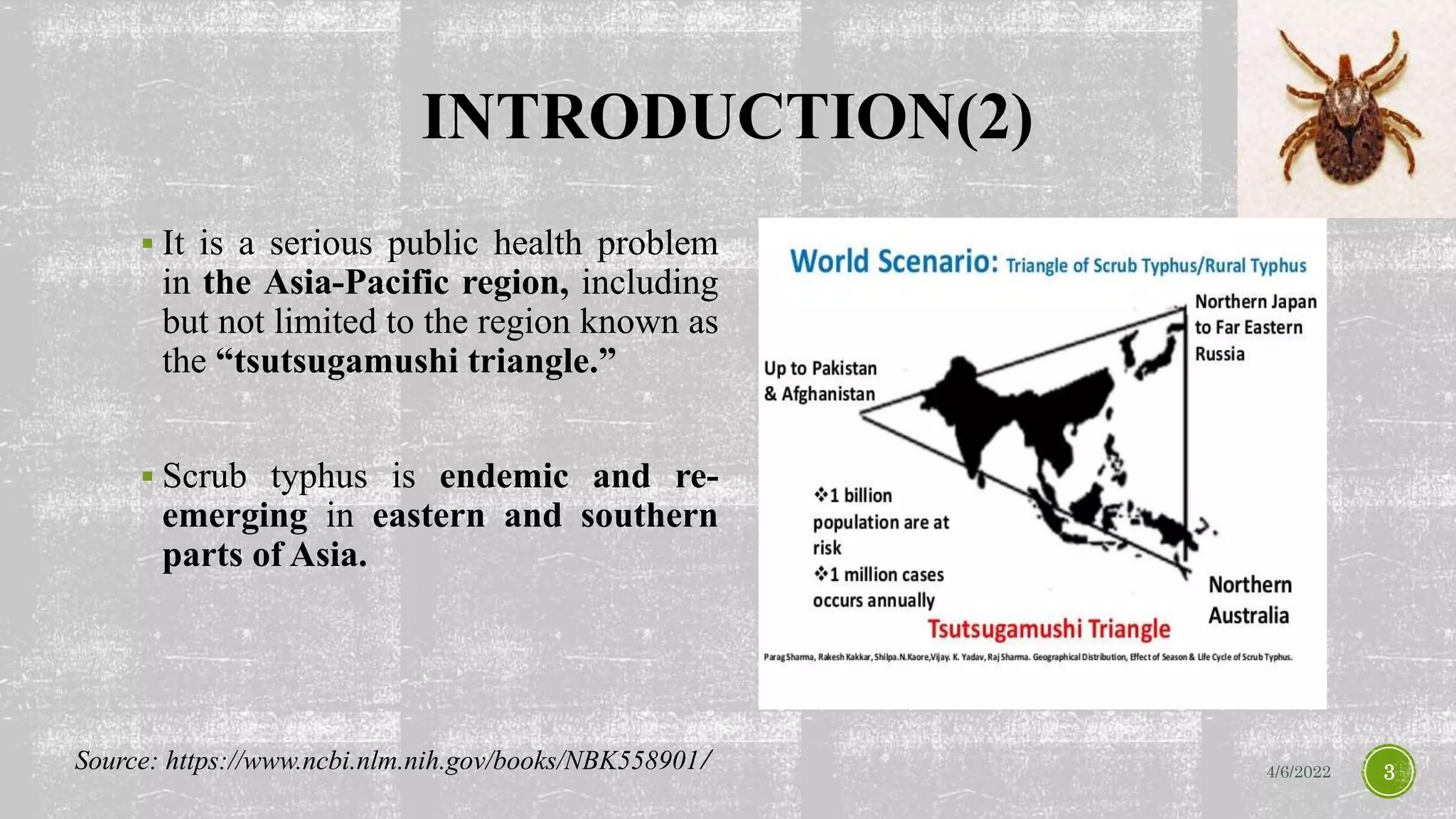
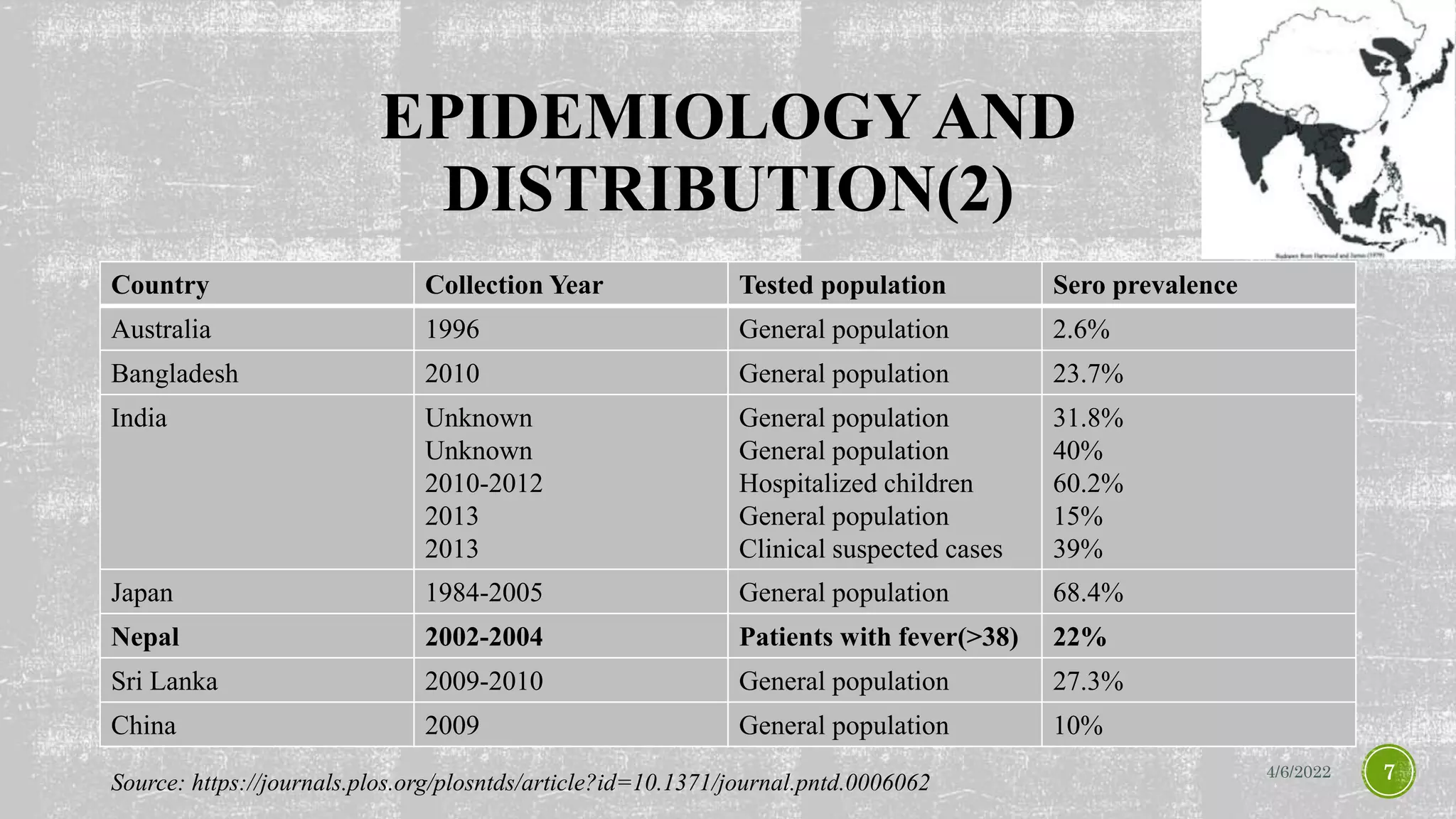
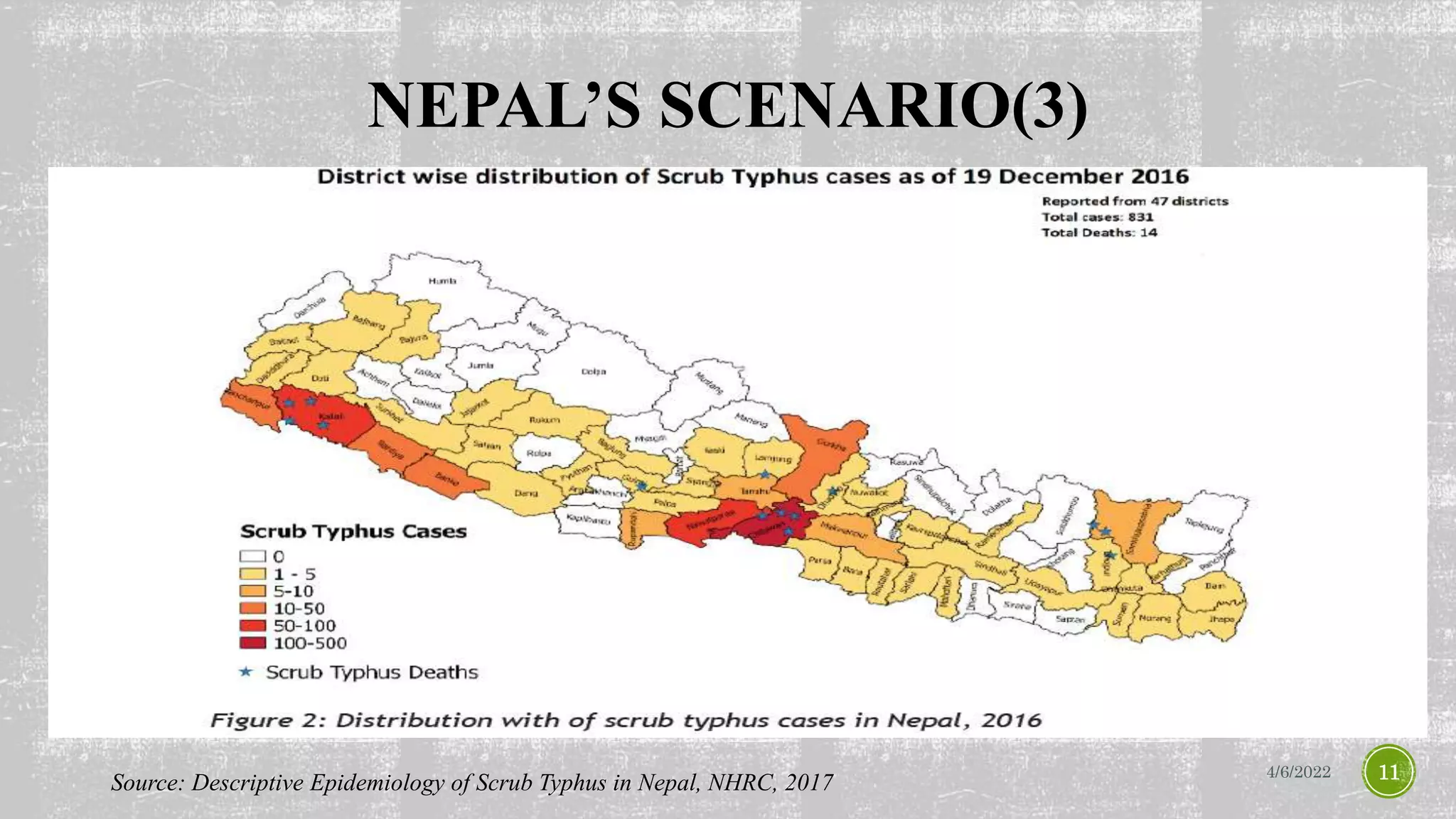
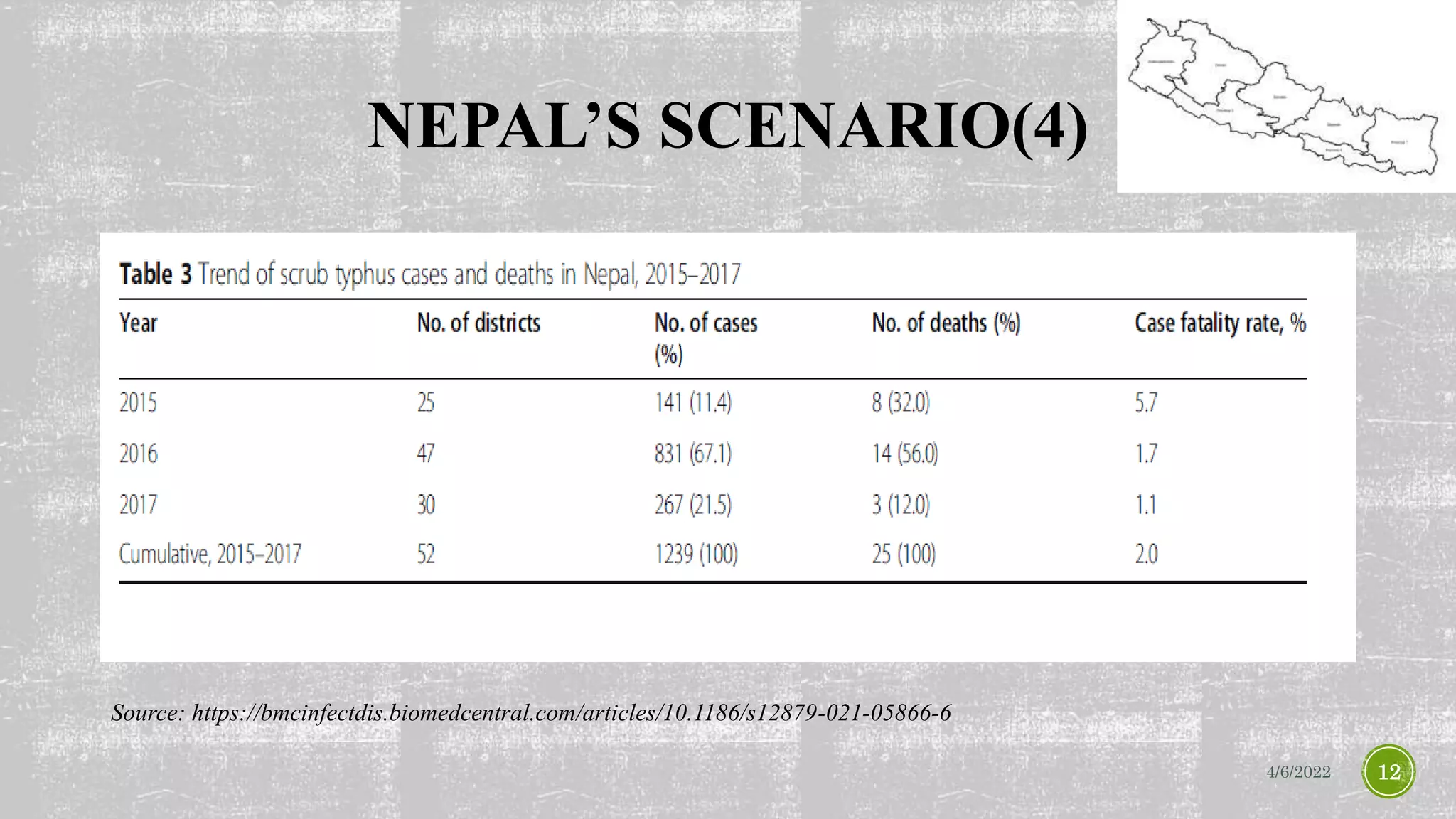
Scrub typhus, caused by the Orientia tsutsugamushi bacterium, is a significant public health issue in the Asia-Pacific region, with mortality rates varying based on treatment and infection strain. The disease has seen outbreaks in countries like Nepal since 2014, with various control measures implemented to combat its spread. Despite being treatable, scrub typhus is often under-recognized and neglected, necessitating improved awareness and public health strategies.