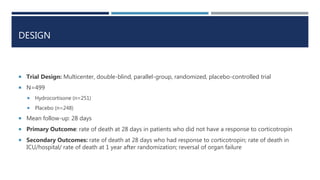
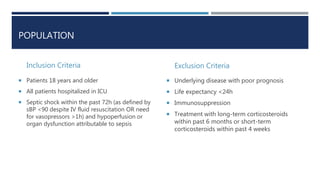
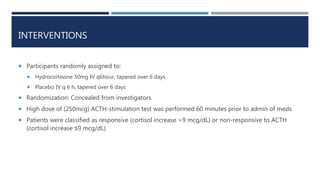
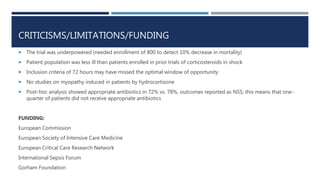
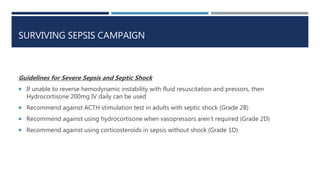
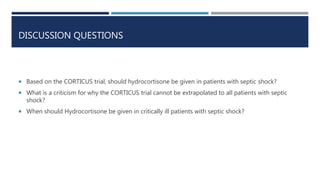
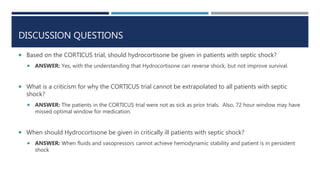
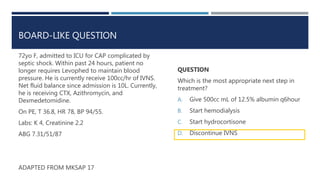
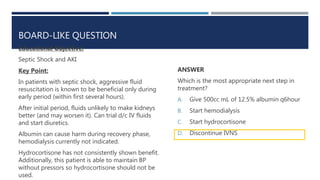
The CORTICUS trial investigated whether low-dose hydrocortisone therapy improves survival in critically ill patients with septic shock. The trial randomized 499 patients with septic shock to receive hydrocortisone or placebo. It found that hydrocortisone hastened the reversal of shock in patients whose shock was reversed, but did not confer an overall survival benefit. Based on this trial and others, corticosteroids should not be routinely used in adult patients with septic shock, though they may benefit selected patients.