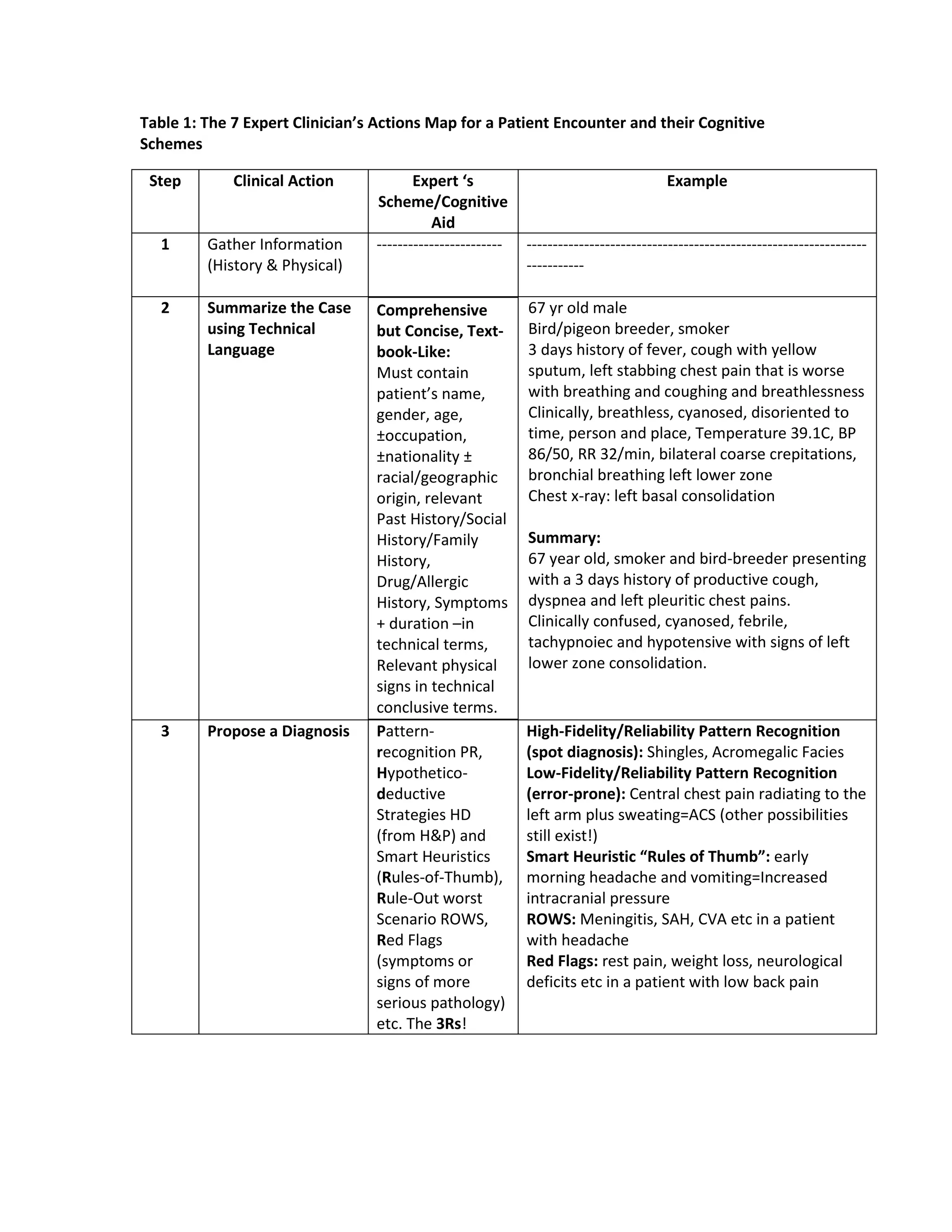
The document outlines 7 steps expert clinicians follow during a patient encounter: 1) gather information, 2) summarize the case, 3) propose a diagnosis, 4) generate a differential diagnosis, 5) order tests rationally, 6) confirm a diagnostic label, and 7) plan therapeutic interventions and discharge. It provides examples of cognitive aids used at each step, such as summarizing patient history concisely, using pattern recognition to propose diagnoses, and considering anatomical, physiological and pathological factors for differential diagnoses. Key diagnostic tests are matched to pre-test probabilities based on their sensitivity and specificity.