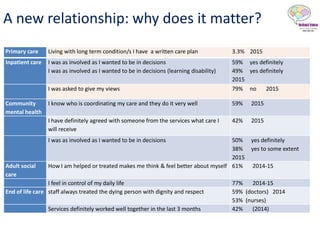
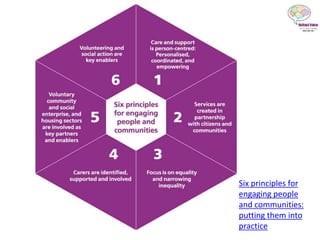
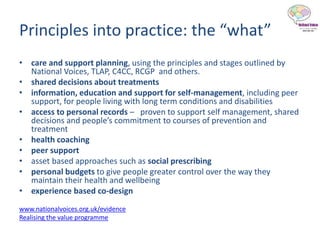
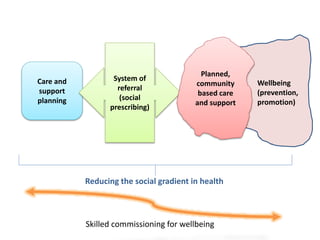
The document outlines six principles for engaging people and communities in health and care, emphasizing person-centered care and the importance of patient involvement in decision-making. It highlights the need for healthier outcomes and improved experiences through community-focused approaches and shared decision-making in care planning. Additionally, it discusses the necessity of supportive frameworks and local partnerships to drive change and recognize patients as experts in their own care.