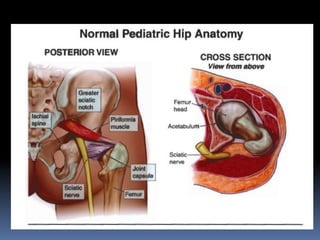
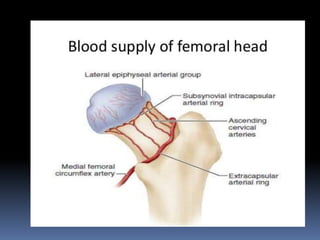
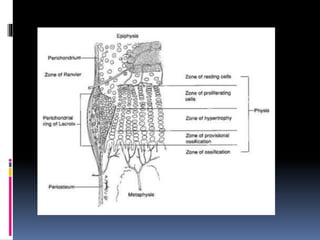
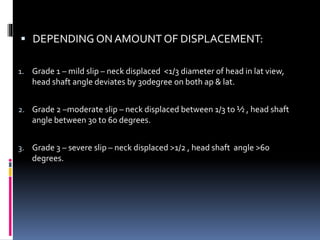
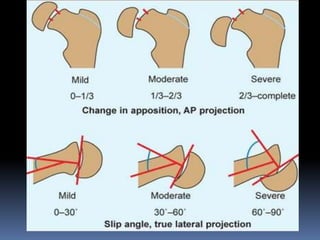
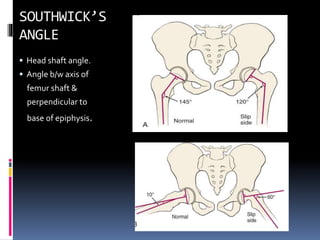
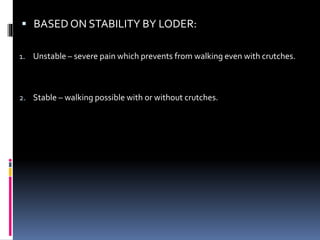
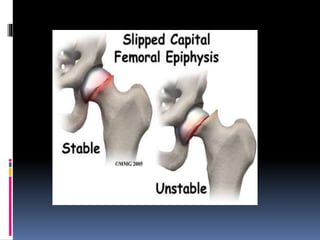
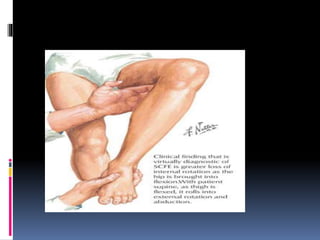
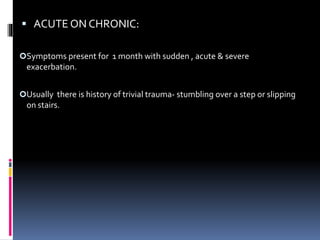
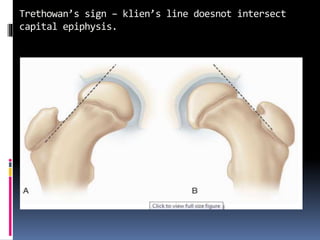
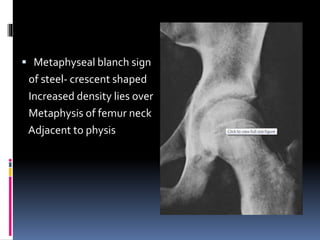
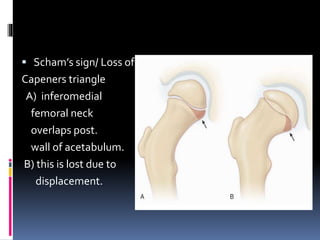
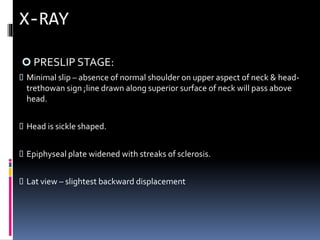
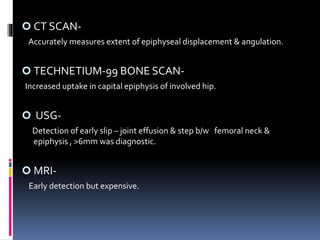
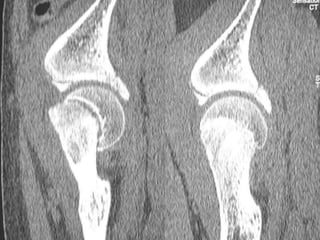
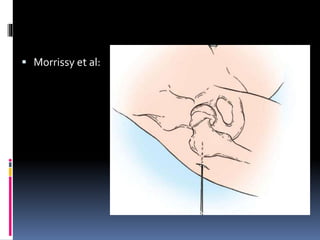
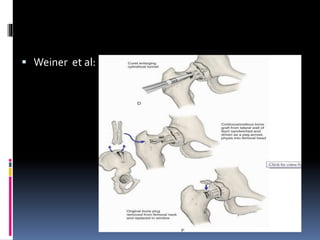
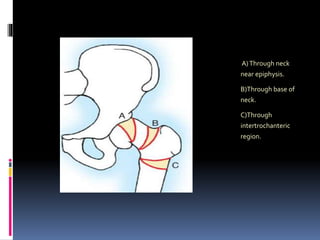
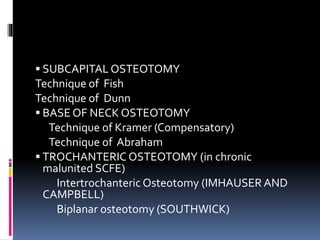
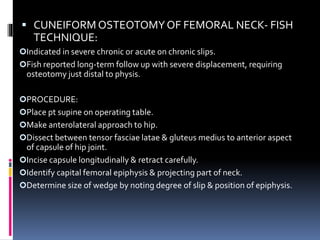
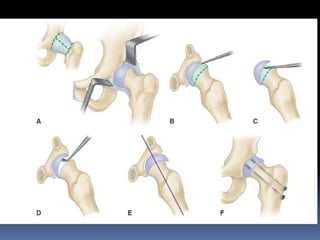
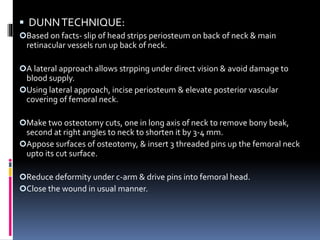
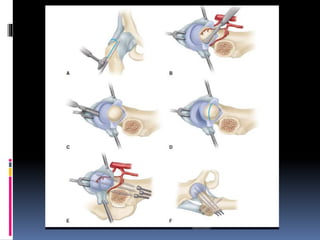
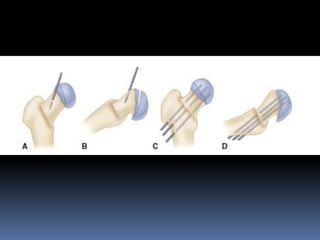
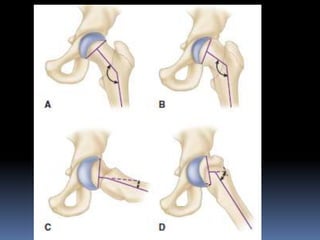
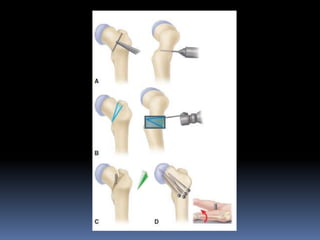
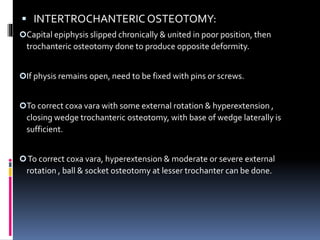
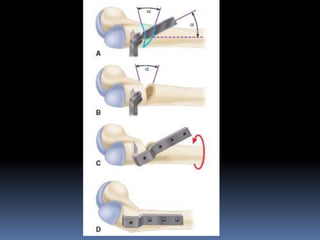
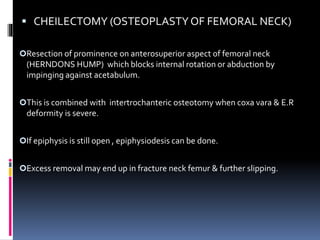
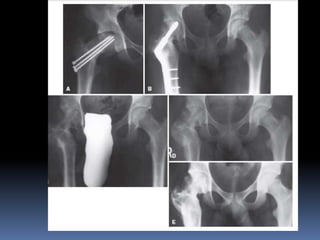
This document discusses slipped capital femoral epiphysis (SCFE), beginning with its history and definitions. It describes the anatomy and pathophysiology, presenting typical age and sex distributions. Risk factors include growth hormones, sex hormones, and trauma. Clinical presentations range from pre-slip to acute/chronic stages. Radiographic findings and grading systems are outlined. Differential diagnoses and treatment approaches like pinning, osteotomies, and epiphysiodesis are summarized. Surgical techniques like the Dunn and Kramer procedures aim to reduce displacement and prevent further slipping through fixation.