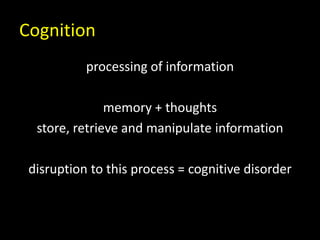
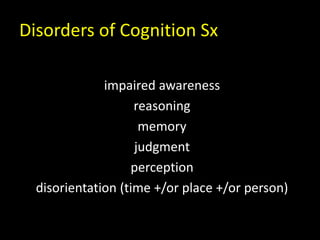
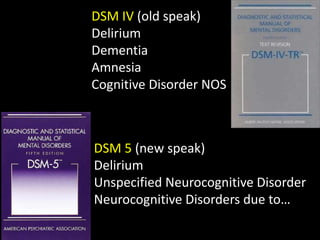
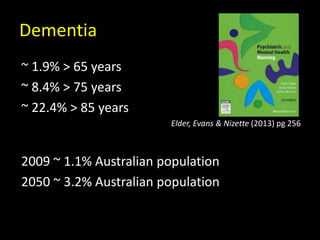
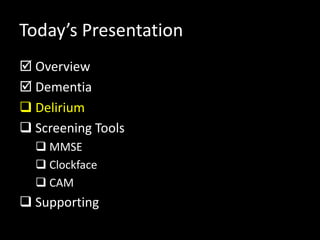
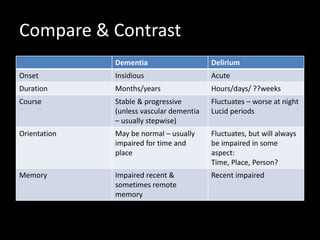
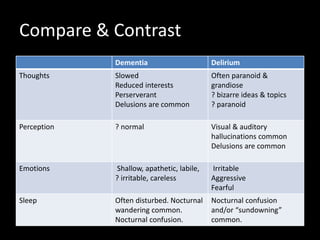
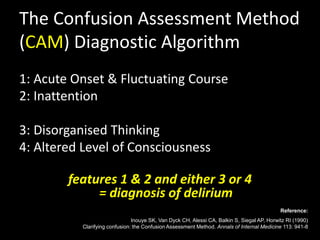
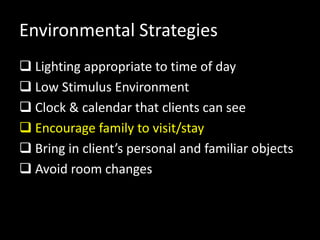
This document provides an overview of assessing and caring for older adults with mental illnesses. It discusses key concepts like dementia, delirium, and screening tools. Nurses play an important role in screening for cognitive issues using tools like the Mini-Mental State Examination and supporting patients. The presentation aims to help nurses understand common conditions, distinguish between dementia and delirium, and properly manage and support older adults with mental illnesses.



![Clinical Practice Strategies [1]
Interpreter for culturally & linguistically
diverse (CALD) patients/clients
Indigenous Liaison Officer
Eating & Drinking
Hearing Aids?
Glasses?
Bowels – avoid constipation
Mobilisation](https://image.slidesharecdn.com/session8lecture-150116193427-conversion-gate02/85/Dementia-and-Delirium-39-320.jpg)
![Clinical Practice Strategies [2]
Encourage independence in basic ADLs
Medication review
Promote sufficient sleep at night
Manage discomfort or pain
Provide orienting information
Minimise use of indwelling catheters
Avoid use of physical restraints
Avoid polypharmacy/psychoactive drugs](https://image.slidesharecdn.com/session8lecture-150116193427-conversion-gate02/85/Dementia-and-Delirium-40-320.jpg)