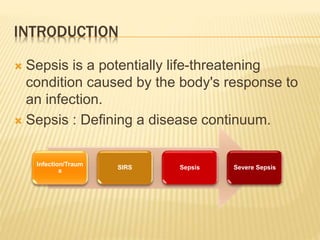
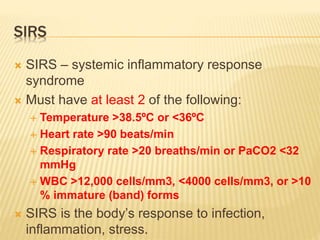
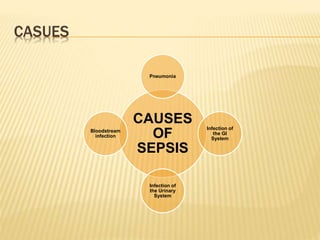
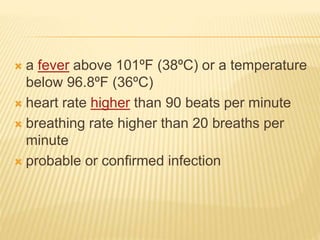
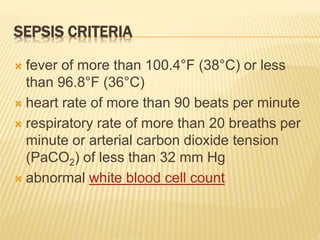
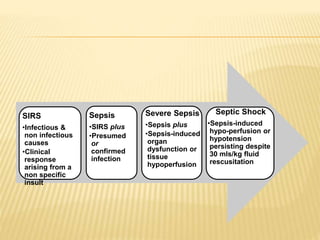
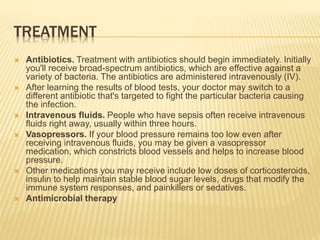
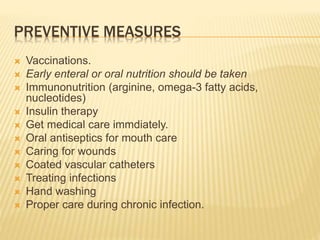
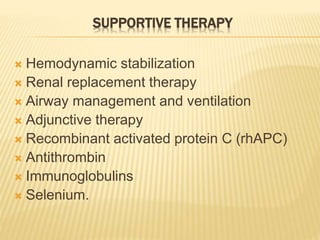
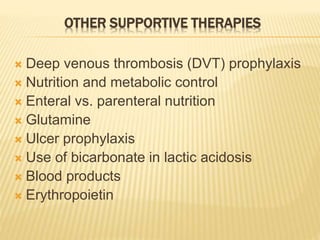
Sepsis is a life-threatening condition caused by the body's response to an infection. It occurs when an infection you already have triggers a chain reaction throughout your body. Sepsis is diagnosed when a person has both an infection and signs of a systemic inflammatory response. Treatment involves administering broad-spectrum antibiotics intravenously, giving intravenous fluids, and using vasopressors if blood pressure is too low. Preventive measures include vaccinations, early nutrition, immunonutrition, and proper wound and infection care.