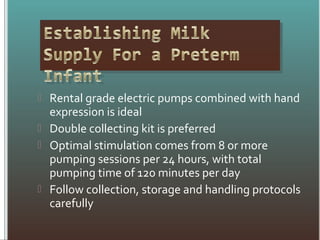
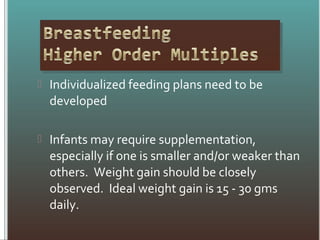
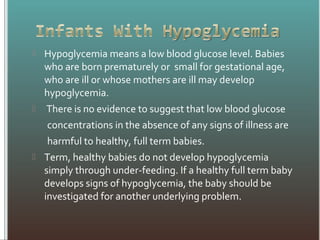
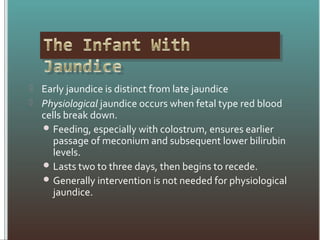
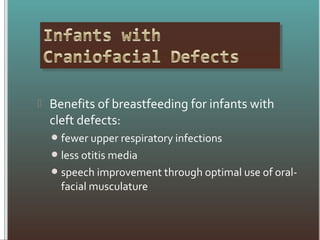
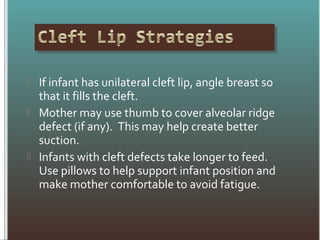
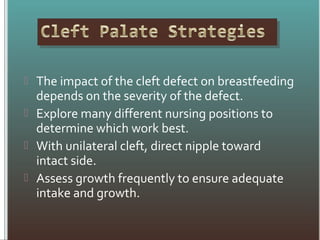
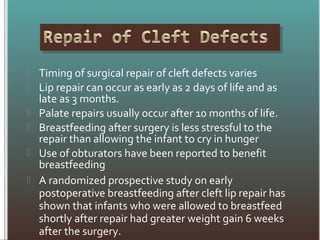
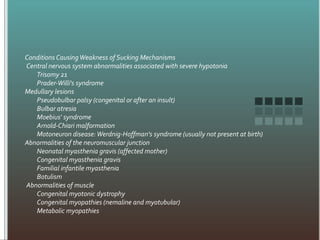
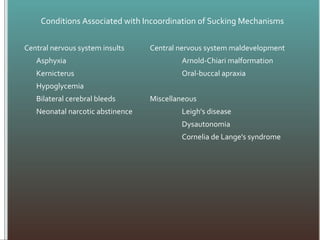
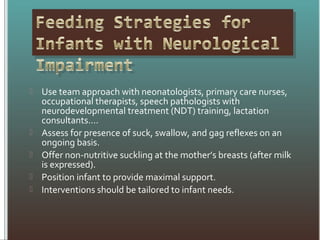
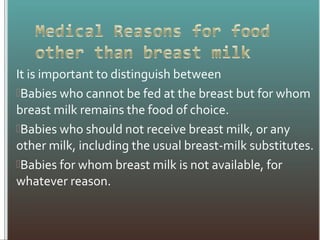
This document discusses strategies for breastfeeding special needs infants, including those born preterm or with low birth weight. It outlines recommendations for pumping and storing breastmilk, as well as supporting skin-to-skin contact and breastfeeding. The document also describes managing common clinical issues like jaundice, hypoglycemia, and dehydration. Finally, it notes that while breastmilk is usually best, in rare cases of inborn errors of metabolism, special formulas may be needed.