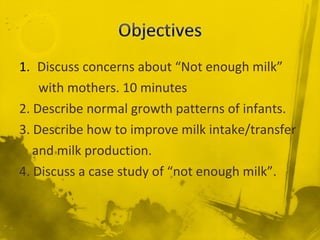
This document discusses concerns about low milk supply in mothers and strategies to address this issue. It covers normal breastfeeding and infant growth patterns, factors that influence milk production, signs of inadequate milk intake in infants, and interventions to improve milk supply and transfer. These include ensuring proper latch and frequent, on-demand feedings to stimulate milk production as well as monitoring mothers and infants to identify and address supply issues. The goal is to provide appropriate support to establish and maintain a sufficient milk supply through education and early intervention.