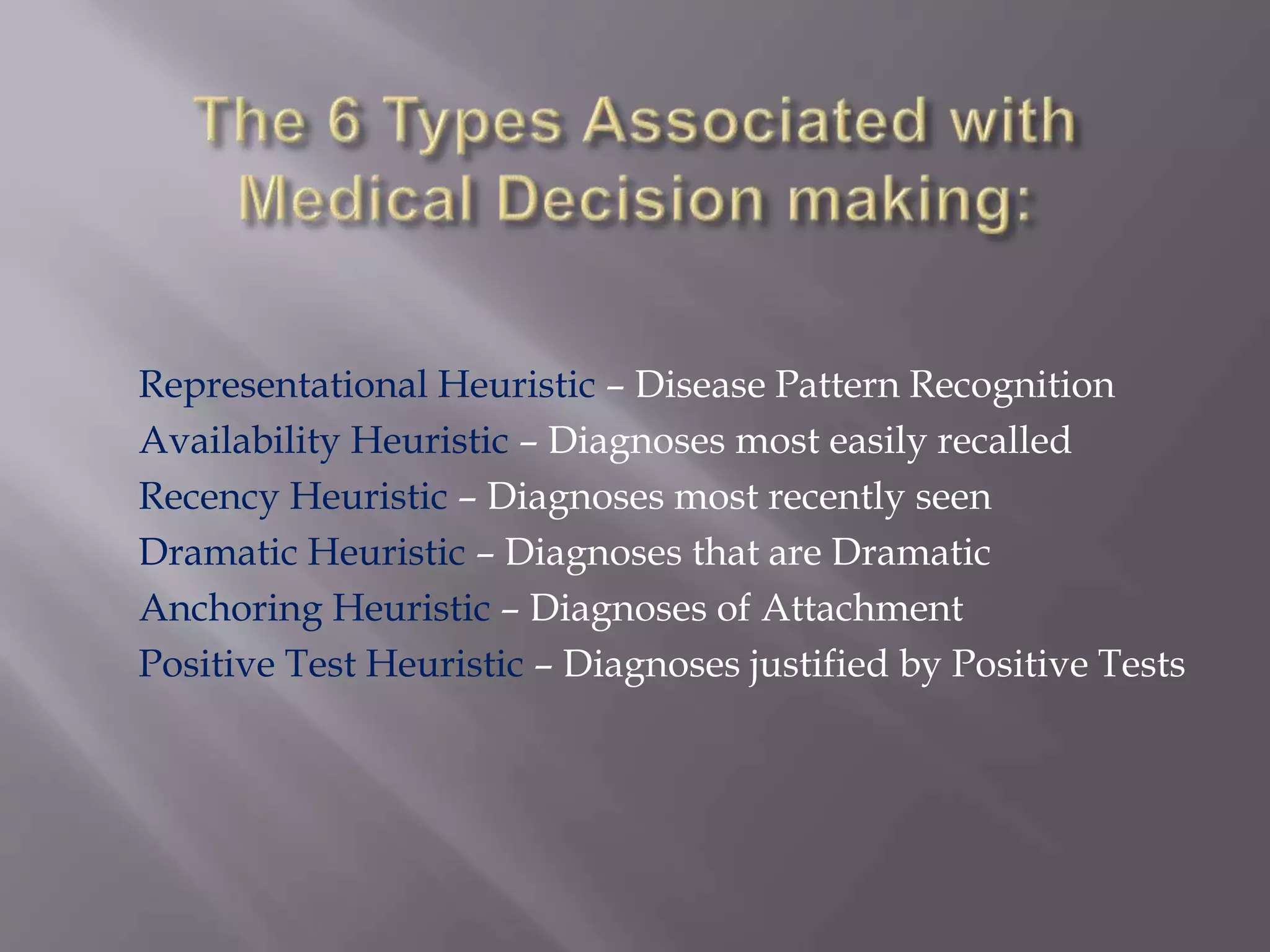
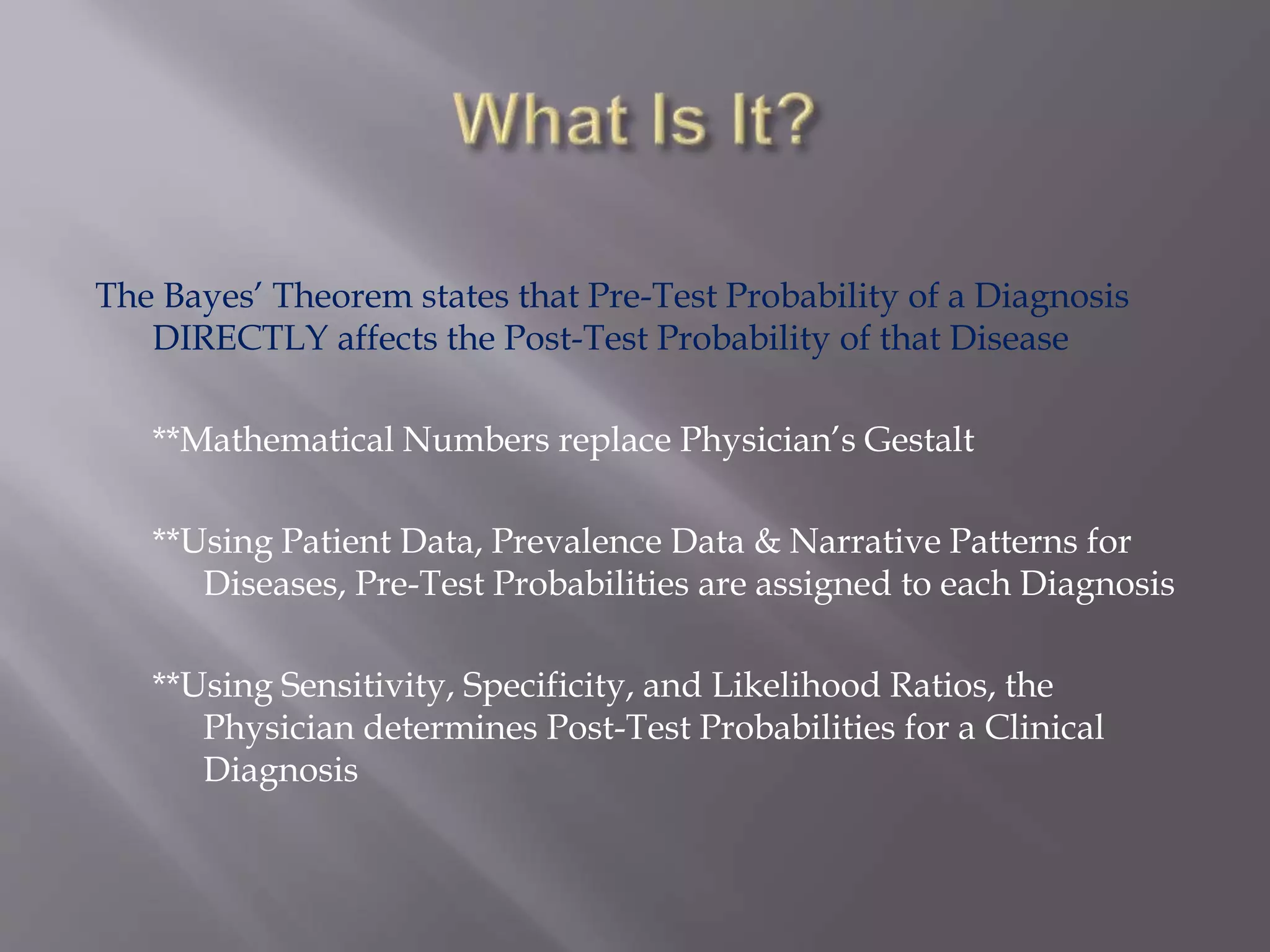
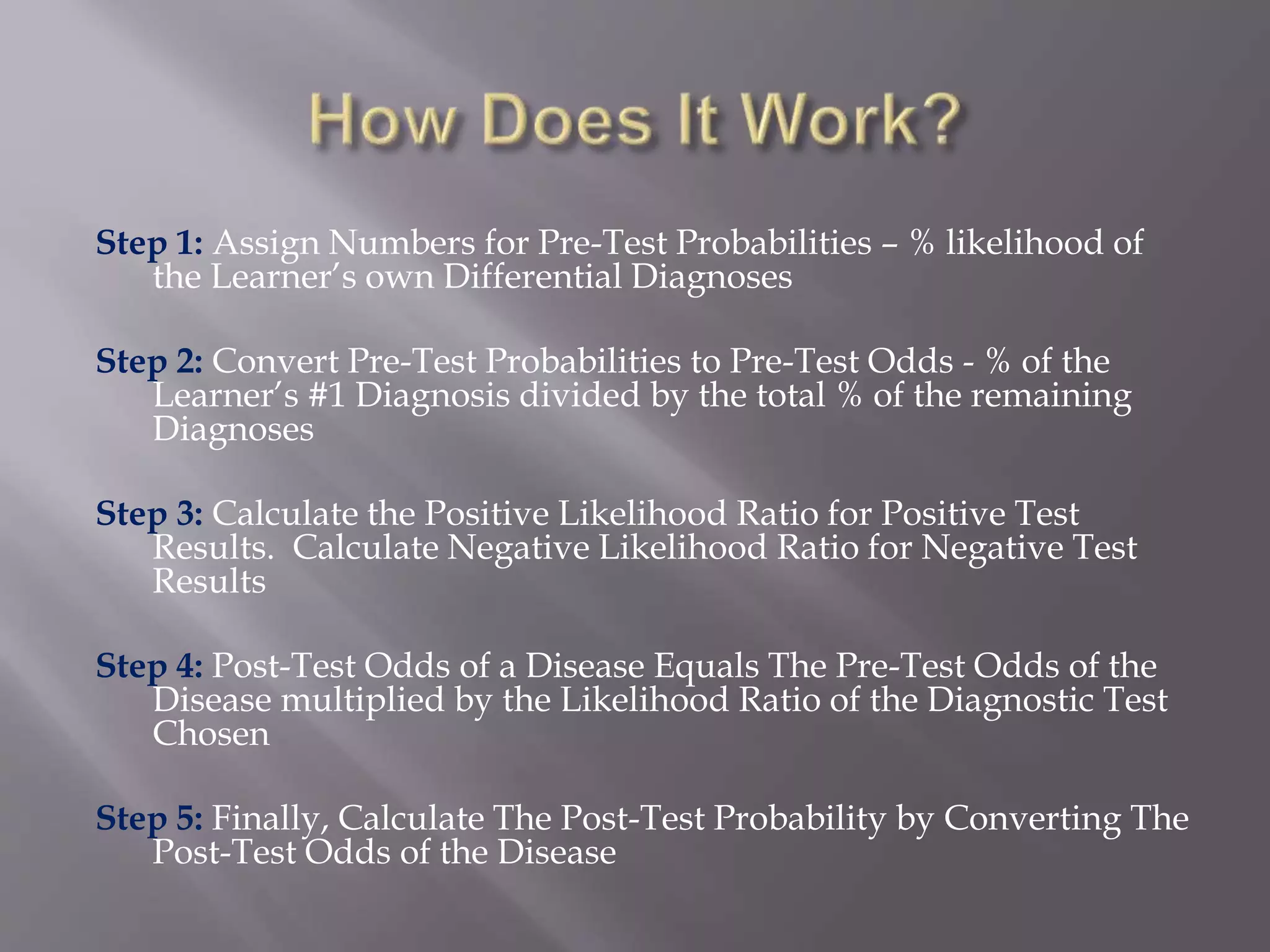
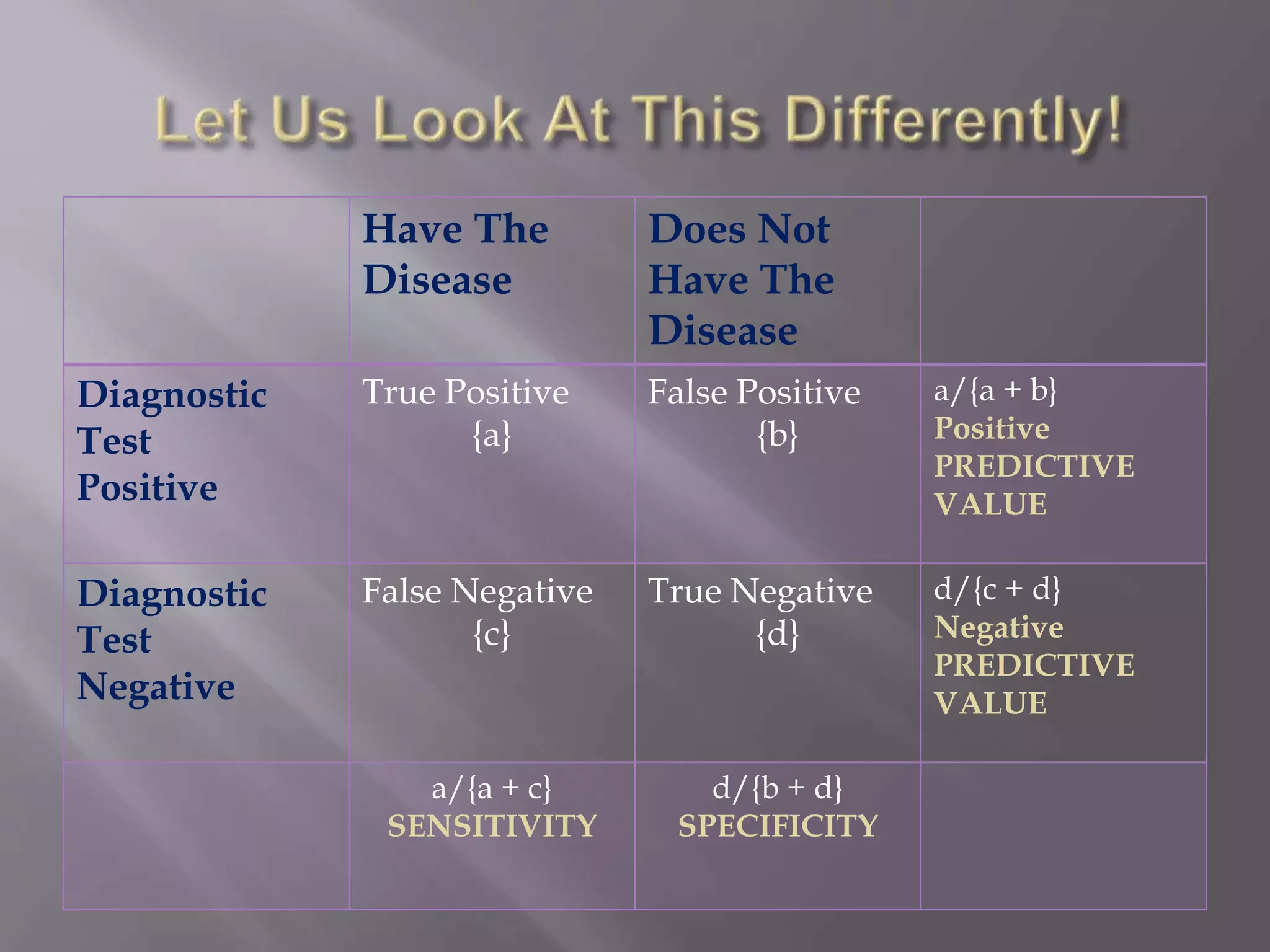
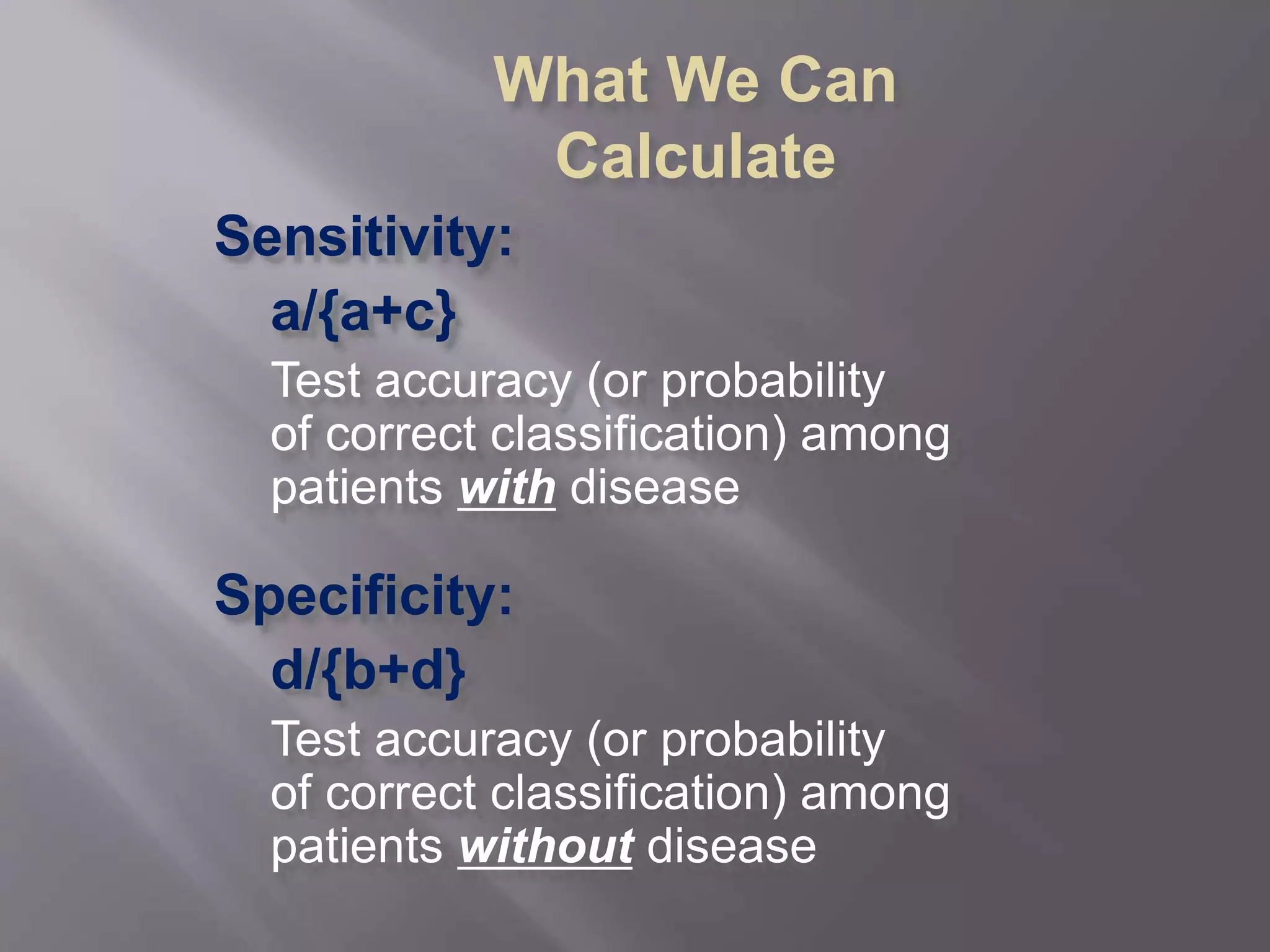
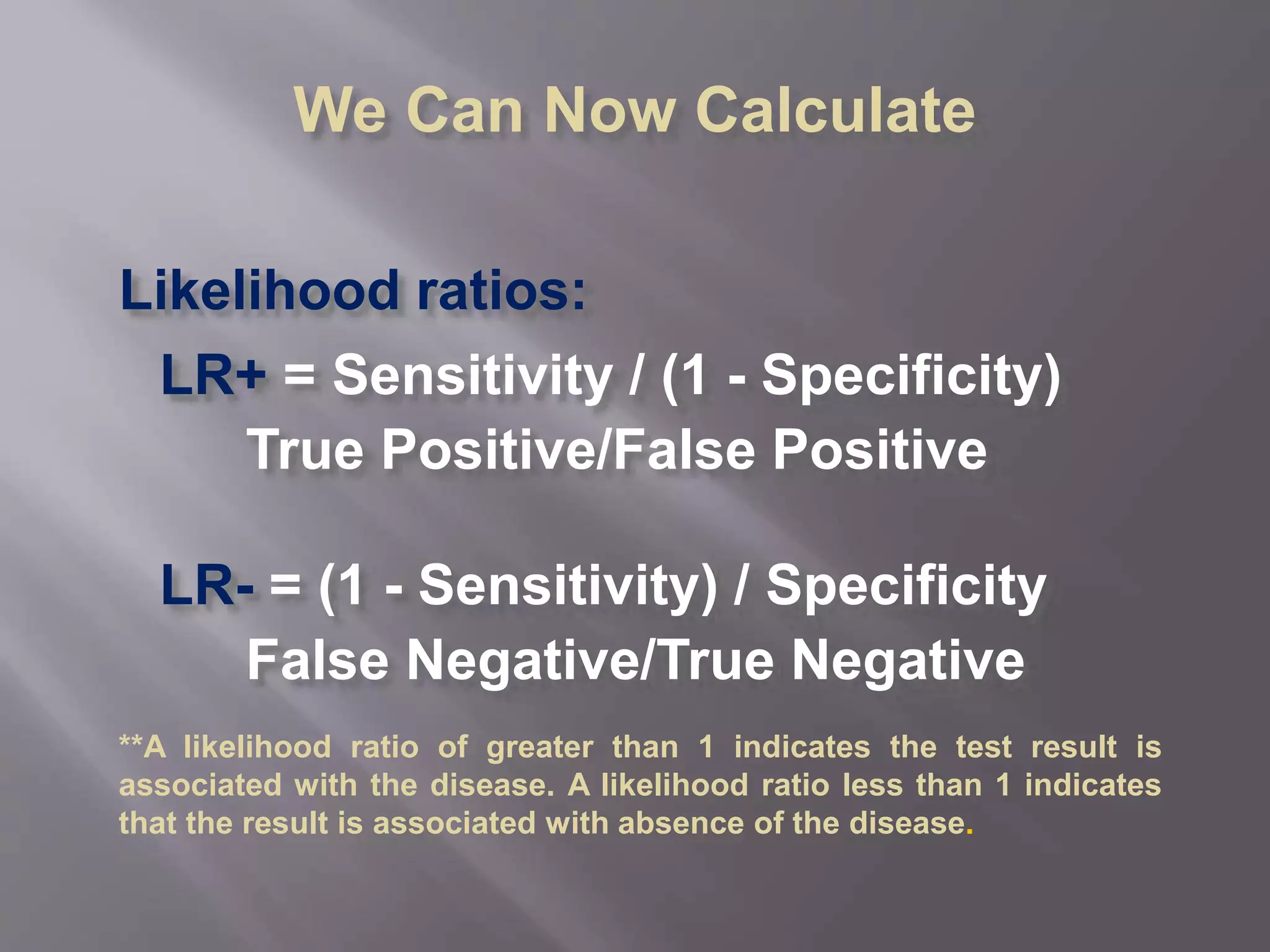
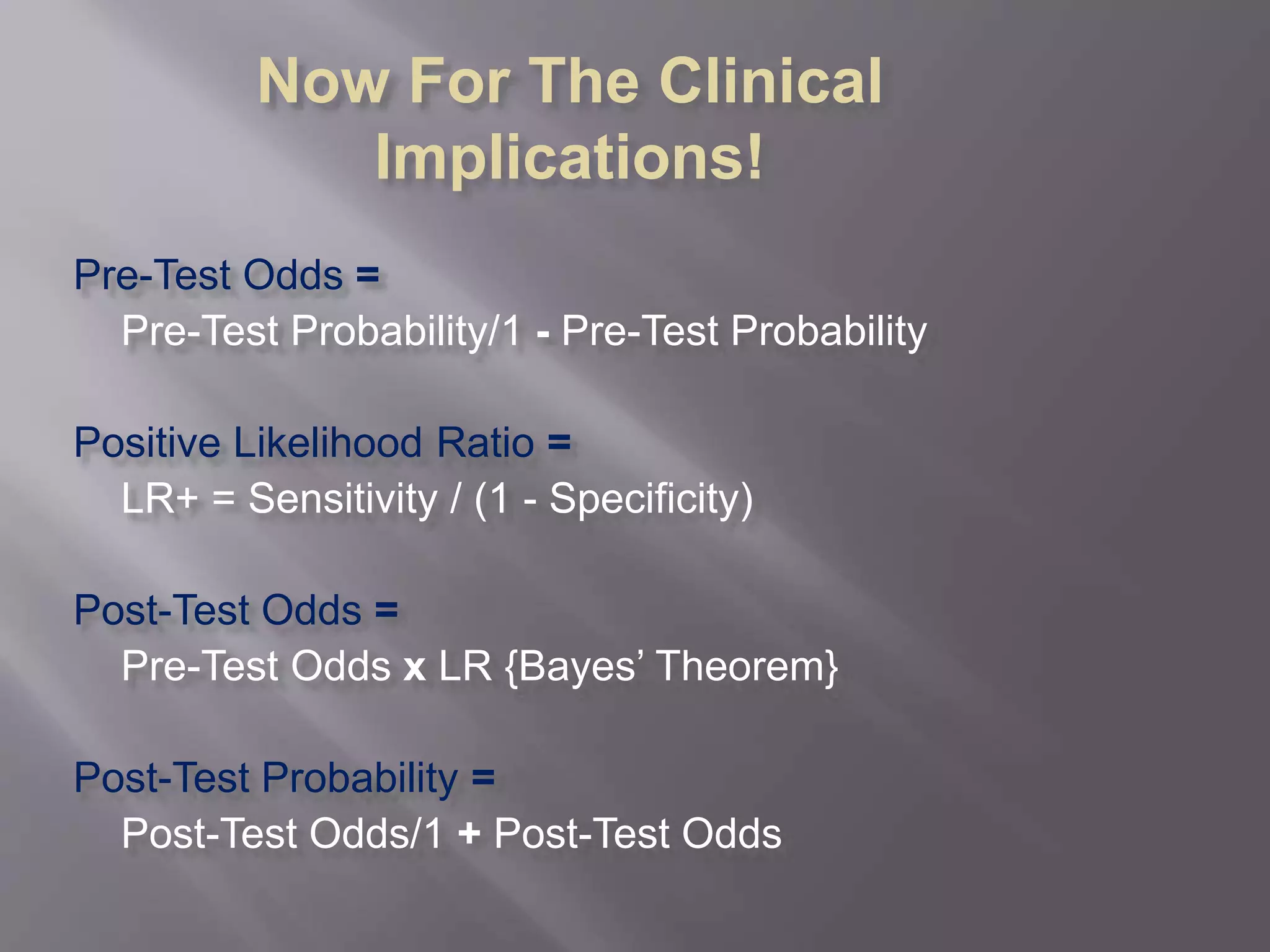
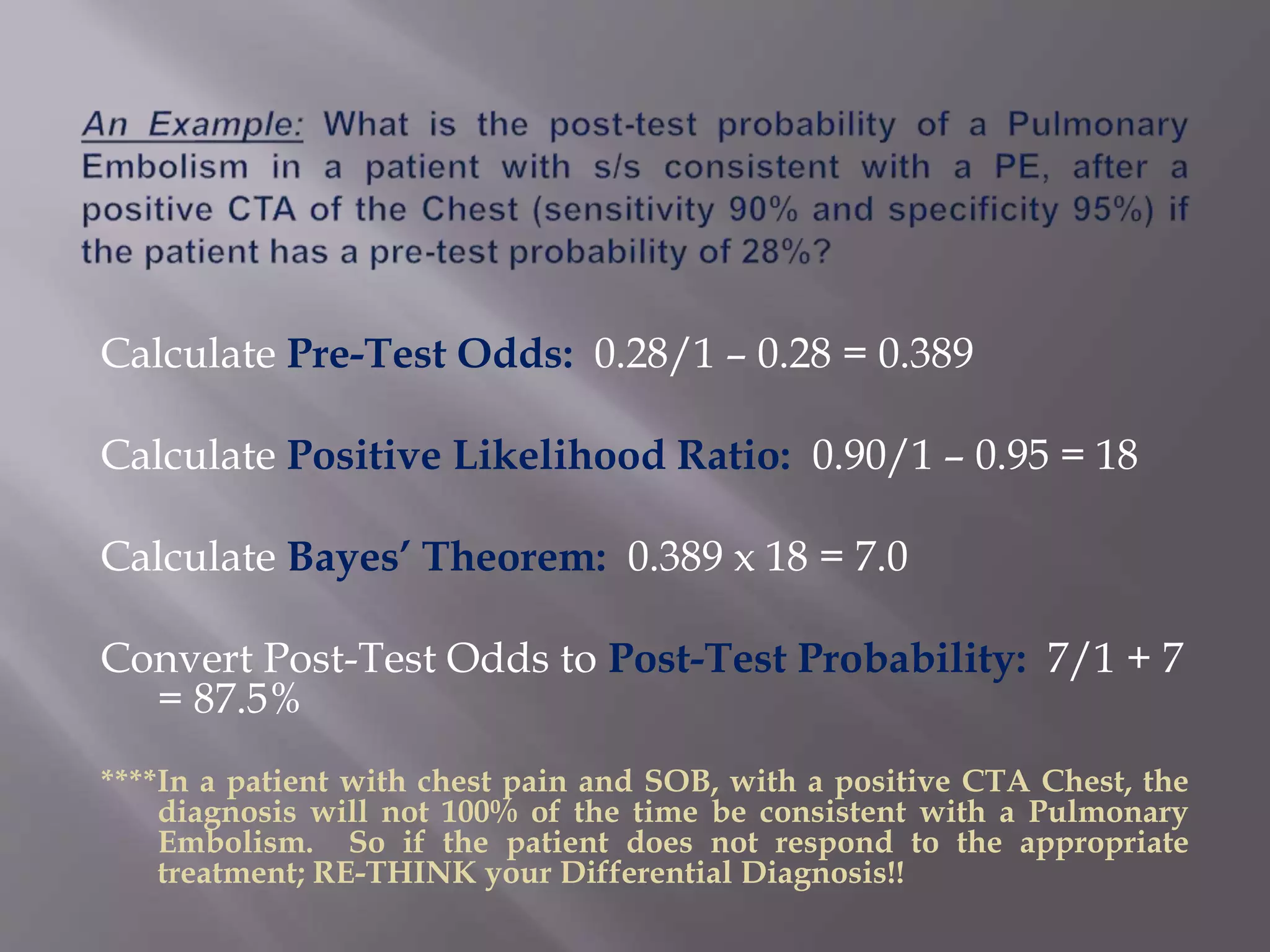
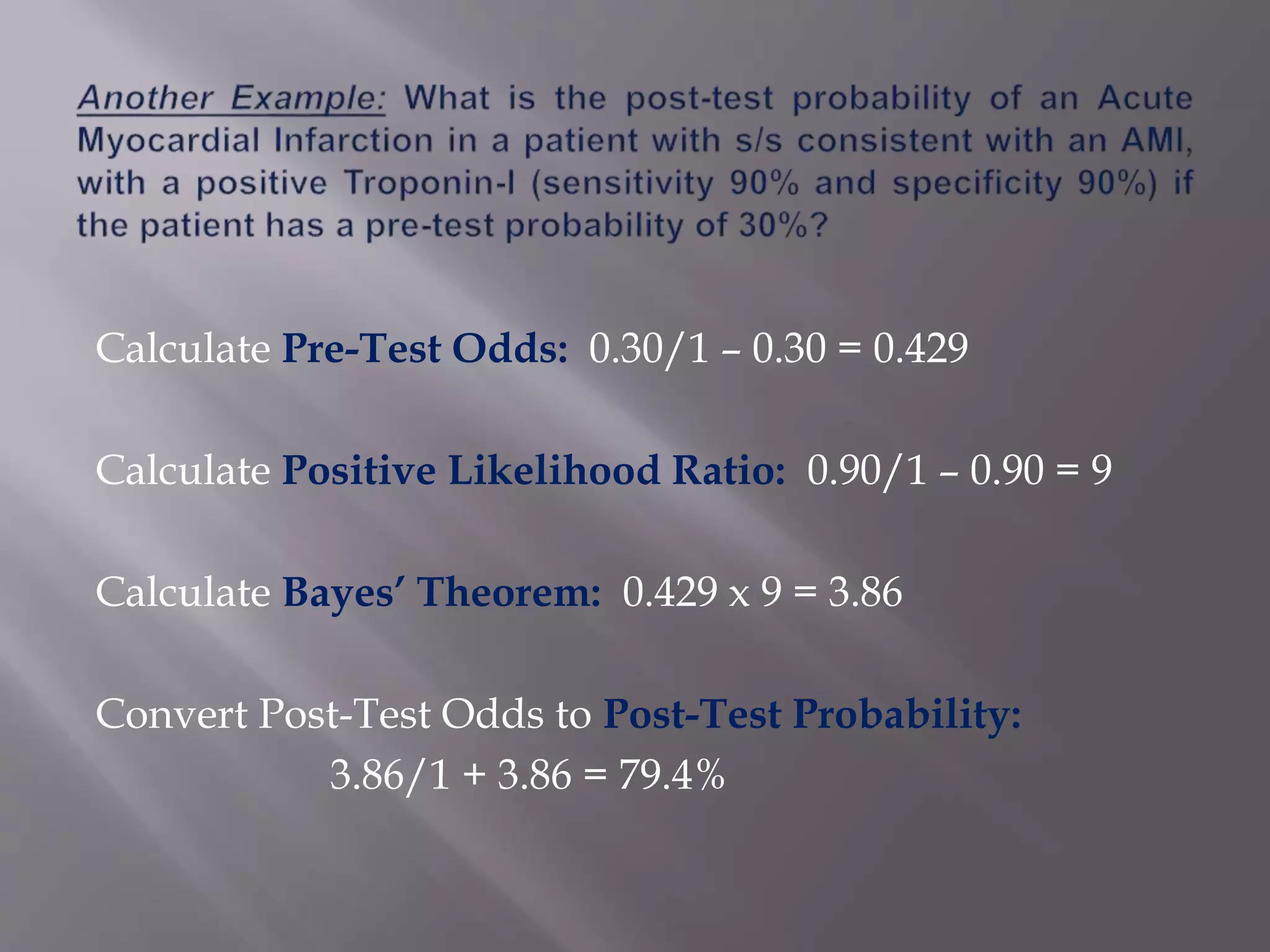
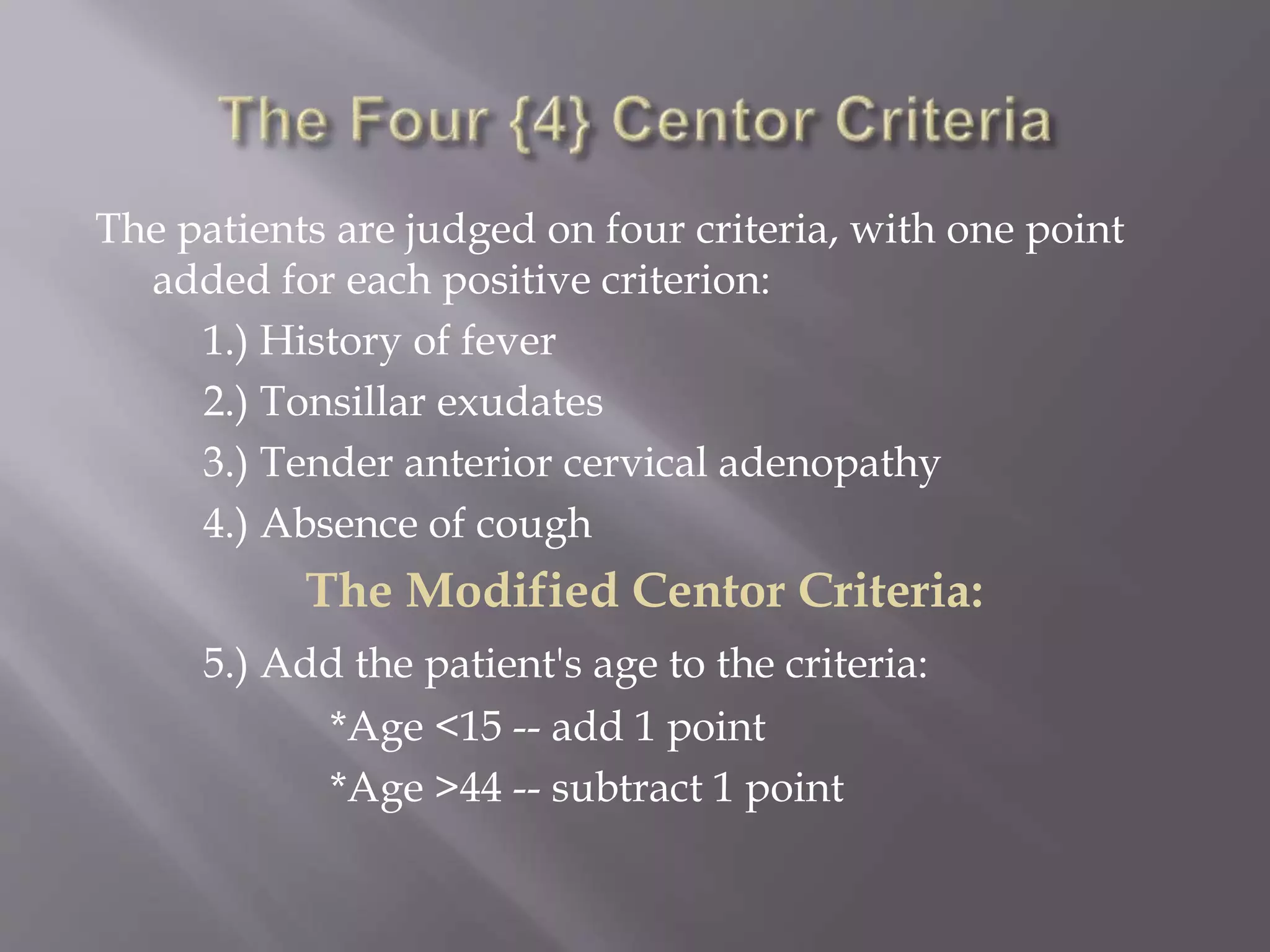
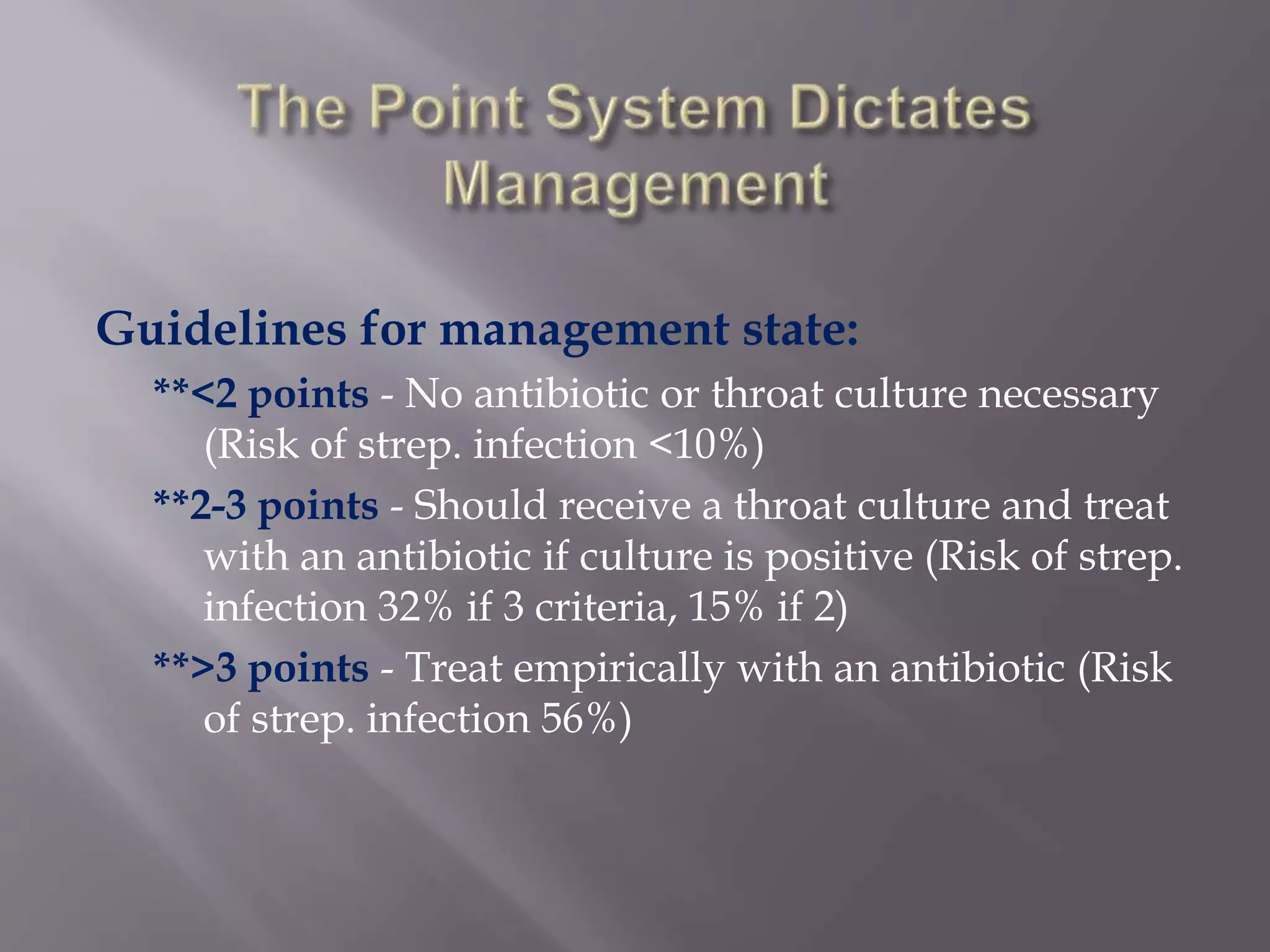
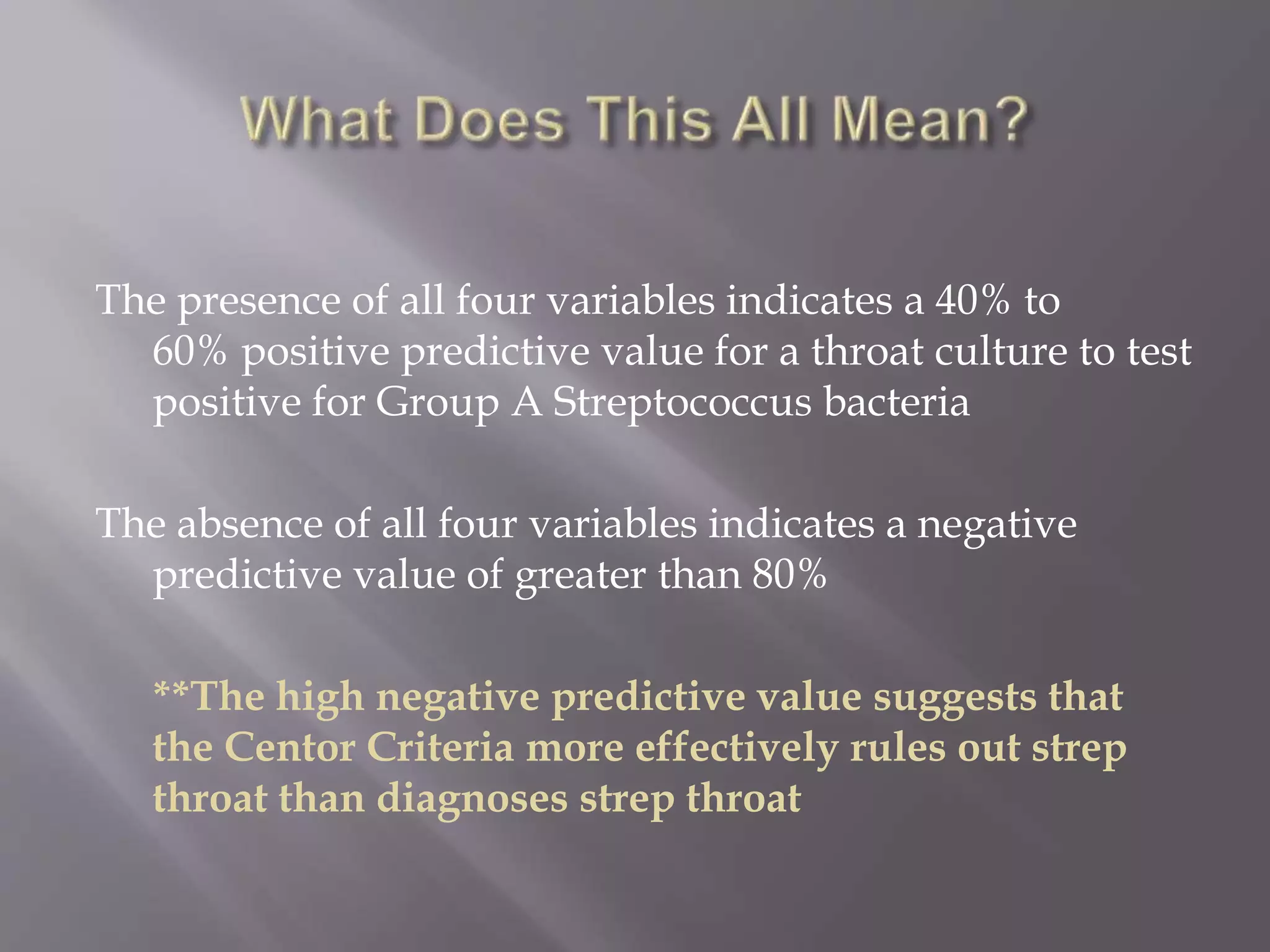
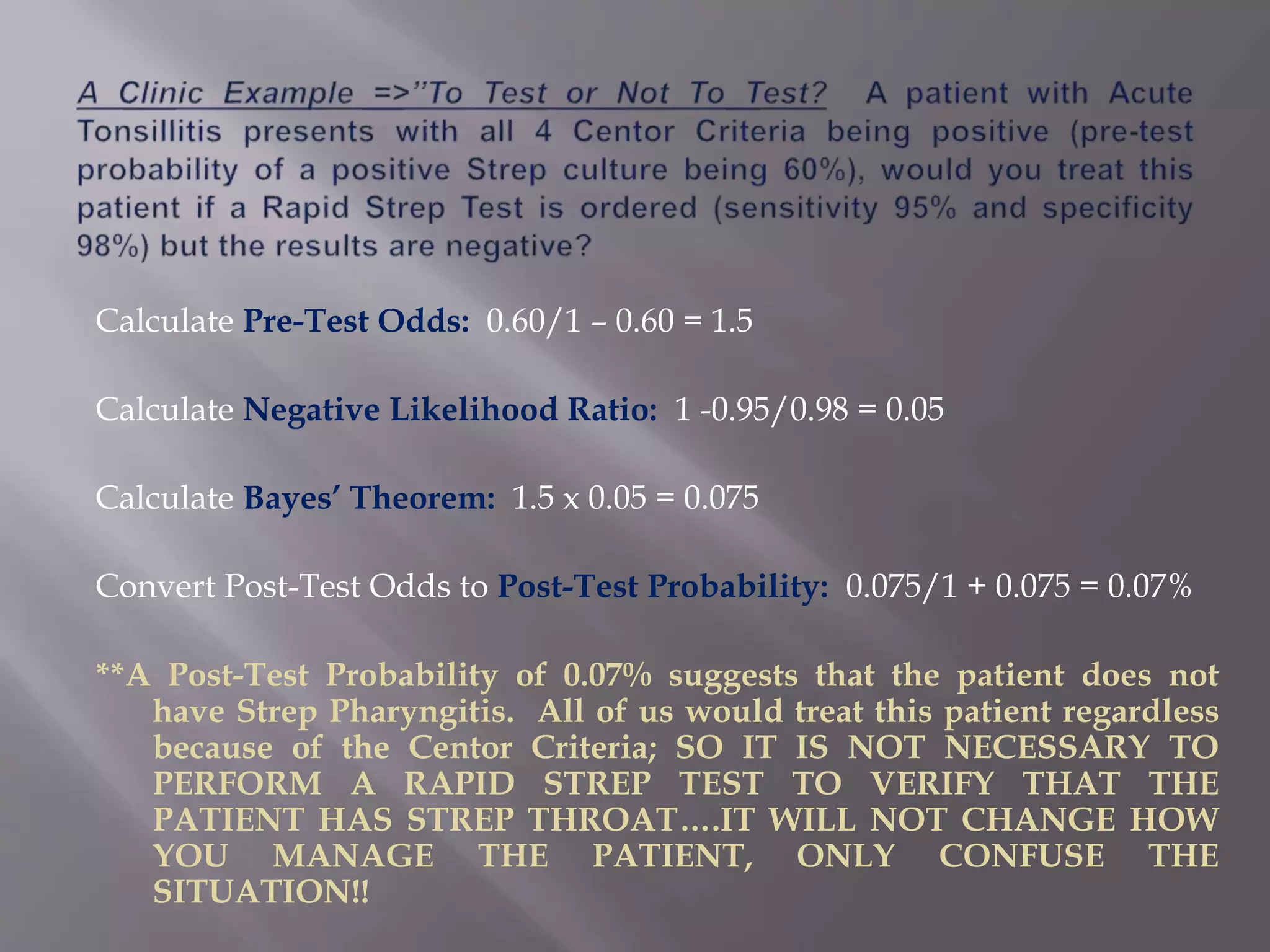
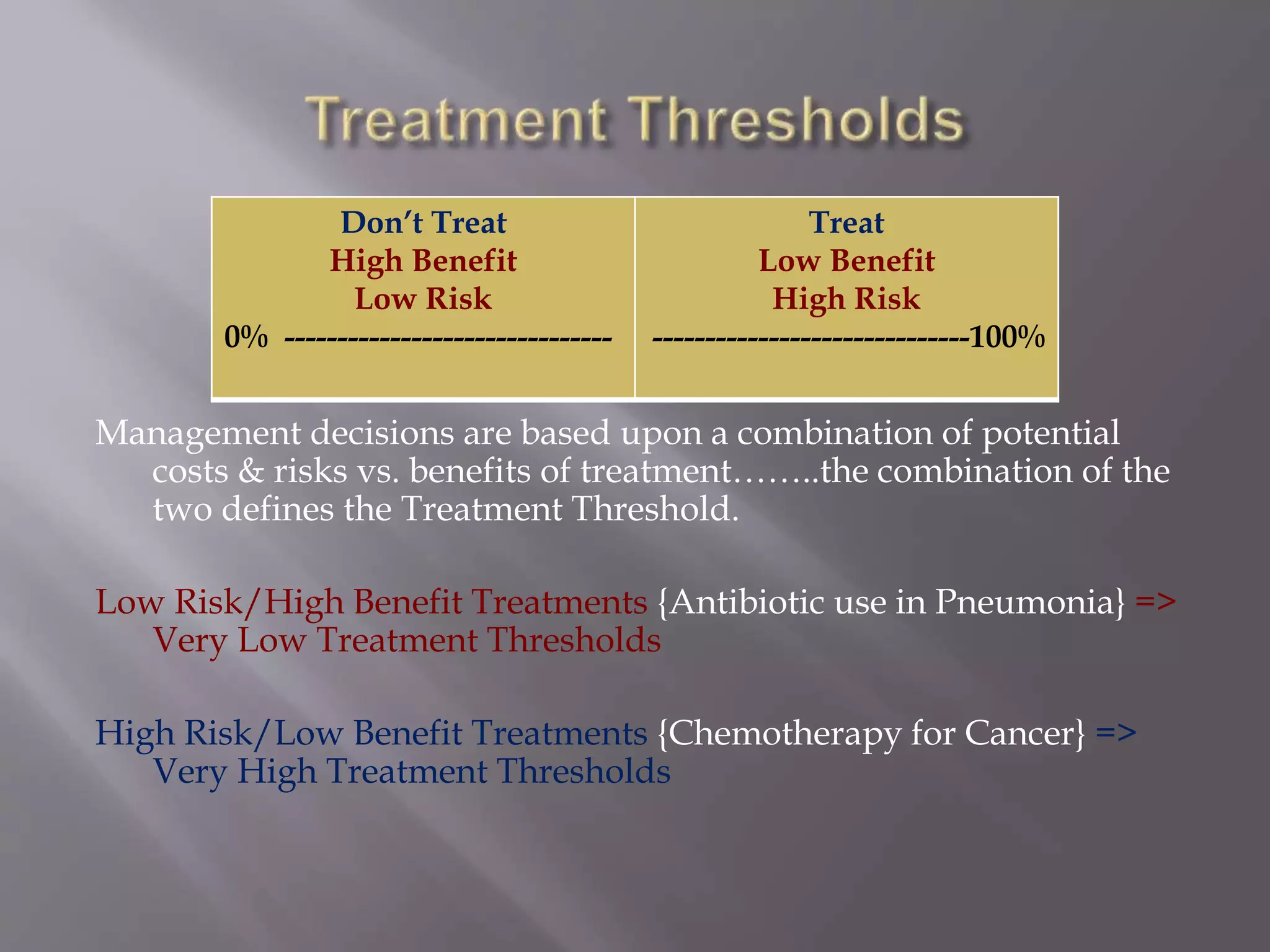
This document discusses teaching clinical reasoning skills to learners. It emphasizes using both analytical and non-analytical reasoning approaches. Non-analytical reasoning like pattern recognition is intuitive for experts but can lead to errors for novices. The document recommends teaching Bayesian reasoning to help learners develop analytical skills in a structured way. It provides examples of using sensitivity, specificity, and likelihood ratios to calculate pre-test and post-test probabilities to diagnose conditions. Developing these quantitative reasoning abilities helps learners strengthen clinical decision making and determine appropriate treatment thresholds. Active learning approaches that challenge learners' clinical judgments are advocated over passive knowledge acquisition.