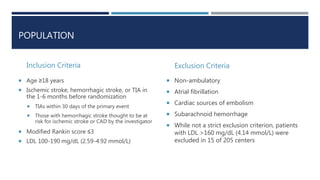
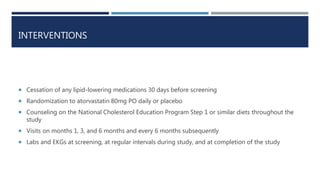
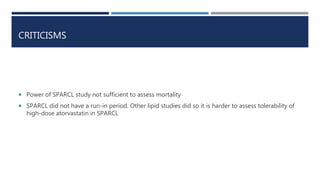
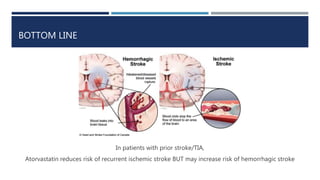
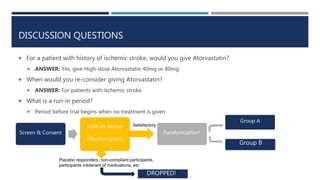
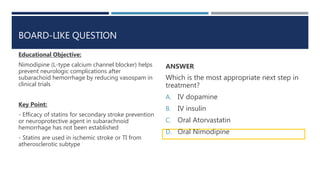
The SPARCL trial investigated whether high-dose atorvastatin reduces the risk of recurrent stroke in patients with a history of stroke or transient ischemic attack (TIA). The trial randomized 4,731 patients to atorvastatin 80mg daily or placebo. Atorvastatin reduced the risk of recurrent ischemic stroke but increased the risk of hemorrhagic stroke. The trial showed that high-dose statin therapy can lower the risk of another stroke in patients with a previous stroke or TIA through reduction of cholesterol levels.